Studying subjects heterozygous for mutations of the cystic fibrosis (CF) gene may help clarify the impact on disease onset of CF transmembrane conductance regulator protein (CFTR-)-dependent chloride secretion. CFTR-mediated chloride transport was evaluated in 52 heterozygous subjects, 32 healthy control subjects, and 77 patients with CF with class I or II mutations. We measured the change in nasal potential difference in response to chloride-free isoproterenol solution for each subject and used a video-imaging fluorescent dye assay to assess the percentage of nasal ciliated cells with cAMP-dependent anion conductance. Our findings did not confirm the standard assumption that heterozygosity implies 50% of normal CFTR function. Half the heterozygous subjects had CFTR-mediated chloride transport levels below 50% of the normal range, and one-third had levels similar to those of the patients with CF. This reduced CFTR function was not associated with an elevated prevalence of CF-like symptoms in heterozygous subjects but was highly related to respiratory status in the patients with CF. These data suggest that CFTR-dependent chloride conductance does not directly modulate disease severity but may be part of a more global defect in patients with CF involving other CFTR functions or currently unknown modulatory factors.
Keywords: cystic fibrosis transmembrane conductance regulator; heterozygosity; nasal potential difference
Cystic fibrosis (CF) is caused by mutations in the gene encoding for the CF transmembrane conductance regulator (CFTR) protein, which acts as a chloride channel after activation by cyclic AMP (cAMP) (1). Classic CF is characterized by chronic bacterial infection in the airways, fat maldigestion caused by pancreatic exocrine insufficiency, and elevated chloride concentrations in sweat (2). More than 1,300 mutations have been described. Premature termination signals (class I mutations) and abnormal protein folding (class II mutations, including ΔF508, the most common CFTR mutation) are characterized by the absence of CFTR protein at the apical membrane, whereas class III, IV, and V mutations produce proteins that are inserted in the apical membrane but either do not function normally (class III and IV) or result in significantly decreased production of normal CFTR (class V) (3). However, although pancreatic insufficiency is associated with class I, II, and III mutations, there is no correlation between genotype and severity of pulmonary disease (4).
In a previous study, we found residual cAMP-dependent chloride conductance in the nasal ciliated cells (NCC) of ΔF508 homozygous patients with mild lung disease (5). This finding led us to wonder whether clinical heterogeneity in patients with CF might be linked to heterogeneity in CFTR function. Studying heterozygous subjects for CFTR mutations may help clarify the relation between CFTR function and onset of CF symptoms because, in this population, the mutation's clinical expression is not obscured by the secondary consequences of the disease (6). Furthermore, heterozygous subjects with CF are known to be overrepresented among patients with isolated features of the classic CF phenotype, such as asthma (7), disseminated bronchiectasis (8), allergic bronchopulmonary aspergillosis (9), chronic sinusitis (10), chronic pancreatitis (11), congenital bilateral absence of the vas deferens (12), and elevated sweat chloride concentrations (13).
CFTR functioning in heterozygous subjects is generally assumed to be half of the normal level, which is believed to be sufficient to remain disease-free (6, 14). Two studies of heterozygous subjects with isolated CF symptoms, however, reported low CFTR-dependent chloride levels (15, 16). They suggested that a single mutation might be sufficient to reduce CFTR function to the range found in patients with CF and that this may, in turn, be related to the expression, albeit limited, of a CF phenotype (17).
This study investigated CFTR-mediated chloride transport in nasal epithelium with nasal potential difference (NPD) measurements and a halide-sensitive fluorescent dye assay to determine whether the level of this chloride secretion is related to clinical expression of CF in a population of heterozygotes and patients with CF with class I and class II CFTR mutations.
METHODS
Subjects
All patients with CF had class I or class II mutations on both alleles. The heterozygous subjects, also carrying a class I or II mutation, were either parents or siblings of patients with CF with known mutations. Control subjects had no family history of CF and were asymptomatic. Before inclusion, they were screened and found negative for the 30 CFTR mutations most prevalent in the French population. The study was approved by the Necker-Enfants Malades Ethics Committee, and written, informed consent was obtained from each adult and parent.
