Definition
Withdrawal syndrome occurs in drug and alcohol addicted individuals who discontinue or reduce the use of their drug of choice. This process of eliminating drugs and alcohol from the body is known as detoxification. Anxiety, insomnia, nausea, perspiration, body aches, and tremors are just a few of the physical and psychological symptoms of drug and alcohol withdrawal that may occur during detoxification.
Description
Drugs and alcohol affect mood by altering brain chemistry, specifically the production of neurotransmitters. Neurotransmitters are chemicals in the central nervous system that enable nerve impulses to travel through the central nervous system and regulate thought processes, behavior, and emotion. Drugs that temporarily elevate neurotransmitter levels are called stimulants. Drugs that decrease neurotransmitter levels and depress the central nervous system are called depressants; they include opiates and sedative-hypnotic drugs such as alcohol and barbiturates. (There are exceptions: Benzodiazepine elevates the level of an inhibitory neurotransmitter, GABA, therefore it serves as a tranquilizer)
When drug or alcohol consumption becomes chronic, the body adjusts to the constant presence of the substance by changing its normal production of neurotransmitters. If drug and alcohol use suddenly stops, the body and central nervous system react to the absence of the substance with an array of symptoms known collectively as withdrawal syndrome.
Causes & symptoms
Acute withdrawal syndrome begins within hours of abstinence, and includes a full range of physical and psychological symptoms. More long-term, or subacute, withdrawal symptoms, such as intense drug craving, may occur weeks or months after detoxification has taken place.
Alcohol withdrawal
Alcohol withdrawal syndrome occurs in alcohol-dependent individuals who suddenly stop or dramatically reduce their alcohol intake. The onset of the syndrome is likely to occur within a week, but usually occurs within 24 hours of the individual's last drink, and is triggered when the central nervous system attempts to adjust to the sudden absence of ethyl alcohol in the body. Symptoms may include extreme anxiety, disorientation, hallucinations, sleep disorders, hand tremors, nausea, sweating, seizures, and racing pulse. Delirium tremens (DTs) are an extreme example of withdrawal. In the worst cases, untreated alcohol withdrawal syndrome can result in death.
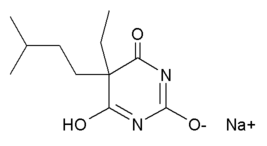
Barbiturate withdrawal
Barbiturates are prescribed as anticonvulsants, sedatives, and general anesthetics. They can also mimic some of the characteristics of alcohol intoxication (including euphoria, elation, and uninhibited behavior), which make them candidates for abuse. Commonly abused barbiturates include amobarbital (Amytal), pentobarbital (Nembutal), and secobarbital (Seconal). These drugs depress the respiratory and nervous system functions; and, because abusers rapidly build up a tolerance to the effects of the drug, fatal overdose or coma can easily occur. Symptoms of withdrawal syndrome appear 12-20 hours after the last dose; they include anxiety, irritability, elevated heart and respiration rate, muscle pain, nausea, tremors, hallucinations, confusion, and seizures. Death is a possibility if the condition is left untreated. Because barbiturates decrease REM sleep (rapid eye movement sleep, during which dreaming takes place), withdrawal often results in sleep disruptions such as nightmares, insomnia, or vivid dreaming.
Opiate withdrawal
Opiates are powerfully addictive analgesic drugs that deaden nerve pathways related to pain. Abusers of propoxyphene (Darvon), meperidine (Demerol), percocet (Oxycodone), heroin, morphine, and other powerfully addictive opiates quickly build up a tolerance to the drugs and need progressively larger doses to achieve the desired effect. Stopping or reducing the intake of the drug can cause severe withdrawal symptoms, which begin six to eight hours after the last dosage. Symptoms are flu-like, and include gastrointestinal distress, anxiety, nausea, insomnia, muscle pain, fevers, sweating, and runny nose and eyes.
Stimulant withdrawal
Use of stimulants, such as cocaine, crack, amphetamines, and methamphetamines, cause an increase in neurotransmitters in the central nervous system and produce feelings of alertness and increased energy. This initial "rush" is followed by a longer period of neurotransmitter loss, characterized by depression, lethargy, and a craving for more stimulants -- sometimes called a rebound effect. When a stimulant-dependent individual abstains from stimulant use, withdrawal symptoms, including depression, fatigue, insomnia, and loss of appetite, reflect this drop in neurotransmitter levels. Withdrawal typically takes one to two weeks.
Diagnosis
A detailed history of the patient's drug or alcohol use taken before detoxification can be helpful in predicting the severity of withdrawal symptoms. Standardized clinical tests, such as the Clinical Institute Withdrawal Assessment for Alcohol, revised, (CIWA-Ar), are used to evaluate the severity of withdrawal symptoms throughout the detoxification procedure.
Treatment
Pharmacologic and medical management is often recommended for withdrawal syndrome. The physical condition of the patient is closely monitored throughout the detoxification procedure.
