Angiotensin-converting enzyme (ACE) inhibitors are considered standard therapy in patients with left ventricular systolic dysfunction as the cause of their heart failure. However, chronic heart failure in general has a poor prognosis and, despite the benefits of ACE inhibitors, mortality and morbidity remain high in this patient population. Recent study results of the effects of beta1 blockade in patients with heart failure demonstrated a significant reduction in total mortality. Results from meta-analyses of previous smaller studies of various beta1 blockers indicate a benefit. The Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF) study demonstrated a reduction of 34 percent in mortality. Hjalmarson and associates report further on the MERIT-HF study, specifically looking at the effect of controlled-release/extended-release (CR/XL) metoprolol on hospitalization, heart failure symptoms and quality of life.
The MERIT-HF study included 3,991 patients with chronic heart failure and reduced ejection fraction. The study was a double-blind, placebo-controlled, randomized trial. The primary outcome measures were total mortality and the combined end point of total mortality or all-cause hospitalization (time to first event). The study was discontinued earlier than planned because of the significant reduction (as mentioned above) in mortality in patients taking metoprolol CR/XL. Other outcomes recorded included death, heart transplantation, nonfatal acute myocardial infarction, emergency department visits because of worsening heart failure and change in the New York Heart Association (NYHA) functional class. Patients with symptomatic heart failure (NYHA classes II to IV) of at least three months' duration and a left ventricular ejection fraction of no more than 0.40 in men or women between 40 and 80 years of age were included in the study. Other inclusion criteria included a resting heart rate of at least 68 beats per minute, with the patient receiving optimal heart failure pharmacotherapy (defined as any combination of diuretic plus ACE inhibitor at least two weeks before randomization). Patients were excluded if they had an acute myocardial infarction or unstable angina within 28 days of randomization, severe decompensated heart failure (e.g., pulmonary edema or hypoperfusion) or a supine systolic blood pressure of less than 100 mm Hg. Patients with an indication for or contraindication to beta blockers were also excluded.
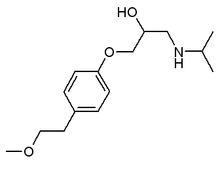
Patients were randomized to receive one 25-mg tablet of metoprolol CR/XL once daily or placebo. Patients with worsening heart failure (NYHA functional class III or IV) were started on a 12.5 mg per day dosage). The suggested regimen was to double the dosage every two weeks until a level of 200 mg per day was reached, although the researchers were allowed to adjust this regimen at their discretion. During follow-up, patients were seen every three months. Follow-up included assessment of NYHA functional class, as well as quality of life, using standard assessment instruments. There were 2,004 patient-years accounted for in the metoprolol CR/XL group and 1,977 patient-years in the placebo group, in terms of total mortality. There were similar numbers for combined mortality/all-cause hospitalization and for worsening heart failure. The mean follow-up was one year. Groups were not significantly different at baseline.
Metoprolol CR/XL therapy reduced all combined end points (time to first event) compared with placebo. All-cause hospitalization or total mortality decreased by 19 percent, hospitalization or total mortality for worsening heart failure decreased by 31 percent, death or heart transplantation decreased by 32 percent and nonfatal acute myocardial infarction or cardiac death decreased by 39 percent. Patients receiving metoprolol CR/XL were less likely to be hospitalized for all causes or, if hospitalized, to have as lengthy a stay as those receiving placebo. The NYHA functional class improved two levels between baseline and the last visit (as rated by the physician) in 2.6 percent of patients receiving metoprolol CR/XL versus 1.5 percent of patients receiving placebo. Deterioration was seen in 6.0 percent of patients receiving metoprolol CR/XL versus 7.5 percent of patients receiving placebo. The overall treatment evaluation score improved significantly in the treatment group compared with the placebo group, with 72 percent of patients judging this to be an important change. Reasons for discontinuing the assigned drug were worsening heart failure, angina pectoris and atrial fibrillation; more of these events occurred in the placebo group.
The authors conclude that metoprolol CR/XL given daily (in addition to conventional therapy) to patients with chronic heart failure caused by left ventricular systolic dysfunction leads to improved survival, fewer hospital admissions because of worsening heart failure and overall improvement in well-being. Using the CR/XL formulation makes the regimen simpler for the patient (once-daily dosage) and allows titration up to a higher total daily dosage (200 mg daily) than conventionally used thrice-daily dosing (50 mg three times daily), without an increase in peak plasma concentration.
COPYRIGHT 2000 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group