Procedures
We recorded the medical history and performed a chest film and pulmonary function tests for each subject and assessed the Shwachman clinical score for patients with CF (18).
Sweat chloride concentrations were determined by conductivity with the Sweat-Chek conductivity analyzer (J2L Elitech; Wescor, Labarthe Inard, France) (19). Because sweat conductivity methods yield sodium chloride values approximately 15 mEq/L higher than pad-absorption iontophoresis methods, chloride concentrations above 70 mEq/L were defined as abnormal and those between 50 and 70 mEq/L as borderline.
We used the procedure of Knowles and collaborators (20) to determine NPD. Baseline NPD was measured after perfusion of nasal epithelium with saline solution. NPD changes were recorded after perfusion with the following solutions: 100 µM amiloride in saline solution (Δamiloride), chloride-free solution with 100 µM amiloride (Achloride-free), and 100 µM amiloride plus 10 µM isoproterenol in chloride-free solution (Δisoproterenol). The sum of Achloride-free and Δisoproterenol (Δchloride-free-isoproterenol) served as an index of transepithelial CFTR-dependent chloride transport because it reflects the cAMP activation of nasal mucosa chloride permeability.
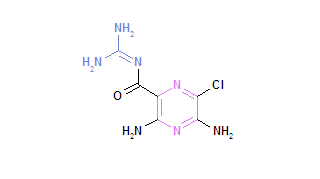
We used a halide-sensitive video-imaging assay with fluorescent dye 6-methoxy-N-3'-sulfopropylquinolinium (SPQ) to measure chloride transport at the cellular level, as described by Verkman (21). After loading the cells with 10 mM SPQ (Molecular Probes Europe, Leiden, The Netherlands), the cells were continuously perfused with the isotonic NaI solution, followed by the NaNO^sub 3^ solution, to which cAMP agonists were finally added (5). Details on this method are available in the online supplement. The maximum change in fluorescence rate after addition of cAMP agonists was defined as cAMP-dependent anion conductance (ΔF^sub cAMP^/Δt) and the CFTR-mediated cAMP-stimulated anion conductive pathway was considered present when ΔF^sub cAMP^/Δt was greater than 0.1 (Figure 1). At least five NCC were studied for each experiment, and the SPQ assay endpoint was the percentage of cells with cAMP response (%cAMP) in a given experiment. Details on this method are available in the online supplement.
CFTR transcript levels were analyzed in nasal cells by reverse transcriptase-polymerase chain reaction as previously reported (5). CFTR mRNA content was expressed as the ratio of the densitometric value of CFTR amplification product to that of β^sub 2^-microglobulin amplification product.
The variable IVS8 (TGmTn) sequence at 1342-12 was investigated in heterozygous individuals to ascertain if the IVS8-5T variant might be related to a defect in CFTR functioning. This test was performed either by direct sequencing or by denaturing gradient gel electrophoresis of a fragment containing exon 9 and its surrounding sequences (22). Each DGGE pattern obtained could be allocated to a specific combination of TGmTn.
Statistical Analysis
Data are presented as mean (SEM) for n subjects. Groups were compared with an unpaired t test or with the Mann-Whitney U test if there were fewer than 30 subjects per group. Because CFTR functioning in heterozygous subjects is generally assumed to be 50% of normal, the results of these assays were compared with 50% of the corresponding mean value for control subjects, a value representing a 50% reduction of normal CFTR function. Correlation coefficients were calculated with simple regression analysis or, if there were fewer than 30 values, with Spearman's rank correlation test. A p value less than or equal to 0.05 was considered statistically significant.
