INTRODUCTION
Neuropsychological evidence suggests that children with attention deficit hyperactivity disorder (ADHD) show impairments in frontal-lobe mediated executive and self-monitoring functions (Barkley, 1997; Rubia et al., 2001b). Structural and functional neuroimaging findings suggest a dysfunction in fronto-strio-thalamo-cortical and fronto-cerebellar circuitries as the neural correlate of the disorder (Rubia & Smith, 2001). Motor timing is a poorly investigated executive function which has recently been shown to be impaired in community children with hyperactive behavior (Rubia, Taylor, Taylor, & Sergeant, 1999b). The temporal organization of behavior includes preplanning the acts that constitute purposeful behavior, deciding their temporal onset, and monitoring their time course once they have been initiated (Fuster, 1985). There is evidence that children with ADHD are impaired in these different processes of motor timing.
Evidence for Poor Motor Timing in ADHD
Behavioral and neuropsychological evidence suggests that hyperactive children show deficits in timing of behavior. ADHD children show poor "intertemporal competence," that is, poor ability to associate events which are separated by time. They live more in the present and display greater risk-taking behavior than nonhyperactive children (Barkley, 1997). This "temporal myopia" manifests itself also in reward-mediated behavior. ADHD children prefer small and immediate rewards to large but delayed ones, are less tolerant of reward delays and less reactive to punishment if it is delayed in time (Milich, Hartung, Martin, & Haigler, 1995; Schweitzer & SulzerAzaroff, 1995; Sonuga-Barke, Taylor, Sembi, & Smith, 1992). Poor performance on planning tasks, in which future events have to be taken into account, suggest poor intertemporal competence (Pennington & Ozonoff, 1996).
Apart from deficits in behavioral planning, hyperactive children have problems in motor execution. Hyperactive children are impaired in sensorimotor, paced sensorimotor, and speeded motor tasks (Carte, Nigg, & Hinshaw, 1996; Rubia et al., 1999b; Steger et al., 2001; Stevens, Stover, & Backus, 1970).
Abnormal motor timing is further suggested by the fact that the event rate has different effects on the performance of hyperactive children compared to controls (Rubia et al., 1999b). Both slow and fast event rates have been shown to have a detrimental effect on the performance of hyperactive children, suggesting that they are less able to adjust their own speed to the externally demanded pace in motor and cognitive tasks (Carte et al., 1996; Denckla, Rudel, Chapman, & Krieger, 1985; van der Meere, Vreeling, & Sergeant, 1992).
Poor timing of motor output has been related to impulsiveness, defined as a temporally inadequate, premature and erratic response style, where motor acts are executed prior to the appropriate time without consideration of future consequences. Premature responding is a typical feature in ADHD performance on most cognitive tasks (Rubia et al., 2001b), including timing paradigms such as delay tasks (Rubia et al., 1999b; Sonuga-Barke et al., 1992) and time-estimation (Barkley, Koplowitz, Anderson, & McMurray, 1997; Sonuga-Barke, Saxton, & Hall, 1998).
In a previous study, we examined poor motor timing in a group of community children with hyperactive behaviors. The hyperactive children demonstrated deficits in motor timing, but not in their temporal perception (Rubia et al., 1999b). The deficits observed in motor timing consisted of increased variability of free tapping, synchronizing, and anticipating the motor response to visual stimulation (Rubia et al., 1999b). Inconsistencies in free tapping suggest the inability to sustain a self-chosen regular pacing of motor output. Variable sensorimotor synchronization indicates difficulties in generating a stable, rhythmic response pattern that matches the visual input. A similar deficit in the consistency of sensorimotor adjustment was observed in an anticipation task; hyperactive children had difficulties emitting a consistent motor response in anticipation of a visual stimulus that appeared every 6 s.
Using functional magnetic resonance imaging (fMRI), reduced mesial prefrontal activation has been observed in adolescents with the diagnosis of ADHD during motor timing in a sensorimotor synchronization task (Rubia et al., 1999a, 2000, 2001b). It thus seems possible that abnormalities in prefrontal brain regions are related to motor timing deficits that may underlie the behavioral impulsiveness of ADHD children (Rubia, 2002).
Evidence for the Effect of Methyiphenidate on Motor Timing
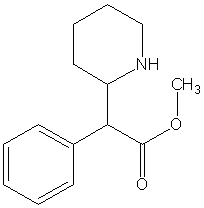
It has been suggested that dopaminergic pathways may be involved in motor timing functions in healthy adults, based on the effect of dopamine agonists and antagonists on motor timing and time perception (Meck, 1996). Stimulant medication, the most effective treatment for ADHD symptoms, has been shown to have a positive effect on motor timing functions via dopaminergic, rather than noradrenergic or serotonergic receptors (Volkow et al., 1997). Methylphenidate has been shown to increase metabolism in the dorsolateral prefrontal cortex, the cerebellum, and the basal ganglia (Volkow et al., 1997). These brain areas have been implicated in motor timing functions (Rubia et al., 1998b, 2000, 2001b) and have been shown to be morphologically and functionally compromised in ADHD (Rubia & Smith, 2001). Methylphenidate has been shown to increase activation in prefrontal brain areas and in the striatum in children with ADHD (Teicher et al., 2000; Vaidya et al., 1998). Increased dopamine transporter (DAT) availability in A DHD could be decreased with 4 weeks of methylphenidate administration (Dougherty et al., 2000; Krause, Dresel, Krause, Kung, & Tatsch, 2000).
Methylphenidate has been shown to reduce predominantly externalising dysfunctions in ADHD such as hyperactivity (Butte, Treuth, Voigt, Llorente, & Heird, 1999) and impulsive, oppositional (Schachar, Tannock, Cunningham, & Corkum, 1997), and antisocial behaviors (Smith et al., 1998). In the cognitive domain, methylphenidate has been shown to improve the executive functions of sustained attention (O'Toole, Abramowitz, Morris, & Dulcan, 1997; Pelham, Hoza, Kipp, Gnagy, & Trane, 1997), self-regulation (Berman, Douglas, & Barr, 1999), working memory (Tannock, Ickowitz, & Schachar, 1995b), cognitive flexibility (Solanto & Wender, 1989), and inhibitory control in hyperactive children (Tannock, Schachar, & Logan, 1995a). Thus, basic neuroscience research shows that there is evidence implicating dopamine in motor timing functions; clinical studies show abnormalities in both dopamine levels and motor timing functions in ADHD; and there is evidence for a positive effect of methylphenidate on motor--cognitive performance of hyperactive children.
Motor timing tasks seem therefore to be well-suited to test for an effect of methylphenidate on the dopaminergic system of ADHD children. A decline in the dopamine system during ageing has been shown to correlate with performance on finger tapping, making this task particularly suitable for indirect measurement of dopamine brain function (Volkow et al., 1998).