Alcohol withdrawal
Alcohol withdrawal syndrome can be treated at home or in a hospital or treatment setting. Inpatient treatment is recommended for patients who are at risk for serious withdrawal symptoms or re-intoxication if treated as an outpatient. Withdrawal symptoms are minimized through the administration of cross-tolerant sedatives. Long-acting benzodiazepines, such as diazepam (Valium), chlordiazepoxide (Librium), and lorazepam (Ativan), are the pharmacologic treatment of choice in managing the symptoms of alcohol withdrawal. Drug dosage is adjusted to offset the discomfort of withdrawal, without causing a euphoric effect, and is then gradually decreased as withdrawal symptoms lessen.
Barbiturate withdrawal
Because the risk for seizures and other severe complications is high, barbiturate withdrawal should be monitored in a hospital setting. Patients are given low doses of phenobarbital at a regular interval until mild intoxication is achieved. The dosage amount and frequency is then gradually decreased until withdrawal is complete.
Opiate withdrawal
Two basic treatment approaches are used for managing opiate withdrawal. The first involves treating the symptoms of the withdrawal with appropriate medication. Clondine, an antihypertensive drug, is commonly prescribed to reduce muscle pain and cramping. Other symptom-specific drugs are administered on an as-needed basis.
The second treatment option is to replace the patient's drug of choice with methadone, a long-acting, cross-tolerant opiate that does not normally produce a "high." Doses of methadone are administered every four to six hours. The patient's reaction is closely observed, and dosages are slowly decreased until withdrawal symptoms have disappeared, and dosages are then discontinued. Methadone withdrawal can be completed within three weeks. It is important to note that methadone withdrawal treatment differs from a methadone maintenance program, in which patients who are unwilling to give up opiates are prescribed methadone as a legal, long-term substitute for their drug of choice.
Rapid opiate detoxification (ROD) is an emerging treatment option for opiate withdrawal. The ROD method is reported to be faster and to cause less physical discomfort than traditional forms of opiate detoxification. The treatment is typically performed in a hospital or private clinic setting. Naltrexone, an opiate antagonistic that blocks opiate receptors and reverses the effects of opiates, is administered to trigger the withdrawal response. Clonidine is given simultaneously to ease the symptoms of withdrawal. The patient is anesthetized throughout the three to four hour procedure, and withdrawal occurs while the patient sleeps. Vital signs are monitored closely and a ventilator may be employed.
Stimulant withdrawal
Because of the depression and dysphoria (feeling of a psychological low) related to stimulant withdrawal, psychological and/or medical management is critical. Treatment may include a regimen of drugs that increase neurotransmitter production.
Prognosis
A closely observed, medically managed detoxification typically results in a safe and tolerable withdrawal experience for the patient. Detoxification is only a short-term solution for obtaining abstinence. An addiction treatment and long-term recovery program is necessary to achieve long-term sobriety. Without such a treatment program, the likelihood of recurrence of abuse and, therefore, the recurrence of withdrawal syndrome is high.
Prevention
After detoxification, alcohol and drug dependent individuals are encouraged to maintain their abstinence through participation in substance abuse treatment or a twelve-step recovery program.
Key Terms
- Analgesics
- Pain killing drugs that depress respiratory function. Opiates are analgesics.
- Antagonist
- A substance that tends to nullify the action of another.
- Benzodiazepines
- Sedatives used to treat anxiety, epilepsy, and alcohol withdrawal syndrome. Diazepam (Valium), alprazolam (Xanax), and chlordiazepoxide (Librium) are all benzodiazepines.
- Cross-tolerant
- A drug that has the same pharmacological effect as another is considered cross-tolerant. Cross-tolerant drugs are often used in treating withdrawal syndromes.
- Detoxification
- The process of physically eliminating drugs and/or alcohol from the system of a substance-dependent individual.
- Dysphoria
- A depressed and anxious mood state.
- Neurotransmitters
- Chemicals in the brain that affect the nervous system and alter thinking patterns.
- Opiates
- Analgesic, pain killing drugs, such as heroin and morphine that depress the central nervous system.
Further Reading
For Your Information
Books
- Landry, Mim J. Understanding Drugs of Abuse: The Processes of Addiction, Treatment, and Recovery. Washington, DC: American Psychiatric Press, 1994.
- Schuckit, Marc A. Drug and Alcohol Use: A Clinical Guide to Diagnosis and Treatment. 4th ed. New York, NY: Plenum, 1995.
Periodicals
- Barttner, Thaddeus, and Lance Gooberman. "Rapid Opiate Detoxification." American Journal of Drug and Alcohol Abuse 22, no. 4 (Nov. 1996): 489-95.
- Hall, Wayne, and Deborah Zador. "The Alcohol Withdrawal Syndrome." The Lancet 349, no. 9069 (June 1997): 1897-900.
Organizations
- Alcoholics Anonymous (A.A). General Service Office. 475 Riverside Drive, New York, NY 10015. (212) 870-3400. http://www.alcoholics-anonymous.org/index.html.
- National Clearinghouse for Alcohol and Drug Information. Center for Substance Abuse Prevention. P.O. Box 2345, Rockville, MD 20847-2345. (800) 729-6686. http://www.health.org.
- National Council on Alcoholism and Drug Dependence. 12 West 21st Street, New York, NY 10010. (800) 622-2255. http://www.ncadd.org.
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). 6000 Executive Boulevard, Willco Building, Bethesda, Maryland 20892-7003. http://www.niaaa.nih.gov.
Gale Encyclopedia of Medicine. Gale Research, 1999.