RESULTS
Subjects' Clinical Characteristics and Genotypes
The study included 52 heterozygous subjects, 32 control subjects, and 77 patients with CF (Table 1). Patients had the following mutations: ΔF508/ΔF508 (n = 46), class I/class II (n = 22), or class I on both alleles (n = 9). Most of the mutations observed in heterozygous subjects were class II: ΔF508 (n = 40) and N1303K (n = 2) mutations. Ten had class I mutations: 3659delC, 1078delT, 3791delC, 1717-1G>A, 2183AA>G, S466X, W1282X, R553X, or G542X (n = 2). Five of the 52 heterozygous subjects had possible CF-related symptoms: three had chronic sinusitis and two had asthma. All heterozygous and control subjects had normal chest films and pulmonary function tests. Forty-four patients had chronic Pseudomonas aeruginosa colonization.
Sweat Test
Sweat chloride concentrations were measured in all heterozygous and control subjects and a sample of 20 patients with CF (Table 1). The mean level for the heterozygote population was significantly higher than for the control group: 51 (range, 27-109) mEq/L compared with 41 (range, 30-55) mEq/L (p = 0.01). Twenty-seven heterozygous subjects had borderline sweat chloride concentrations, ranging from 50 to 70 mEq/L, but they had no clinical symptoms. One heterozygous subject had a sweat chloride concentration of 109 mEq/L and moderate asthma. An extensive gene search did not reveal a second CFTR mutation.
Functional Assays
Measurement of NPD. Neither the baseline nor the Aamiloride NPD values of heterozygous and control subjects differed significantly, but patients' baseline NPD was significantly more negative and they had significantly greater depolarization after amiloride (Table 1, lines 6 and 7; Figures 2A and 2B). After chloride-free superfusion and after isoproterenol, NPD response for the three groups overlapped significantly (Figures 2C and 2D). Nevertheless, change in the voltage response was significantly lower among heterozygotes than among control subjects and was minimal or absent in the patient group (Table 1, lines 8, 9, and 10; Figures 2C, 2D, and 2E). Among the heterozygous subjects, the five symptomatic subjects did not differ from the others in their NPD results.
The Δchloride-free-isoproterenol response in heterozygous subjects was compared with 50% of its mean absolute value in the control group (i.e., |-7.5| mV; from Table 1, line 10), a value that reflects 50% of the normal CFTR-regulated cAMP-dependent chloride secretion. After perfusion of isoproterenol in chloride-free solution, repolarization of less than |-7.5| mV was observed for 17 heterozygous subjects (46%; Figure 2E). In this group, the mean Δchloride-free-isoproterenol was -4.3(0.4) mV versus -12.5(1.2) mV for the patients with repolarization greater than |-7.5| mV. These subjects did not differ from the other heterozygous subjects for the prevalence of isolated CF-like symptoms, the results of respiratory function tests, or sweat chloride concentrations. This pattern did not change when the analysis was restricted to ΔF508 heterozygotes.
In the patient group, we focused on the isoproterenol response because the low chloride response may vary with natural hormonal influences. The magnitude of this response was compared with 50% of its mean absolute value in the control group (i.e., |-2.5| mV; from Table 1, line 9). Six patients with CF (16%) responded to isoproterenol with a voltage change of |-2.5| mV or greater, thereby demonstrating the persistence of more than 50% of the CFTR-dependent chloride permeability. They had better respiratory function tests and Shwachman scores than the patients with Aisoproterenol values of less than |-2.5| mV (Table 2).
SPQ Fluorescent Dye Video-imaging Assay. The heterozygous subjects and the patients had overlapping %cAMP values (Figure 3). For the control subjects, the lowest proportion of NCC demonstrating a cAMP-dependent conductance was 50%, whereas heterozygous subjects and patients with CF had responses scattered between 0 and 100% (Table 1, line 11; Figure 3). Results did not differ between the symptomatic and nonsymptomatic heterozygous subjects. This pattern of results did not change when the analysis was restricted to the ΔF508 carriers and the ΔF508 homozygous patients. Nine of the 17 heterozygous subjects investigated with the SPQ assay (52%) had cAMP-mediated response in less than 50% of their NCC. Eight of the 17 heterozygous subjects had %cAMP levels less than or equal to the mean patient response (i.e., 38%), and four had no cells showing a cAMP-dependent conductive pathway (Figure 3). These findings reveal that CFTR function was reduced by more than 50% in half of the subjects investigated and that one-third had levels similar to those of the patients with CF. The heterozygous subjects with %cAMP of less than 50% did not differ from those with %cAMP of 50% or greater for CF-related symptoms, sweat chloride concentrations, or respiratory function tests.