The Aim of This Study
The aims of this study were twofold: (I) to compare a group of clinically diagnosed children with ADHD with our previously studied community group of children with hyperactive behavior on the same battery of motor timing tasks to investigate whether a clinical sample of ADHD children would show the same deficits in motor timing as the community sample with hyperactivity and (2) to investigate the effect of methylphenidate on the timing functions of the clinically diagnosed children with ADHD in a placebo-controlled, double-blind crossover design, including a 4-week medication condition.
Although there is some evidence of poor sensorimotor functions in children with clinically diagnosed ADHD on speeded sensorimotor and neuromotor tasks (Carte et al., 1996; Denckla et al., 1985; Stevens et al., 1970), motor timing skills have never been tested previously in a systematic way in a clinical sample of ADHD children. The hypothesis of poor intertemporal competence and sensorimotor anticipation was tested using an anticipation task, that required an anticipated motor response to a repeatedly appearing visual stimulus. A free tapping task was used to test the hypothesis that ADHD children would show a fast and inconsistent response style in an unstructured task condition. Possible differences in temporal adjustment of the motor output to visual stimulation in the three groups was tested with a sensorimotor synchronization task using four different event rates. A duration discrimination task controlled for possible deficits in the perception of temporal intervals.
Although there are studies suggesting that community and clinical samples do not differ in the severity of hyperactive behavior as measured by behavioral rating scales (Woodward, Dowdney, & Taylor, 1997), in other childhood disorders, such as conduct disorder, the severity of behavioral symptoms has been shown to be significantly greater in referred compared to nonreferred samples (Gerralda & Bailey, 1988). Very few studies have compared the cognitive performance of nonreferred and referred cases of childhood disorders directly, especially ADHD. Daugherty, Quay, and Ramos (1993) did not find the same deficits on a delayed response task in a nonreferred sample of children with hyperactive behaviors that have been found in clinically referred children with ADHD. Likewise, deficits in children diagnosed with ADHD on a choice reaction time task (Sykes, Douglas, Weiss, & Minde, 1971) were not observed in community samples with hyperactive behaviors (Sykes, Douglas, & Morgenstern, 1973). Smith, Taylor, Warner-Roger s, Taylor, and Rubia (2002) found that only a clinical group of children with ADHD showed time reproduction deficits, while the community children with hyperactive behaviors were unimpaired. On the basis of these studies, we hypothesised that the clinical group with ADHD would show the same or even greater impairment than the community group with hyperactive behavior on the motor timing battery.
Based on the evidence implicating dopamine in timing functions and in the behavioral and cognitive deficits of ADHD, we investigated the effect of methylphenidate on motor timing functions in the clinical sample with ADHD. We assessed whether a single dose and 4 weeks of chronic administration of methylphenidate would show a positive effect on deficient motor timing abilities in ADHD children. The effect of stimulant medication on motor timing functions has thus far never been investigated in children with ADHD. Methylphenidate, however, has been shown to have no effect on perceptual time estimation in hyperactive children (Barkley et al., 1997). We expected, therefore, no effect on time estimation abilities in ADHD, but an improvement on the motor timing functions.
A second aim of the study was to investigate whether there would be any differences between the single dose of methylphenidate and chronic administration. Although most studies have investigated the effect of a single dose on cognitive performance in ADHD children, to our knowledge no studies have compared long-term with acute administration of methylphenidate on cognitive and motor performance.
The hypotheses were that (1) children with clinically diagnosed ADHD would show the same deficits on the motor timing tasks when compared to healthy controls as the community hyperactive group; (2) like the children with hyperactive behaviors, children with the clinical diagnosis of ADHD would show unimpaired time estimation; and (3) both the acute and the persistent dose of methylphenidate would improve motor timing abilities in the clinical group with ADHD, but would not show an effect on time estimation.
METHOD
Subjects
Thirty-five boys participated in the study. Clinical patients were 13 right-handed boys with a clinical diagnosis of ADHD (American Psychiatric Association [APA]. 1994) from the Department of Child and Adolesceni Psychiatry of the Academic Medical Center University of Amsterdam. One of the subjects was predominantly hyperactive-impulsive, one predominantly inattentive, the other eleven were combined type. DSM-IV psychopathology was assessed by a psychiatrist using clinical observation and information from parents and teachers. DSM-III-R diagnosis was assessed using the Diagnostic Interview Schedule for Children, Parent version 2.3 (DISC-P; National Institute of Mental Health [NJMH], 1992). All boys scored above the 75th percentile (T-score 58) on the Attention Problem factor score of both the Child Behavior Checklist and Teacher's Report Form (Achenbach, 1994; see Table I). No comorbid DSM-IV diagnoses were present, including specific learning disorder, oppositional defiant disorder, conduct disorder, pervasi ve developmental disorder, anxiety disorder, mood disorder or Tic disorder. Conduct disorder was not excluded from the selection criteria, but was absent in the children who completed all four testing sessions. All children were free from neurological disorders. The ADHD children had never been medicated previously with psychopharmacological substances. The children were of average intelligence quotient (IQ> 80) and aged 7-11 years. IQ was assessed with four subtests of the Revised Wechsler Intelligence Scale for Children (Vocabulary, Arithmetic, Block Design, and Picture Arrangement) shown to correlate significantly (r = .93) with the full administration of the WISC-R (Groth-Marnat, 1990; see Table I). Complete data were available from all four test sessions from 13 of the 29 children that have been tested, due to technical problems.
The baseline performance of the boys with clinical ADHD was compared to the performance data from our previous study with control boys and community boys with hyperactive behavior (see Rubia et al., 1999b). The 11 right-handed community boys with hyperactivity were selected after screening over 500 children from special educational services in The Netherlands on the basis of questionnaires administered to parents (Child Behavior Checklist; Achenbach, 1994) and teachers (Teachers Report Form; Achenbach, 1994) and were in the age range of 6-12 years (see Table I). Boys were rated at or above the 95th percentile on the "attention problems" scales on both questionnaires. Boys who scored above the cut-off for any other scale (except conduct disorder) were excluded from the study. Boys were excluded with specific reading or leaming disorders. Children who met criteria for both attention problems and conduct disorder were included, because we considered the latter to be a complication of the disorder rather than a c omorbidity (Fergusson, Horwood, & Lloyd, 1991; Taylor, Chadwick, Heptinstall, & Danckaerts, 1996). Three of the boys met criteria for both conduct disorder and ADHD.
The 11 dextral boys in the control group were in the age range of 6-12 years (mean age 9.0 +/- 1.5) and were recruited from public schools; all were rated below the 75th percentile on all syndrome scales of the Child Behavior Checklist (CBCL) and the Teacher Report Form (TRF; see Table I). The ethnic background for all children was White-caucasian with the exception of one
Afro-caribbean boy in the community sample of hyperactive children.