%cAMP greater than 50% was observed in 31 patients (40%). Their clinical status was less severe than that of the other patients in terms of respiratory status, number of bronchial exacerbations requiring antibiotics, and Shwachman score (Table 2).
%cAMP was significantly correlated with Δisoproterenol (r = 0.46, p = 0.01) but not with Δamiloride (r = 0.32, p = 0.08) or Δchloride-free (r = 0.15, p = 0.43; Spearman correlation test; results based on the entire study population; Figure 4).
Intron 8Tn Sequence Analysis
Forty heterozygous subjects underwent a functional exploration either by NPD test or the SPQ assay. Nineteen heterozygous subjects agreed to provide a blood sample to investigate the IVS8 (TGmTn) genotyping pattern. None carried the 5T allele. Nine had either Δchloride-free-isoproterenol or %cAMP below 50% of the control value. Of the 21 heterozygous subjects who could not be tested, we would expect only one to carry the 5T allele, considering its 5% frequency in the general population (12). However, in this group, 15 subjects had CFTR function reduced below the 50% level according to either the NPD test or the SPQ assay. These data suggest that the presence of 5T is not related to the function of CFTR.
CFTR Expression
CFTR mRNA levels did not differ between heterozygous subjects and patients with CF (Table 1). The transcript levels were not correlated with either Δisoproterenol or %cAMP.
DISCUSSION
Few studies have investigated CFTR function in carriers of CFTR mutations. Wilson and colleagues (23) reported greater sodium transport inhibition among them, whereas Knowles and colleagues (24) found PD values similar to those of a control group. Both studies involved small heterozygote samples. This is the first large-scale study to investigate CFTR function in individuals heterozygous for a CFTR mutation compared with two control groups, one healthy and one composed of patients with CF. We found significantly lower cAMP-mediated conductance in the nasal epithelium of heterozygous subjects with class I or II mutations. Our study of a large sample shows that CFTR-mediated chloride transport appears to be reduced by more than 50% in about half of the heterozygous subjects investigated and reaches levels similar to those in one-third of patients with CF. This pattern of results was similar when the analysis was restricted to the ΔF508 mutation. These results are consistent with another study of carriers of CFTR mutations and obligate heterozygous subjects, which also found significant alterations in CFTR ion channel function (25).
Investigation of CFTR-dependent Cl- Conductance in Nasal Epithelium
The cAMP-activated Cl- conductance in the nasal epithelium was explored with measurements from two functional tests: Δchloride-free-isoproterenol for NPD and %cAMP for the SPQ video-imaging assay. It can be assumed that these tests reflect the cAMP-stimulated Cl- transport mediated by CFTR because our experimental protocols exclude the other cAMP-dependent Cl-conductive pathways present in the nasal epithelium (i.e., the Ca^sup 2+^ and the volume-mediated conductance pathways) (26). Specifically, we excluded the Ca^sup 2+^-induced response to isoproterenol reflected by a rapid rise in NPD that fades to baseline over 2 to 3 minutes. We considered only the steady-state value obtained after 3 to 5 minutes of chloride perfusion, which represents the cAMP-CFTR-mediated Cl- conductance (24). For SPQ assay, the cells were left to settle for 30 minutes, long enough to deactivate the cAMP-stimulated volume-dependent anion conductance.
The American Pediatric Society consensus statement on CF has validated the use of the NPD to identify CF in patients with borderline sweat tests and only one identified mutation (27). The principal disadvantage of NPD, however, is that nonspecific epithelial trauma, such as rhinitis or allergy, can damage the epithelial barrier and blunt all bioelectrical parameters. The SPQ video-imaging assay avoids this pitfall because it evaluates the chloride conductive pathway at the single-cell level, whereas NPD reflects all of the isoproterenol-activated conductive pathways across the entire epithelium (24). It must, nonetheless, be stressed that the SPQ assay requires high technology available only in specialized laboratories. The strong correlation between Aisoproterenol and %cAMP observed in our study suggests that the SPQ video-imaging test may be a useful tool for studying the Cl- channel CFTR function. This assay is currently used in CF gene therapy trials and clinical research assessment (5, 28-30).
Variability of CFTR Activity in Normal Nasal Epithelium
Our results show that the cAMP-dependent Cl- conductance pathway can vary markedly in the NCC of control subjects without CF and can be quite low regardless of the assay. This suggests that even a low level of functional protein is sufficient to offer protection from symptoms of CF disease. These results are consistent with previous studies demonstrating that the CFTR gene is expressed at low levels (1-2 transcripts/cell) in the epithelium of the nose, trachea, and bronchi (31) in normal, healthy individuals, and that this low level of normal CFTR is sufficient for restoration of normal airway epithelial function in gene transfer experiments (32, 33).
Residual CFTR Activity Is Related to Mild Pulmonary Disease in Patients with CF
Approximately one-third of the patients with CF showed a significant CFTR-dependent response for either the NPD test or the SPQ assay. This residual CFTR activity seems to be clinically relevant because these patients' pulmonary status is significantly better. This finding is consistent with those of previous studies that have documented mild pulmonary phenotypes in patients with residual CFTR functioning (5, 28, 34-36).
Reduction of CFTR Function in Heterozygous Subjects and Pathophysiologic Hypotheses
The loss of CFTR function in heterozygous subjects is not associated with either increased prevalence of isolated CF-related clinical symptoms or higher sweat chloride concentrations. CFTR-mediated chloride transport at the range seen in patients with CF thus does not appear to be related per se to clinical symptoms. A growing body of evidence suggests that mechanisms other than those related to chloride secretion may underlie chronic obstructive lung disease in patients with CF (37). Possibilities include hyperactivity of the amiloride-sensitive epithelial sodium channel (38), alterations in intracellular processes, reduced host defenses, and persistent inflammatory response (39). On the other hand, our results show that residual CFTR-dependent chloride transport in patients with CF is positively correlated with better clinical condition. The explanation for the apparent contradiction between the findings for heterozygous subjects and for patients with CF may be that the cAMP-dependent chloride transport is not directly correlated with CF disease severity but rather reflects a more global defect, involving other CTFR functions or other currently unknown modulatory factors.
Molecular Basis of CFTR Function Reduction in Heterozygous Subjects
Several hypotheses may explain how heterozygosity for CF mutations is linked to CF-like functional defects. We can rule out the hypothesis of a second undetected CFTR mutation in our group of heterozygous subjects, because they are obligate heterozygotes. Modulation of the phenotype by the genotype can be excluded because we reach similar conclusions when the analysis is restricted to the homozygous ΔF508 patients. Nor is a lower rate of CFTR transcription a plausible explanation, as we did not observe any correlation between it and the response to isoproterenol in NPD testing or to cAMP in the SPQ assay.
We analyzed the variable intron 8 (TG)mTn sequence to determine whether the 5T allele, in combination with a CF mutation, might be associated with reduced chloride secretion. Because none of the 19 heterozygotes tested carried the 5T allele and nine of them had CFTR function reduced below 50%, differential splicing of exon 9 cannot explain this reduction. A more likely explanation for this modulation of the impaired CFTRdependent chloride transport in heterozygous subjects is that the combination of one mutation with CFTR polymorphisms or with specific alleles of modifier genes modifies a post-translational step: for example, altering biosynthesis of the CFTR protein, decreasing its stability in the plasma membrane, or directly downregulating cAMP-dependent chloride secretion (40).