Medication
All children with the clinical diagnosis of ADHD participated in a double-blind, placebo-controlled, crossover design employing a single dose (0.3 mg/kg) and 4 weeks of the same dose of methylphenidate administration. The dose of 0.3 mg/kg has been chosen based on the optimal dose reported in the NIMH Collaborative Multisite Multimodal Treatment Study of children with ADHD (MTA study; Greenhill et al., 2001). Furthermore, low doses of methylphenidate, between 0.1 and 0.4 mg/kg optimally enhance ADHD children's performance on attention tasks (Tannock, Schachar, Carr, Chajczyk, & Logan, 1989; Tannock et al., 1995a, 1995b). Children received a baseline session, followed 1 week later by a test trial after a single dose of either placebo or medication (children were tested 90 mm postmedication), followed a second week later by another test trial after a single dose of either placebo or medication, which was then repeated after 4 weeks of chronic methylphenidate administration (0.3 mg/kg). Children had not received medication prior to the study.
Experimental Tasks
All paradigms were identical to a previous study (see Rubia et al., 1999b). All boys were tested on the computerized tasks (duration half an hour). The clinical group was tested four times (for the baseline, placebo, acute, and persistent medication conditions).
Free Tapping
Free tapping is a validated experimental paradigm to investigate the speed and consistency of self-produced finger tapping (Mates, 1990) and has been used in children with ADHD (Rubia et al., 1999b, 2001b; Stevens et al., 1970). The boys were required to tap a response button with their right finger 80 times, as regularly as possible, at a freely chosen rhythm. Dependent measures were tapping time and within-individual standard deviation. The tapping times reflect the preferred speed, while the variability of response reflects consistency and regularity of the freely chosen motor production time.
Synchronized Tapping (Sensorimotor Synchronization)
Participants were required to synchronize their motor response via a right-handed button-press to a visual stimulus (airplane) which appeared at a fixed event rate on a computer screen. Synchronization of finger tapping using repetitive stimuli is a validated paradigm to study sensorimotor timing mechanisms, widely used in children and adults (Piek & Skinner, 1999; Rubia et al., 1998b; 1999a, 1999b, 2000, 2001b). Good perceptual--motor integration is required in order to achieve temporal coincidence between the motor response and the sensory stimulus. The accuracy of synchronization depends on the sensory system (ability to perceive asynchrony), the motor system (ability to correct the perceived asynchrony) and the accuracy of the corresponding time-keeping mechanism in a sequence of responses (Mates, 1990). Good perceptual-motor integration is also required in order to achieve sensorimotor coincidence. Five blocks of 60 trials were administered. Interstimulus intervals (ISIs) were 700, 900, 1200, and 1800 in s, respectively. Dependent measures were synchronization times, reflecting accuracy of time estimation and intraindividual variability, reflecting the consistency of the synchronization timing.
Sensorimotor Anticipation Task
A visual stimulus (an airplane) appeared 40 times on a computer screen with a fixed ISI of 6 s. The child was instructed to monitor the intertemporal gap between the appearances of the first three airplanes and to press a response button with the right index finger in anticipation of the appearance of the fourth and subsequent airplanes. The children thus had to estimate the time interval and press the button shortly before they estimated when the stimulus would appear on the screen. The children were advised to estimate the ISI by either counting or by intuition. The task involves time estimation, sustained attention (to time), and sensorimotor timing. The continuity of stimulus appearance (no breaks between trials) imposes a high processing load on the child by requiring mental resetting after every stimulus in order to monitor the next temporal interval. Implicit feedback was given by the perception of the synchrony or asynchrony of their own button-press in relation to the appearance of the stimulus.
Dependent measures were the "anticipation times" and their within-subject variability. Anticipation time is the "response" time in anticipation of the stimulus appearance, reflecting the accuracy of time estimation, while its variability reflects the consistency of the time estimation. This task is a variant of a delayed response task which has been widely used to test motor preparation and motor timing, where a motor response has to be made in response to a stimulus appearing after a fixed interval. By instructing boys to anticipate their response to the stimulus instead of reacting to it, we intended to impose a greater load on time estimation and motor timing functions compared to the "classical" delayed response task. This task variant has been shown to activate prefrontal brain regions mediating motor-output timing functions in healthy subjects (Rubia et al., 1998b, 2000) and reduced prefrontal activation in subjects with ADHD (Rubia et al., 1999a, 2000, 2001b).
Time Discrimination Task
Time discrimination is one of the four major methods used in time estimation research (Zackay, 1990) and has previously been applied to ADHD children (Rubia et al., 1999b; Smith et al., 2002). Pairs of airplanes were presented on a screen, separated by an interval of 1 s. The first airplane was displayed for 5 s, while the second airplane was displayed for 5 or 3 s duration. The children were instructed to judge whether the length of both time intervals was identical or different by pressing the right or left response button, respectively. Decision time was 3 s; 10 trials were administered. The children were advised to estimate the durations by either counting or by guessing. Dependent measures were the number of errors, the reaction time of decision making and within-subject standard deviation of reaction time.
The four tasks were administered in the same order to all children, starting with free tapping, followed by synchronized tapping (sensorimotor synchronization), anticipation, and time discrimination tasks.
Data Analysis
Group means were compared using multiple analyses of covariance (ANCOVAs) at a = .05 to test for group differences between control boys, community boys with hyperactivity and clinically ADHD boys. IQ was covaried because significant differences emerged in IQ between the community group with hyperactivity and the clinical group with ADHD and the controls, respectively (see Table I). To analyze data across both ISI and condition in the synchronization task, data were transformed by expressing the synchronization times as a proportion of the delay (by dividing synchronization times and within-subject standard deviations by the respective time intervals). Post hoc differences were tested using two-tailed t tests (SPSS Inc, 1994). Post hoc comparisons were used for the case-control comparisons on the dependent measures. For the post hoc comparisons, significance levels were adjusted to account for multiple comparisons using the modified Bonferroni correction of p lower than [alpha]/3 = .017 for the group compariso ns. For the medication comparisons, planned t tests were conducted at a = .05 to test for a difference between single dose versus placebo, multiple dose versus placebo, and single versus multiple dose. Where there were unequal variances, t and p values were adjusted.
RESULTS
IQ
A one-way ANOVA showed a significant group effect on the prorated full-scale IQ. Post hoc comparison showed that both the clinical as well as the community group with hyperactivity had significantly lower IQ scores than controls (see Table I; comparison clinical group vs. controls: t = 3.29, p < .003; comparison community group with hyperactivity vs. controls: t 3.84, p < .001). The two hyperactive groups did not differ in their IQ scores (t = -0.14, p < .88).
Although there was no significant correlation between any of the performance measures and IQ, analysis of covariance was conducted on all data. There was no evidence of an interaction between IQ and group for any of the dependent measures and the ANCOVA model was considered adequate to adjust for group effects.
TRF and CBCL Measures
ANOVA showed a significant group effect for both the CBCL total score (F = 26; df = 2, 32; p < .00) and the TRF total score (F = 31.l; df = 2,32;p <.00). Post hoc comparisons showed that the two groups with hyperactivity did not differ from each other on any scores on either the TRF or the CBCL subscales; both groups scored significantly higher on these scales compared to controls (see Table I).