In conclusion, our results provide evidence of a defect in the CFTR-regulated chloride conductive pathway in heterozygous subjects, sometimes at levels similar to those seen in patients with CF. This reduced function is correlated with better clinical condition in patients with CF but does not seem to be clinically relevant in subjects who are heterozygous. Taken together, these results point to the need for large-scale studies of CF carriers and highlight the potential importance of alternatives to reduced CFTR-dependent chloride transport as a mechanism for CF pathogenesis (41).
Conflict of Interest Statement: I.S.-G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; M.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; B.V. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; E.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; T.N.-K. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; R.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; I.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.L.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; G.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; A.E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank all the children and parents who took part in the study as well as Delphine Bataille and Mireille Blonde for technical assistance.
References
1. Anderson MP, Gregory RJ, Thompson S, Souza PW, Paul S, Mulligan RL, Smith AE, Welsh MJ. Demonstration that CFTR is a chloride channel by alteration of its anion selectivity. Science 1991;253:202-205.
2. Stern RC. The diagnosis of cystic fibrosis. N Engl J Med 1997;336:487-491.
3. Choo-Kang LR, Zeitlin PL. Type I, II, III, IV and V cystic fibrosis transmembrane conductance regulator defects and opportunities for therapy. Curr Opin Pulm Med 2000;6:521-529.
4. Tsui LC, Durie P. Genotype and phenotype in cystic fibrosis. Hosp Pract 1997;32:115-134.
5. Sermet-Gaudelus I, Vallée B, Urbin I, Torossi T, Marianovski R, Fajac A, Feuillet MN, Bresson JL, Lenoir G, Bernaudin JF, et al. Normal function of the cystic fibrosis conductance regulator protein can be associated with homozygous ΔF508 mutation. Pediatr Res 2002;52:628-635.
6. Griesenbach U, Geddes DM, Alton EW. The pathogenic consequences of a single mutated CFTR gene. Thorax 1999;54:S19-S23.
7. Dahl M, Tybjaerg-Hansen A, Lange P, Nordestgaard BG. Delta-F508 heterozygosity in cystic fibrosis and susceptibility to asthma. Lancet 1998;351:1911-1913.
8. Girodon E, Cazeneuve C, Lebargy F, Chinet T, Costes B, Ghanem N, Martin J, Lemay S, Scheid P, Housset B, et al. CFTR gene mutations in adults with disseminated bronchiectasis. Eur J Hum Genet 1997;5: 149-155.
9. Miller PW, Hamosh A, Macek MJR, Greenberger PA, Maclean J, Walden SM, Slavin RG, Cutting GR. Cystic fibrosis transmembrane conductance regulator (CFTR) gene mutations in allergic bronchopulmonary aspergillosis. Am J Hum Genet 1996;59:45-51.
10. Wang X, Moylan B, Leopold DA, Kim J, Rubenstein RC, Togias A, Proud D, Zeitlin PL, Cutting GR. Mutation in the gene responsible for cystic fibrosis and predisposition to chronic rhinosinusitis in the general population. JAMA 2000;284:1814-1819.
11. Cohn JA, Friedman KJ, Noone PG, Knowles MR, Silverman LM, Jowell PS. Relation between mutations of the cystic fibrosis gene and idiopathic pancreatitis. N Engl J Med 1998;339:653-658.
12. Chillon M, Casals T, Mercier B, Bassas L, Lissens W, Silber S, Romey MC, Ruiz-Romero J, Verlingue C, Claustres M. Mutations in the cystic fibrosis gene in patients with congenital absence of the vas deferens. N Engl J Med 1995;332:1475-1480.
13. Farrell PM, Koscik RE. Sweat chloride concentrations in infants homozygous or heterozygous for ΔF508 cystic fibrosis. Pediatrics 1996;97:524-528.
14. Castellani C, Quinzii C, Altieri S, Mastella G, Assael BM. A pilot survey of cystic fibrosis clinical manifestations in CFTR mutation heterozygotes. Genet Test 2001;5:249-254.
15. Bronsveld I, Bijman J, Mekus F, Ballmann M, Veeze HJ, Tiimmler B. Clinical presentation of exclusive cystic fibrosis lung disease. Thorax 1999;54:278-281.
16. Noone PG, Zhou Z, Siverman LM, Jowell PS, Knowles MR, Cohn JA. Cystic fibrosis gene mutations and pancreatitis risk: relation to epithelial ion transport and trypsin inhibitor gene mutations. Gastroenterol 2001;121:1310-1319.
17. Super M. Can manifesting heterozygotes have cystic fibrosis? Thorax 1999;54:194-195.
18. Shwachman H, Kulczycki LL. Long term study of one hundred five patients with cystic fibrosis. Am J Dis Child 1958;96:6-15.
19. Hammond KB, Turcios NL, Gibson LE. Clinical evaluation of the macroduct sweat collection system and conductivity analyser in the diagnosis of cystic fibrosis. J Pediatr 1994;124:255-260.
20. Knowles MR, Paradise AM, Boucher RC. In vivo nasal potential difference: techniques and protocols for assessing efficacy of gene transfer in cystic fibrosis. Hum Gene Ther 1995;6:445-455.
21. Verkman AS. Development and biological applications of chloride-sensitive fluorescent indicators. Am J Physiol 1990;259:C375-C388.
22. Costes B, Girodon E, Ghanem N, Flori E, Jardin A, Soufir JC, Goossens M. Frequent occurrence of the CFTR intron 8 (TG)n 5T allele in men with congenital bilateral absence of the vas deferens. Eur J Hum Genet 1995;3:285-293.
23. Wilson D, Ellis L, Zielenski J, Corey M, Ip WF, Tsui LC, Tullis E, Knowles MR, Durie PR. Uncertainty in the diagnosis of cystic fibrosis: possible role of in vivo nasal potential difference measurements. J Pediatr 1998;132:596-599.
24. Knowles M, Gatzy J, Boucher R. Increased bioelectric difference across respiratory epilhelia in cystic fibrosis. N Engl J Med 1981;305:1489-1495.
25. Ellis L, Dupuis A, Martin S, Yuan X, Schibli S, Corey M, Zielenski J, Tullis E, Durie PR. Do carriers of CFTR mutations have alterations in ion channel function [abstract]? Pediatr Pulmtmol 2004;38(Suppl 27): A111.
26. Anderson MP, Shcppard DN, Berger HA, Welsh MJ. Chloride channels in the apical membrane of normal and cystic (ibrosis airway and intestinal epithelia. Am J Physiol 1992;263:1-14.
27. Rosenstein BJ, Cutting GR. The diagnosis of cystic fibrosis: a consensus statement. Cystic Fibrosis Foundation Consensus Panel. J Pediatr 1998; 132:589-595.
28. Thomas SR, Jaffe A, Geddes DM, Hudson ME, Alton EWFW. Pulmonary disease severity in men with ΔF508 cystic fibrosis and residual chloride secretion. Lancet 1999;353:984-985.
29. Stern M, Munkonge FM, Caplen NJ, Sorgi F, Huang L, Geddes DM, Alton EWFW. Quantitative fluorescence measurements of chloride secretion in native airway epithelium from CF and non-CF subjects. Gene Ther 1995;2:766-774.
30. McLachlan G, Ho L-P, Davidson-Smith H, Samways J, Davidson H, Stevenson BJ, Carothers AD, Alton EsWFW, Middleton PG, Smith SN, et al. Laboratory and clinical studies in support of cystic fibrosis gene therapy using pCMV-CFTR-DOTAP. Gene Ther 1996;3:1113-1123.