Motor Timing Tasks
Free Tapping
ANCOVA showed no group differences in the speed of free tapping. A significant group effect was found for the within-subject variability of free tapping (F = 6.0; df = 2,32; p = .006), which was significant for the community group with hyperactive behavior compared to controls, but did not survive the Bonferroni correction for the clinical group with ADHD. The two groups with hyperactivity did not differ from each other on this measure (see Table II).
Synchronized Tapping
To compare the data across the different temporal intervals, the synchronization times were transformed into percentage values by dividing the synchronization times and standard deviations by the respective temporal intervals (700, 900, 1200, and 1800 ins, respectively). All subjects anticipated the respective temporal intervals, in line with normative characteristics of synchronized tapping (Mates, Radil, & Poeppel, 1992). There was no overall group effect for mean synchronization times and no interaction of group with time interval for reaction times or variability of reaction times (see Table II). Significant group differences were observed, however, for the variability in synchronization times (F = 10.3, df = 2, 32, p < .000). Post hoc comparison showed that both the clinical and the community groups with hyperactivity were significantly more inconsistent in sensorimotor timing compared with controls, but did not differ from one other for this measure (see Table II).
Anticipation Task
Responses which were not anticipatory to the visual stimulus, but made 300-700 ms after stimulus appearance, were excluded from the analysis and considered as impulsive errors (see Rubia et al., 1999b). One boy was excluded from this task due to failing to comply with instructions. ANCOVA showed that there were no group differences on anticipation times, but on within-subject standard deviation of these anticipation times (F = 6.7; df = 2, 31; p = .004). Post hoc comparisons showed that both the clinical and the community groups with hyperactivity had significantly increased within-subject variability in sensorimotor anticipation time compared to control subjects, but did not differ from each other (see Table II). Group differences were also observed for the number of impulsive errors (F = 3.6; df = 2, 31; p = .017); both the clinical and the community groups with hyperactivity made significantly more impulsive errors compared to controls, but did not differ from each other in the number of impulsive errors ( see Table II).
Time Discrimination Task
ANCOVA showed significant group differences for errors (F = 4.7; df = 2,32; p = .017) and within-subject variability of decision time (F = 4.9; df = 2, 32; p = .014), but not in decision times. Post hoc comparisons showed that the clinical group made significantly more time estimation errors compared to the control group. The community group with hyperactivity was unimpaired in time estimation. The hyperactive groups, however, did not differ from each other in the number of time estimation errors. Both the clinical and the community groups with hyperactivity were significantly more variable in decision times compared to controls and did not differ from each other in this measure (see Table II).
Medication Effects
Free Tapping
There was no effect of any of the medication conditions on the speed or the variability of free tapping (see Table III).
Synchronized Tapping
There was no interaction effect of ISI by condition for either speed or variability. Paired t tests showed that the persistent administration of methyiphenidate accelerated the synchronization times. The multiple dose of methyiphenidate also significantly reduced the variability of synchronized tapping compared to both the placebo and the acute administration conditions (see Table III).
Anticipation Task
There was no effect of any of the medication conditions on mean anticipation times. However, there was a significant effect for the persistent, but not the acute administration of methylphenidate in reducing both the variability of anticipation and the number of impulsive errors. Acute and persistent medication conditions, however, did not significantly differ from each other on these two measures (see Table III).
Discrimination Task
There were no effects of any of the medication conditions on number of time estimation errors, decision times, or variability in decision times (see Table III).
Power of the Study
To ascertain that our study had enough power to detect potential effects of methylphenidate, we estimated expected effect size, based on previous studies of the effect of methylphenidate on the performance of children with ADHD on a go-no-go (Trommer, Hoeppner, & Zecker, 1991), a reward (Wilkison, Kircher, McMahon, & Sloane, 1995), and a continuous performance task (Verbaten et al., 1994). These effect sizes ranged from 0.66 to 1.48. The power to detect these effect sizes with n = 13 ranges from 0.72 to 0.96, the lowest of which approaches an acceptable level according to Maddock, Rossi, and Joseph (2001).
There were no apparent outliers in our dataset that could have disproportionately influenced the group statistics. In the medication study, out of 13 boys, at least 10 boys showed improvement on the performance measures that were statistically significant in the group statistics.
DISCUSSION
Differences Between the Clinical and the Community Groups With Hyperactivity
Our previous findings of motor timing inconsistencies in a group of community children with hyperactive behavior were replicated in a clinical sample of children diagnosed with ADHD. In our previous study we found that the community group with hyperactive behavior was significantly more inconsistent in free tapping and in visuomotor anticipation and synchronization, but did not show deficits in time perception (Rubia et al., 1999b). In this study, the clinical group shared similarities with the community group with hyperactivity with increased within-subject variability on most motor timing tasks compared to controls: they showed increased variability in visuomotor synchronization, visuomotor anticipation, and in decision latency for time discrimination. However, in the free tapping task, the clinical group showed only a marginal impairment in within-subject variability with a medium to large effect size, which did not survive the Bonferroni correction. Both hyperactive groups showed more impulsive errors on the anticipation task. Thus, with the exception of the free tapping task, we could confirm the hypothesis that the clinical group with ADHD is as impaired in motor timing as the community group with hyperactive behavior.
We could not confirm the hypothesis that the clinical group with ADHD was more impaired than the community group with hyperactive behavior. The two hyperactive groups did not differ from each other on any of the dependent measures. However, on the time discrimination task, only the clinical group and not the community group was impaired compared to controls. On this task, the clinical group made more errors than controls, while the community children with hyperactivity were unimpaired in their time discrimination abilities.
The finding of a deficit in ADHD at the perceptual level is unusual, since most deficits have been observed at the executive level of performance (Barkley, 1997). This finding, however, is in line with a recent study of Smith et al. (2002), where a clinical group with ADHD was impaired in time discrimination in the range of milliseconds, but this deficit was not found in a community sample with hyperactive behavior (Smith, 2002). This effect may reflect symptom severity, since time estimation abilities of the community group with hyperactivity lay between the normal and the clinical range. Time estimation abilities are a controversial subject in ADHD research. Some studies found shorter time production and reproduction in seconds in ADHD children (Barkley et al., 1997; Sonuga-Barke et al., 1998); other studies, using passive time estimation of several seconds, did not find time perception deficits (Rubia et al., 1999b; Smith et al., 2002), but reported differences in time discrimination in the range of millis econds (Smith et al., 2002). Deficits in time production or reproduction, as opposed to passive time estimation, where no motor response is required, can be confounded by motor output related deficits such as poor motor timing, delay aversion, poor inhibitory control, prepotent response style, or even poor working memory in the case of reproduction (Rubia et al., 1999b; Rubia, Schuri, von Cramon, & Poeppel, 1997). This study is the first to show deficits in children with ADHD in discrimination of intervals in the range of seconds.
The finding of increased numbers of premature, impulsive responses in the anticipation task is in line with findings of a premature response style in children with ADHD on many cognitive tasks (Rubia et al., 2001b). Impulsive, premature responding has been observed especially in timing tasks, where waiting is required (Smith et al., 2002; Sonuga-Barke et al., 1998) and has been associated with deficient inhibitory control mechanisms (Rubia, Oosterlaan, Sergeant, Brandeis, & van Leeuwen, 1998a). Poor response control has been measured in other contexts such as stop or go/no-go task performance (Rubia et al., 1998a, 2001b; Schachar, Tannock, Marriott, & Logan, 1995), and the premature response errors observed here are likely to reflect the inability to inhibit a prepotent response.
Both the clinical and the community groups with hyperactivity were impaired in their within-subject variability in the synchronization and anticipation tasks. A similar finding of increased inconsistency of sensonmotor timing of an interval of 300 ms has been reported in a previous study (Vongher et al., 2001). The finding of increased variability in sensorimotor adjustment rather than in free tapping suggests that the temporal adjustment to externally given time points presents more difficulties to hyperactive children than does maintaining a consistent, freely adopted rhythm in free tapping. To adjust to externally determined temporal rhythms is more effortful than to maintain a self-imposed time rhythm and may reflect the increased problems that children with ADHD have with effortful as opposed to automatic performance (Carte et al., 1996; Robaey, Breton, Dugas, & Renault, 1992). The fact that variability rather than speed of synchronization and anticipation was impaired suggests that the deficit lies in f ine-temporal control of the motor output adjustment rather than in a general inability to adjust to external temporal requirements.
Increased variability in reaction times has been found consistently across a wide range of cognitive tasks in children with ADHD and may reflect problems with sustaining attention (Leth-Steensen, Elbaz, & Douglas, 2000; Rubia et al., 1999b). It is thus also possible that the more variable response style in motor timing tasks is related to poor attention allocation, that manifests itself also in the timing domain.
It has been shown that children with dyslexia and comorbid ADHD show reduced rhythmicity in speeded motor timing (Denckla et al., 1985), and children with dyslexia alone show deficits in synchronized tapping tasks (Waber et al., 2000), and fine-temporal discrimination (Nicolson, Fawcett, & Dean, 1995). In these two samples, there was no comorbidity for dyslexia or general learning disability. This suggests that poor temporal adjustment of the motor output and poor time discrimination in children with dyslexia and in children with ADHD may be caused by common mechanisms that are deficient in both disorders.
Medication Effect
The persistent use of methylphenidate had a positive effect on the increased variability in the externally paced motor timing tasks. It decreased the variability of seasorimotor anticipation and of sensorimotor synchronizadon. Persistent administration of methylphenidate also increased the speed of synchronization and reduced the number of impulsive errors in the anticipation task. It had, however, no effect on time perception. The acute dose of methylphenidate had no effect on either motor timing or time perception. It appears, therefore, that only persistent administration of methylphenidate has a positive effect on consistency of motor output timing but not on perceptual timing abilities. The lack of effect of methylphenidate on perceptual time estimation in ADHD has been found in a previous study (Barkley et al., 1997).
It is possible that methylphenidate improves output related abilities rather than perceptual information processing; it reduces externalizing, rather than internalizing dysfunctions at a behavioral level (Butte et al., 1999; Schachar et al., 1997) and executive, rather than perceptive functions in the cognitive domain (Berman et al. 1999; O'Toole et al., 1997; Pelham et al., 1997; Tannock et al., 1995a, 1995b). A role of methylphenidate in improving output rather than input related functions would be in line with its attributed effect on the dopaminergic system (Volkow et al., 1998), which has been related primarily to motor and motivational control functions (Le Moal, 1995).
The positive effect of methylphenidate on within subject consistency of motor timing is interesting; methylphenidate has been shown to decrease within subject variability of response in other cognitive domains such as response inhibition (Tannock et al., 1995 a, 1995b), selective attention (Kiorman et al., 1991; Thurston, Sobol, Swanson, & Kinsbourne, 1991), and sustained attention (Sonneville et al., 1991).
In this study only the persistent use of methylphenidate, however, improved variability of motor timing, while the single dose was not more effective than placebo. This is not in line with previous findings of a positive effect of acute administration of methylphenidate on cognitive functions such as inhibitory control, sustained attention, and working memory (O'Toole et al., 1997; Tannock et al., 1995a, 1995b, 1989), and within-subject consistency of these functions (see above). It is unlikely that a practice effect has accounted for the findings, since practice effects should have been stronger between the first, second, and third time of testing, which were only 1 week apart, rather than after 4 weeks. It is possible that a replication using larger samples, thereby increasing statistical power, might detect an effect of an acute dose of methylphenidate on motor timing consistencies. It is, on the other hand, conceivable that only the persistent administration of methylphenidate over longer time periods leads to the type of improvements such as the ones found in this study: namely increased stability and regularity of temporal motor response. To our knowledge there are no studies that, like this one, have compared acute with long-term administration of methylphenidate on motor-cognitive task performance. A study in rats showed that long-term, but not acute administration of methylphenidate attenuated presynaptic striatal dopamine function (Sproson, Chantrey, Hollis, Marsden, & Fone, 2001). A change in presynaptic dopamine function achieved with long-term treatment may be responsible for the effects observed on motor timing stability.
It is possible that other neurotransmitters are involved in the still relatively unknown psychopharmacology of stimulant medication. Evidence exists that the noradrenergic (Biederman & Spencer, 1999; Solanto, 1998; Spivak et al., 2001) and the serotonergic systems are implicated (Gainetdinov et al., 1999; Oades, 2000) in both ADHD symptoms and short-term and long-term psychopharmacological effects of methylphenidate.
Within-individual variability of response is a common finding in children with ADHD on most motor and cognitive functions, and presumably reflects deficits in response regulation and attention allocation (Leth-Steensen et al., 2000; Rubia et al., 1999b). The improvement with methylphenidate on precision of motor timing could be caused by a positive effect on networks mediating executive attention. An important structure mediating motor attention is the anterior cingulate gyrus (Rubia et al., 1998b, 2001a), which has been found to be underactivated in functional magnetic resonance studies in adolescents with ADHD during motor timing functions (Rubia et al., 1999a, 2000, 2001b). Apart from the anterior cmgulate, the dorsolateral and inferior prefrontal cortices (Rubia et al., 1998b, 2000, 2001b) and the basal ganglia (Ivry, 1996) have been involved in motor timing functions. Methylphenidate could have a positive effect on motor timing functions in ADHD through its demonstrated effect on frontal and striatal bra in activation (Teicher et al., 2000; Vaidya et al., 1998).
Limitations
We are aware that the small sample size of our study imposes limitations on the interpretation of the negative findings, which will have to be confirmed by replication with larger samples. Particularly the controversial finding of time discrimination deficits in the clinical ADHD children in the seconds' range will need to be replicated using larger sample sizes. On the other hand, several of the trends and the findings that did not survive Bonferroni-corrected p values might have been stronger with a larger sample size.
The negative effect of the single dose of methylphenidate on motor timing was unexpected, considering the positive effect of single doses on other cognitive functions (O'Toole et al., 1997; Tannock et al., 1989, 1995a, 1995b). Replication in larger sample sizes are needed to corroborate this negative finding.
The small sample size is also vulnerable to confounds from single extreme cases. We did not, however, observe extreme outliers and in the medication condition the vast majority of boys improved with the long-term methylphenidate administration in those parameters where we found a significant group effect.
Another limitation of the study is the generalizability of these findings to the general population of ADHD children. Comorbidity with conduct disorder, dyslexia, and learning deficits is common in ADHD. In this study it was our aim to avoid comorbidity with other psychiatric disorders to investigate the effect of both motor timing functions and the effect of methylphenidate on these functions on a group of children with relatively "pure" ADHD symptoms. It is, on one hand, a strength of the study that the observed findings are not confounded by comorbid psychiatric conditions. On the other hand, it imposes limitations to the extent to which the findings are applicable to the more common cases of highly comorbid ADHD.
There was a significant difference in IQ between the community and the clinical group with hyperactivity and control children and we have adjusted for it by covarying IQ. It is debatable whether an ANCOVA with IQ as a covariate is appropriate in case-control studies, since IQ cannot be seen as independent from a nonrandom group assignment (Miller & Chapman, 2001). We consider, however, that the model is adequate, since there was no interaction effect between IQ and group for any of the performance measures. Furthermore, we did not find a significant main effect whether or not IQ was covaried.
A further limitation of the study is that only one dose of 0.3 mg/kg has been tested. It would be of interest to investigate different dosages of methylphenidate on consistency of motor timing and determine potential linear or U-shaped functions. Follow-up studies are clearly needed using larger sample sizes and varying dosages of methylphenidate to replicate and extend the findings reported here.
CONCLUSIONS
In conclusion, a clinical and a community group of children with hyperactive symptoms showed increased within-subject variability on several measures of motor timing, such as, sensorimotor synchronization and anticipation. Only the clinical group showed deficits in time discrimination. The persistent administration of methylphenidate in the clinical group with ADHD improved consistency on the externally paced motor timing tasks, but had no effect on time perception. This study extends, therefore, the therapeutic effect of methylphenidate on behavioral and executive functions to the domain of motor timing.
ACKNOWLEDGMENTS
Dr Rubia was supported by a fellowship of the European Community and Dr Anna Smith was supported by the Wellcome Trust.
Received December 3, 2001; revision received October 13, 2002; accepted October 13, 2002
REFERENCES
Achenbach, T. (1994). Manual for the child behavior checklist/4-18 and 1991 profile. Burlington: University of Vermont.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
Barkley, R. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121, 65-94.
Barkley, R. A., Koplowitz, S., Anderson, T., & McMurray, M. B. (1997). Sense of time in children with ADHD: Effects of duration, distraction, and stimulant medication. Journal of International Neuropsychological Society, 3, 359-369.
Berman, T., Douglas, V. I., & Barr, R. G. (1999). Effects of methylphenidate on complex cognitive processing in attention-deficit hyperactivity disorder. Journal of Abnormal Psychology, 108, 90-105.
Biederman, J., & Spencer, T. (1999). Attention-deficit/hyperactivity disorder (ADHD) as a noradrenergic disorder, Biological Psychiatry, 46, 1234-1242.
Butte, N., Treuth, M., Voigt, R., Llorente, A., & Heird, W. (1999). Stimulant medications decrease energy expenditure and physical activity in children with attention deficit/hyperactivity disorder. Journal of Pediatrics, 135, 203-207.
Carte, E. T., Nigg, J. T., & Hinshaw, S. P. (1996). Neuropsychological functioning, motor speed, and language processing in boys with and without ADHD. Journal of Abnormal Child Psychology, 24, 481-498.
Daugherty, T. K., Quay, H. C., & Ramos, L. (1993). Response perseveration, inhibitory control, and central dopaminergic activity in childhood behavior disorders. Journal of Genetic Psychology, 154, 177-188.
Deackla, M. B., Rudel, R. G., Chapman, C., & Krieger, J. (1985). Motor proficiency in dyslexic children with and without attentional disorders. Archives of Neurology, 42, 228-231.
Dougherty, D., Bonab, A., Spencer, T., Rauch, S., Madras, B., & Fischman, A. (2000). Dopamine-transporter density in patients with ADHD-Reply. Lancet, 355, 1461-1462.
Fergusson, D, M., Horwood, L. J., & Lloyd, M. (1991). Confirmatory factor models of attention and conduct disorder. Journal of Child Psychology and Psychiatry, 32, 257-274.
Foster, J. M. (1985). Temporal organization of behavior. Human Neurobiology, 4, 57-60.
Gainetdinov, R., Wetsel, W., Jones, S., Levin, E., Jaber, M., & Caron, M. (1999). Role of serotonin in the paradoxical calming effect of psychostimulants on hyperactivity. Science, 283, 397-400.
Gerralda, M. E., & Bailey, D. (1988). Child and family factors associated with referral to child psychiatrists. British Journal of Psychology, 9, 213-227.
Greenhill, L. L., Swanson, J. M., Vitiello, B. V., Davies, M., Clevenger, W., Wu, M., et al. (2001). Impairment and deportment responses to different methylphenidate doses in children with ADHD: The MTA titration trial. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 180-187.
Groth-Marnat, G. (1990). Handbook of psychological assessment: The Wechsler intelligence scales (2nd ed., Vol. 5). New York: Wiley.
Ivry, R. B. (1996). The representation of temporal information in perception and motor control. Current Opinion in Neurobiology, 6, 851-857.
Klorman, R., Brumaghim, J. T., Fitzpatrick, P. A., & Borgstedt, A. D. (1991). Methylphenidate speeds evaluation processes of attention deficit disorder adolescents during a Continuous Performance-Test. Journal of Abnormal Child Psychology, 19, 263-283.
Krause, K.-H., Dresel, S., Krause, J., Kung, H., & Tatsch, K. (2000). Incrased striatal dopamine transporter in adult patients with attention deficit hyperactivity disorder: Effects of methylphenidate as measured by single photon emission computed tomography. Neuroscience Letters, 285, 107-110.
Le Moal, A. (1995). Mesocorticolimbic dopaminergic neurons: Functional and regulatory roles. In F. Bloom & D. J. Kupfer (Eds.), Psychopharmacology: The fourth generation of progress (pp. 283- 294). New York: Raven Press. An Official Publication of the American College of Neuropsychopharmacology.
Leth-Steensen, C., Elbaz, Z. K., & Douglas, V.I. (2000). Mean response times, variability and skew in the responding of ADHD children: A response time distributional approach. Acta Psychologica, 104, 167-190.
Maddock, J. E., Rossi, J. S., & Joseph, S. (2001). Statistical power of articles published in three health-psychology related journals. Health Psychology, 20, 76-78.
Mates, J. (1990). A system of personal computer control programs for tapping experiments. Computer Methods and Programs in Biomedicine, 33, 43-48.
Mates, J., Radii, T., & Poeppel, B. (1992). Cooperative tapping: Time control under different feedback conditions. Perception and Psychophysics, 52, 691-704.
Meck, W. (1996). Neuropharmacology of timing and time perception. Cognitive Brain Research, 3, 227-242.
Milich, R., Hartung, C. M., Martin, C. A., & Haigler, E. D. (1995). Disinhibition and underlying processes in hyperactive and aggressive adolescents. In D. K. Routh (Ed.), Disruptive behavior disorder in childhood: Essays honoring Herbert C. Quay (pp. 109-139). New York: Plenum.
Miller, G. A., & Chapman, J. P. (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110, 40-48.
National Institute of Mental Health (NIMH). (1992). Diagnostic interview Schedule for Children (DISC) Version 2.3. New York: New York Psychiatric Institute, Division of Child and Adolescent Psychiatry.
Nicolson, R. I. Fawcett, A. J., & Dean, P. (1995). Time estimation deficits in developmental dyslexia: Evidence of cerebellar involvement. Proceedings of the Royal Society London: Brain and Biological Science, 259, 437.
Oades, R. (2000). Differential measures of "sustained attention" in children with attention-deficit/hyperactivity or tic disorders: Relations to monoamine metabolism. Psychiatry Research, 93, 165-178.
O'Toole, K., Abramowitz, A., Morris, R., & Dulcan, M. (1997). Effects of methylphenidate on attention and nonverbal learning in children with attention-deficit hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 531-538.
Pelham, W., Hoza, B., Kipp, H., Gnagy, E., & Trane, S. (1997). Effects of methylphenidate and expectancy of ADHD children's performance, self-evaluations, persistence, and attributions on a cognitive task. Experimental and Clinical Psychopharmacology, 5, 3-13.
Pennington, B. F., & Ozonoff, S. (1996). Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry, 37, 51-87.
Piek, J. P., & Skinner, R. A. (1999). Timing and force control during a sequential tapping task in children with and without motor coordination problems. Journal of the International Neuropsychological Society, 5, 320-329.
Robaey P., Breton, F., Dugas, M., & Renault, B. (1992). An event-related study of controlled and automatic processes in 6-8-year-old boys with attention deficit hyperactivity disorder. Elect roencep holography and Clinical Neurophysiology, 82, 330-340.
Rubia, K. (2002). The dynamic approach to neurodevelopmental psychiatric disorders: Use of IMRI combined with neuropsychology to elucidate the dynamics of psychiatric disorders, exemplified in ADHD and schizophrenia. Behavioral Brain Research, 130, 47-56.
Rubia, K., Oosterlaan, J., Sergeant, J. A., Brandeis, D., & van Leeuwen, T. (1998a). Inhibitory dysfunction in hyperactive boys. Behavioral Brain Research, 94, 25-32.
Rubia, K., Overmeyer, S., Taylor, E., Brammer, M., Williams, S., Simmons, A., et al. (1998b). Prefrontal involvement in "temporal bridging" and timing movement. Neuropsychologia, 36, 1283- 1293.
Rubia, K., Overmeyer, S., Taylor, E., Brammer, M., Williams, S., Simmons, A., et al. (1999a). Hypofrontality in attention deficit hyperactivity disorder during higher order motor control: A study with fMRI. American Journal of Psychiatry, 156, 891-896.
Rubia, K., Overmeyer, S., Taylor, B., Brammer, M., Williams, S. C. R., Simmons, A., et al. (2000). Functional frontalisation with age: Mapping neurodevelopmental trajectories with fMPI. Neuroscience and Biobehavioral Reviews, 24, 13-19.
Rubia, K., Russell, T., Overmeyer, S., Branuner, M. J., Bullmore, B. T., Sharma, T., et al. (2001a). Mapping motor inhibition: Conjunctive brain activations across different versions of go/no-go and stop tasks. Neurolmage, 13, 250-261.
Rubia, K., Schuri, U., von Cramon, D., & Foeppel, E. (1997). Time estimation as a neuronal network property: A lesion study. NeuroReport, 8, 1273-1276.
Rubia, K., & Smith, A. (2001). Attention deficit-hyperactivity disorder: current findings and treatment. Current Opinion in Psychiatry, 4, 309-316.
Rubia, K., Taylor, E., Smith, A., Oksanen, H., Overmeyer, S., & Newman, S. (2001b). Neuropsychological analyses of impulsiveness in childhood hyperactivity. British Journal of Psychiatry, 179, 138-143.
Rubia, K., Taylor, A., Taylor, E., & Sergeant, J. (1999b). Synchronization, anticipation, and consistency in motor timing of children with dimensionally defined attention deficit hyperactivity behavior. Perceptual and Motor Skills, 89, 1237-1258.
Schachar, R., Tannock, R., Cunningham, C., & Corkum, P. (1997). Behavioral, situational, and temporal effects of treatment of ADHD with methylphenidate. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 754-763.
Schachar, R., Tannock, R., Marriot, M., & Logan, G. (1995). Deficient inhibitory control in attention deficit hyperactivity disorder. Journal of Abnormal Child Psychology, 23, 411-437.
Schweitzer, J. B., & Sulzer-Azaroff, B. (1995). Self-control in boys with attention-deficit-hyperactivity-disorder: Effects of added stimulation and time. Journal of Child Psychology and Psychiatry, 36, 671-686.
Smith, A. (2002). Time estimation and discrimination in children with hyperactivity. Doctoral dissertation, University of London, London.
Smith, B., Pelham, W., Evans, S., Gnagy, E., Molina, B., Bukstein, O., et al. (1998). Dosage effects of methylphenidate on the social behavior of adolescents diagnosed with attention-deficit hyperactivity disorder. Experimental and Clinical Psychopharmacology, 6,187-204.
Smith, A., Taylor, E., Warner-Rogers, J., Taylor, A., & Rubia, K. (2002). Evidence for a time perception deficit in children with ADHD. Journal of Child and Adolescent Psychiatry, 43, 529-542.
Solanto, M. V. (1998). Neuropsychopharmacological mechanisms of stimulant drug action in attention-deficit hyperactivity disorder: A review and integration. Behavioral Brain Research, 94, 127-152.
Solanto, M. V., & Wender, E. H. (1989). Does methylphenidate constrict cognitive-functioning? Journal of the American Academy of Child and Adolescent Psychiatry, 28, 897-902.
Sonneville, L. M. J., Njiokiktjien, C., & Hilhorst, R. C. (1991). Methylphenidate-induced changes in ADHD information processing. Journal of Child Psychology and Psychiatry, 32, 285-295.
Sonuga-Barke, E., Saxton, T., & Hall, M. (1998). The role of interval underestimation in hyperactive children's failure to suppress responses over time. Behavioral Brain Research, 94, 45-50.
Sonuga-Barke, E.J.S., Taylor, E., Sembi, S., & Smith, J. (1992). Hyperactivity and delay aversion--I. The effect of delay on choice. Journal of Child Psychology and Psychiatry, 33, 387-398.
Spivak, B., Vered, Y., Yoran-Hegesh, R., Averbuch, E., Vinokurow, S., Weizman, A., et al. (2001), The influence of three months of methylphenidate treatment on platelet-poor plasma biogenic amine levels in boys with attention deficit hyperactivity disorder. Human Psychopharmacology--Clinical and Experimental, 16, 333-337.
Sproson, B. J., Chantrey, J., Hollis, C., Marsden, C. A., & Fone, K. C. F. (2001). Effect of methylphenidate administration on presynaptic dopamine and behavior in young adult rats. Journal of Psychopharmacology, 15, 67-75.
SPSS Inc. (1994). SPSS for Windows V 6.1 (Version 6.1). Chicago, IL: Author.
Steger, J., Imhof, G., Coutts, E., Gundelfinger, R., Steinhausen, E.C., & Brandeis, D. (2001) Attentional and neuromotor deficits in ADHD. Developmental Medicine and Child Neurology, 43, 172-179.
Stevens, D. A., Stover, C. E., & Backus, J. T. (1970). The hyperkinetic child: Effect of incentives on the speed of rapid tapping. Journal of Consulting and Clinical Psychology, 34, 56-59.
Sykes, D. H., Douglas, V. I., & Morgenstern, G. (1973). Sustained attention in hyperactive children. Journal of Child Psychology and Psychiatry, 14, 213-220.
Sykes, D. H., Douglas, V.I., Weiss, G., & Minde, K. K. (1971). Attention in hyperactive children and the effect of methylphenidate (ritalin). Journal of Child Psychology and Psychiatry, 12, 129-139.
Tannock, R., Ickowicz, A., & Schachar, R. (1995a). Differential-effects of methylphenidate on working-memory in ADHD children with and without comorbid anxiety. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 886-896.
Tannock, R., Schachar, R., Carr, R. P., Chajczyk, R. P., & Logan, G. D. (1989). Effect of methylphenidate on inhibitory control in hyperactive children. Journal of Abnormal Child Psychology, 17, 473-491.
Tannock, R., Schachar, R., & Logan, G. (1995b). Methylphenidate and cognitive flexibility: Dissociated dose effects in hyperactive children. Journal of Abnormal Child Psychology, 23, 235-266.
Taylor, E., Chadwick, O., Heptinstall, E., & Danckaerts, M. (1996), Hyperactivity and conduct problems as risk factors for adolescent development. Journal of the American Academy of Child Psychiatry, 35, 1213-1226.
Teicher, M., Anderson, C., Polcari, A., Glad, C., Maas, L., & Renshaw, P. (2000). Functional deficits in basal ganglia of children with attention deficit/hyperactivity disorder shown with functional magnetic resonance imaging relaxometry. Nature Medicine, 6, 470-473.
Thurston, C., Sobol, M. P., Swanson, J., & Kinsbourne, M. (1991). Effects of methylphenidate (Ritalin) on selective attention in hyperactive children. Journal of Abnormal Child Psychology, 7, 471-481.
Trommer, B. L., Hoeppner, J. A. B., & Zecker, S. G. (1991). The go-no-go test in attention deficit hyperactivity disorder is sensitive to methlyphenidate. Journal of Child Neurology, 6, S128-S131.
Vaidya, C., Austin, G., Kirkorian, G., Ridlehuber, H., Desmond, J., Glover, G., et al. (1998), Selective effects of methylphenidate in attention deficit hyperactivity disorder: A functional magnetic resonance study. Procedures of the National Academy of Science, 95, 14494-14499.
van der Meere, J., Vreeling, H. J., & Sergeant, J. (1992). A motor presetting study in hyperactive, learning disabled and control children. Journal of Child Psychology and Psychiatry, 33, 1347-1354.
Verbaten, M. N., Overtoom, C. C. E., Koelega, H. S., Swaab-Barneveld, H., van der Gaag, R. J., Buitelaar, J., et al. (1994). Methylphenidate influences both early and late ERP waves of ADHD children in a Continuous Performance Test. Journal of Abnormal Child Psychology, 22, 561-578.
Volkow, N., Gur, R., Wang, O., Fowler, J., Moberg, P., Ding, Y.-S., et al. (1998). Association between decline in brain dopamine activity with age and cognitive and motor impairment in healthy individuals. American Journal of Psychiatry, 155, 344-349.
Volkow, N., Wang, G., Fowler, J., Logan, J., Angrist, B., Hitzemann, R., et al. (1997). Effects of Methylphenidate on regional brain glucose metabolism in humans: Relationship to dopamine D2 receptors. American Journal of Psychiatry, 154, 50-55.
Vongher, J. M., Vassileva, J. L., Fischer, M., Conant, L., Risinger, R. C., Salmeron, B. J., et al. (2001). Behavioral inhibition and motor timing in ADHD adults. Brain and Cognition, 47, 219-222.
Waber, D. P., Weiler, M. D., Bellinger, D. C., Marcus, D. J., Forbes, P. W., Wypij. D., et al. (2000). Diminished motor timing control in children referred for diagnosis of learning problems. Developmental Neuropsychology, 17, 181-97.
Wilkison, P. C., Kircher, J. C., McMahon, W. M., & Sloane, H. N. (1995). Effects of methylphenidate on reward strength in boys with attention-deficit hyperactivity disorder. Journal of American Academy of Child and Adolescent Psychiatry, 34, 897-900.
Woodward, L., Dowdney, L., & Taylor, E. (1997). Child and family factors influencing the clinical referral of children with hyperactivity: A research note. Journal of Child Psychology and Psychiatry, 38, 479-485.
Zackay, D. (1990). The evasive art of subjective time measurement. In R. A. Block (Ed.), Cognitive models of psychological time (pp.59- 84). Hillsdale, NJ: Lawrence Erlbaum.
Katya Rubia (1,4), Janet Noorloos (3), Anna Smith (1), Boudewijn Gunning (3), and Joseph Sergeant (2)
(1.) Institute of Psychiatry, King's College London, London, United Kingdom.
(2.) Department of Clinical Neuropsychology, Vrije Universiteit, Amsterdam, The Netherlands.
(3.) Department of Child Psychiatry, Academic Medical Center, Amsterdam, The Netherlands.
(4.) Address all correspondence to Dr Katya Rubia, Senior Lecturer, Department of Child Psychiatry, Institute of Psychiatry, Maudsley Hospital, De Crespigny Park, London SE5 8AJ, United Kingdom; e-mail: k.rubia@iop.kcl.ac.uk.
COPYRIGHT 2003 Plenum Publishing Corporation
COPYRIGHT 2003 Gale Group