31. Trapnell BC, Chu C-S, Paakko PK, Banks TC, Yoshimura K, Ferrans VJ, Chernick MS, Crystal RG. Expression of the cystic fibrosis transmembrane conductance regulator gene in the respiratory tract of normal individuals and individuals with cystic fibrosis. Proc Natl Acad Sci USA 1991;88:6565-6569.
32. Dorin JR, Parley R, Webb S, Smith SN, Farini E, Dclaney SJ, Wainwright BJ, Alton EW, Porteous DJ. A demonstration using mouse models that successful gene therapy for cystic fibrosis requires only partial gene correction. Gene Ther 1996;3:797-801.
33. Zhang Y, Jiang Q, Dudus L, Yankaskas JR, Engelhardt JF. Vector-specific complementation profiles of two independent primary defects in cystic fibrosis airways. Hum Gene Ther 1998;9:635-648.
34. Ho LP, Samways JM, Porteous DJ, Dorin JR, Carothers A, Greening AP, Innes JA. Correlation between nasal potential difference measurements, genotype and clinical condition in patients with cystic fibrosis. Eur Respir J 1997;10:2016-2022.
35. Bronsveld I, Mekus F, Bijman J, Ballman M, De Jonge HR, Laabs U, Halley DJJ, Ellemunter H, Mastella G, Thomas S, et al. Chloride conductance and genetic background modulate the cystic fibrosis phenotype of ΔF508 homozygous twins and siblings. J Clin Invest 2001; 108:1705-1715.
36. Bronsveld I, Mekus F, Bijman J, Ballman M, Greipel J, Hundrieser J, Halley DJJ, Laabs U, Busche R, De Jonge HR, et al Residual chloride secretion in intestinal tissue of ΔF508 homozygous twins and siblings with cystic fibrosis. Gastroenterology 2000;119:32-40.
37. Groman FD, Meyer ME, Wilmott RW, Zitlin PL, Cutting GR. Variant cystic fibrosis phenotypes in the absence of CFTR mutations. N Engl J Med 2002;347:401-407.
38. Mall M, Grubb BR, Harkema JR, O'Neal WK, Boucher RC. Increased airway epithelial Na+ absorption produces cystic fibrosis-like disease in mice. Nat Med 2004;10:487-493.
39. Becker MN, Saucr MS, Muhlebach MS, Hirsh AJ, Wu Q, Verghese MW, Randell SH. Cytokine secretion by cystic fibrosis epithelial cells. Am J Respir Crit Care Med 2004;169:645-653.
40. Nadeau JH. Modifier genes in mice and humans. Nat Rev Genet 2001;2: 165-174.
41. Knowles MR, Durie PR. What is cystic fibrosis? N Engl J Med 2002;347: 439-442.
Isabelle Sermet-Gaudelus, Michèle Déchaux, Benoît Vallée, Anne Fajac, Emanuelle Girodon, Thao Nguyen-Khoa, Rémi Marianovski, Ilse Hurbain, Jean Louis Bresson, Gérard Lenoir, and Aleksander Edelman
Centre de Ressources et de Compétences en Mucoviscidose, Laboratoire d'Explorations Fonctionnelles Rénales, Service de Biochimie A, Service d'ORL, and Centre d'Investigation Clinique, Hôpital Necker-Enfants Malades; INSERM U 467, Université Paris 5; Service d'Histologie-Biologie Tumorale, Hôpital Tenon, Paris; and Service de Biochimie-Génétique, Hôpital Henri Mondor, and INSERM U 468, Créteil, France
(Received in original form June 11, 2004; accepted in final form January 28, 2005)
Supported by the Association pour l'Aide à la Recherche contre la Mucoviscidose et l'Assistance aux Malades and the ABCF Protéines Association.
Correspondence and requests for reprints should be addressed to Aleksander Edelman, Ph.D., INSERM U 467, Faculté de Médecine Necker, 156 rue de Vaugirard, Paris 75730, France. E-mail: edelman@necker.fr
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 1026-1031, 2005
Originally Published in Press as DOI: 10.1164/rccm.200406-740OC on February 11, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society May 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved