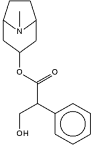
Recognition of the parasympathetic nervous system's importance in the pathogenesis of asthma and the development of anticholinergic agents with minimal bronchopulmonary absorption have led to renewed interest in the use of aerosolized anticholinergic drugs in the treatment of asthma. Anticholinergic agents, such as ipratropium bromide and AMN lack the undesirable systemic side effects of atropine sulfate and have a prolonged duration of action. (1) They are effective in the treatment of adult asthma (2,3) and chronic bronchitis, (4-6) but their efficacy in asthmatic children is controversial.
In single-dose studies in children more than three years of age, anticholinergic agents have been shown to have a bronchodilator effect, (7-10) and some investigators suggest that anticholinergic agents are as effective as beta-adrenergic agonists. (7,8) However, other investigators have not been able to confirm this degree of effectiveness. Also, several studies have suggested that the bronchodilator effect of anticholinergic agents is less consistent than that of beta agonists. (9,10)
Studies using combinations of beta agonists and anticholinergic agents in children are inconsistent. While some investigators report an additive effect, (11) others conclude that the effect of a combination is no better than that of beta-adrenergic agonists alone. (9,10) In these studies, combinations of maximum bronchodilator doses of anticholinergic agents and beta-adrenergic agonists were not evaluated.
The goal of this study was twofold. First, to determine if AMN is an effective bronchodilator in children who require the chronic use of other medications including steroids for control of their asthma. Second, to determine if the combination of maximum bronchodilator doses of AMN and albuterol provides additional bronchodilation compared with the maximum bronchodilator dose of either drug alone.
METHODS
The children enrolled in this study were patients with moderately severe to severe chronic steroid-requiring asthma who were undergoing inpatient evaluation and treatment at the National jewish Center for Immunology and Respiratory Medicine. All patients fulfilled the American Thoracic Society criteria for asthma. Patients had to be able to perform reliable spirometry. They were studied at a time that their asthma was stable and they were receiving a stable dose of corticosteroids.
Patients were considered allergic if they had another atopic disease besides asthma eczema, seasonal or perennial rhinitis) and at least four positive skin tests; or, if they did not have another atopic disease, they had at least four positive skin tests, an IgE >100 IU/ dl and a positive family history for the atopic diseases.
Patients were excluded from the study if they had an upper respiratory tract infection within one week of beginning the study This study was reviewed and approved by the National jewish Institutional Review Board. Informed consent was obtained from all patients and their legal guardians.
This study was divided into two phases. The first phase determined the individual patient's maximal bronchodilator dose and the maximal tolerated dose of nebulized AMN and albuterol. The second phase determined if there was any additional bronchodilator effect from using maximum bronchodilator doses of albuterol aDd AMN together. During both phases, chronic medications, including theophylline, cromolyn and corticosteroids, were continued on their routine schedule. The morning medications were given at 6:00 Doses of these medications remained constant throughout the study To avoid post-withdrawal cholinergic supersensitivity secondary to anticholinergic therapy, patients discontinued anticholinergic agents at least 72 h before beginning the study. (13) Beta-adrenergic agonists were withheld for 8 to 12 h prior to testing. Baseline morning FEV[.sub.1] values were required to be 50 to 80 percent of predicted or of the patients' best previous FEV[.sub.1] on the first study day. On subsequent study days, each patient's FEV[.sub.1] was required to be within [+ or -] 15 percent of his initial baseline value.
The medications employed were albuterol nebulizer solution (Schering Corporation, Kenilworth, NJ) and AMN (obtained from Henley and Co., Montvale, NJ; but produced by Boehringer Ingelheim, Federal Republic of Germany). During both phases, each dose of the medication was diluted to a constant 2 ml volume with sterile phenolated saline solution (0.4 percent, Albay, Hollister Stier, Spokane, WA). Medication was nebulized only during slow inspiration from FRC with the use of a closed nebulizer system (14) consisting of a nebulizer (model 646, (DeVilbiss), and T connector (DeVilbiss), and a Pulmonaide air compressor (DeVilbiss, Somerset, PA). Nebulization was continued until there was no further aerosol delivery The nebulizers were weighed before and after each treatment to calculate the output and then cleaned with water and dried before the next dose was administered.
The bronchodilator response FEV[.sub.1], PEFR, FEF25-75%) was measured with a Collins Eagle II spirometer with pneumotachograph (Warren E. Collins Inc, Braintree, MA). Calibration was performed in the morning and at least two other times during each study day. Spirometry was performed according to the American Thoracic Society guidelines allowing maximum variability of 5 percent between the two best efforts.
In phase 1, the maximal bronchodilator dose and maximal tolerated dose of albuterol and AMN were determined using a double-blind graded dose-response. The dosage schedule for each drug is summarized in Table 1. This schedule allowed each successive dose to be administered at the time of maximum bronchodilator effect from the previous dose. By following this schedule, the total cumulative dose for albuterol was 0.3 mg/kg with a maximum dose of 12 mg/study day. The total cumulative dose of AMN was 0.06 mg/kg of body weight with a maximum of 2.4 mg/study day. Maximum doses were given to children weighing [is greater than or equal to] 40 kg. These doses give maximum bronchodilation in adults. (15,16) Spirometry was performed before each treatment (at 8:00, 8:30, 9:00, 9:30 and 10:00 AM) and at 11:00 AM and 12:00 noon.
At the time of each spirometry test, pulse and blood pressure (sitting and standing), and an ECG rhythm strip were monitored. Objective responses, such as excitement and tremor, were assessed as well as subjective responses, such as the presence of headache, palpitations and dizziness. The study was discontinued if any significant side effects were observed. Significant side effects were considered to be an elevation of pulse rate of >20 beats/min over baseline, symptomatic postural hypotension, significant excitement or tremor or severe headache. Doses were expressed as amount of drug placed in the nebulizer, not that delivered to either the patient or lower airways. The maximal effective bronchodilator dose was defined as the cumulative dose up to and including the last dose, resulting in at least a 5 percent increase in the FEV[.sub.1] over the previous value. The maximal tolerated dose was defined as the cumulative dose of drug before the occurrence of significant side effects or the maximum cumulative dose administered.
In phase 2, the patients were given a single nebulized treatment at 6:45 AM on each of the four study days in a randomized, double-blind, crossover manner. The treatment was either saline placebo, the maximal bronchodilator dose of albuterol or AMN, or the combination of the maximal bronchodilator doses of albuterol and AMN. After the nebulized treatment, spirometry tests were performed at 30 min and hourly for 6 h. Vital signs and the objective and subjective measures outlined previously were determined both at 30 min and 1 h after the nebulized treatment.
ANALYSIS
Pulmonary function data FEV[.sub.1], PEFR and FEF25-75%) were expressed as absolute values. Comparison of data from phase 2 was performed using an analysis of variance with repeated measures with 95 percent confidence limits. Multiple comparisons were performed with Fisher's PLSD (Statview:512+, Brainpower, Inc, Calabasas, CA).
In comparing the degree of bronchodilation achieved with AMN and albuterol, the differing bronchodilator time course and the placebo baseline response were incorporated. The difference between the percentage of improvement above baseline at the time of maximal bronchodilator effect on the medication day was compared with the percentage of improvement above baseline at this same time on the placebo day.
Missing data points resulted from patients requesting early use of a bronchodilator (2.7 percent of data points), or on four occasions from missing pulmonary functions during the study (0.8 percent of data points). These accounted for only 3.5 percent of the data points in phase 2. There were no missing data points from phase 1. If the patient could not continue, the value for the last pulmonary function was used for the remainder of the study. On the four occasions when pulmonary function data were missing, an average of the values on either side of the missing value was used.
RESULTS
Twenty-three children were initially enrolled in this study. Five were subsequently dropped from the study for significant deterioration of baseline pulmonary function, uncertainty of the diagnosis, or significant variability from poor spirometric efforts. Seventeen patients (nine women and eight men) completed the first phase, but only sixteen (eight women and eight men) were able to complete both phases due to early hospital discharge of one patient. The mean age [+ or -] SD) was 13 [+ or -] 3 years (range: 10 to 18 years). The mean weight was 54.3 [+ or -] 4.5 kg (range: 32.5 to 99.1 kg). All patients were receiving oral sustained-release theophylline preparations and inhaled beta-adrenergic agonists. in addition, certain patients received slow release oral beta-adrenergic agonists (ten patients), inhaled corticosteroids (15 patients), inhaled cromolyn (15 patients), oral corticosteroids (eight patients) or ranitidine (six patients) or both of the latter. All patients except one could be considered allergic since most had other atopic diseases (14 patients), positive skin tests ([is greater than or equal to] 4 in 14 patients), or an elevated IgE (greater than 100 IU/DL in ten of 13 patients available). All had positive family histories of atopy.
In phase 1, the mean maximal bronchodilator dose of albuterol was 4.22 [+ or -] 0.51 mg or 0.11 [+ or -] 0.01 mg/kg, and the mean maximal tolerated dose [+ or -]SE) was 8.12 [+ or -] 0.89 mg or 0. 21 [+ or -] 0.02 mg/kg. Significant side effects observed from albuterol were tremor (17 patients), excitement (eight patients) and posturally related tachycardia and hypotension five patients with three manifesting a significant degree of dizziness, nausea and palpitation). The mean maximal bronchodilator dose for AMN was 1.27 [+ or -] 0.13 mg or 0.033 [+ or -] 0.0034 mg/kg. The maximal administered dose of AMN was 2.34 [+ or -] 0.04 mg (0. 06 mg/kg), the maximum intended for this study protocol. No subject developed significant side effects. Minor adverse effects attributed to AMN included mild tremor (ten patients), dryness of the mouth (three patients) and mild headaches (two patients). The mean [+ or -] SD) nebulizer output of the 2-ml dose was 74.4 [+ or -]8.4 percent with a range of 66.5 to 82.1 percent. This is consistent with data from previous reports. (14)
The results of the mean [+ or -] SE) FEV[.sub.1], FEF25-75% and PEFR during phase 2 are summarized in Figures 2 to 4. The maximal responses to albuterol and AMN occurred at 30 and 60 min, respectively. The response to albuterol declined gradually and was similar to that of the placebo in all parameters by the fifth hour. At no time was the AMN response superior to the albuterol response. The AMN response was significantly superior to the placebo response throughout the study for FEF25-75% but only up to and including the third study hour for FEV[.sub.1] and the fourth study hour for PEFR. In contrast, the response to the combination was more prolonged and remained persistently higher than that of the placebo throughout the 6-h study period. The superiority of the response to the combination therapy compared with albuterol alone could be recognized as early as the third hour but did not become statistically significant until the fourth hour for the FEF25-75% and the sixth hour for PEFR and FEV[.sub.1]. The baseline and maximal FEV[.sub.1] values for both phases are summarized in Table 2 [omitted]. Comparing the difference between the mean absolute maximal FEV[.sub.1] response and its respective baseline, the maximum AMN response was 89 percent of the maximal albuterol response for phase 1, and 91 percent for phase 2.
The maximum albuterol response occurred at 30 min in all but one patient. This contrasts with the maximum AMN response which occurred anywhere from 30 min to 6 h after the treatment. Since each of these medications has a different bronchodilator time course, the placebo baseline values to which they should be compared were different since there was a gradual rise in pulmonary function on the placebo days. In correcting for the placebo response as outlined in the "Methods" section, there was a 19.1 percent improvement above baseline on the placebo day compared with a 41.8 percent improvement above baseline on the AMN day for the same time points. Similarly, there was a 5.9 percent improvement above baseline on the placebo day compared with a 48.8 percent improvement above baseline on the albuterol day for the same time points. Thus allowing for the differing levels at the different times on the placebo days, the AMN response was 52.9 percent of the albuterol response. When an individual patient's response to the medication was compared with his own placebo response, six of the 16 patients had less than a 20 percent maximal increase from AMN and four of the 16 had less than a 20 percent maximal increase from albuterol.
No correlation existed between the corrected maximal bronchodilator effect with AMN and the patients' methacholine PC[.sub.20] or their baseline lung volumes using regression analysis. There also was no correlation between response to AMN and asthma severity, IgE level greater than 100 IU/dl or psychiatric diagnosis by chi square analysis.
DISCUSSION
This study demonstrates that AMN is an effective bronchodilator in children with stable, moderately severe to severe, steroid-requiring asthma and confirms the efficacy of albuterol as a bronchodilator in this group of patients.
With the closed delivery system used in this study, the maximal bronchodilator dose for albuterol was 0.11 [+ or -] 0.01 mg/kg or 4.22 [+ or -] 0.51 mg. This dose is substantially more than the 2.5-mg adult dose recommended by the manufacturers. The maximal tolerated dose for albuterol was 0.21 [+ or -] 0.02 mg/kg or 8.12 [+ or -] 0.89 mg. With larger doses, major side effects from albuterol, such as symptomatic postural hypotension and extreme tremor, were significant enough to warrant the termination of phase 1 of the study in certain patients. In contrast, AMN had a wide therapeutic index, and only minimal side effects were noted at the maximal administered dose, 0.06 mg/kg. The mean maximal bronchodilator dose for AMN was 1.27 [+ or -] 0.13 mg or 0.033 [+ or -] 0.003 mg/kg. This is close to the maximal bronchodilator dose of 1.5 mg found for adult asthmatic patients by Pierce et al,16 but greater than the 0.05-mg dose recommended by Altounyan. (17) When maximal bronchodilator doses of AMN and albuterol were compared, the maximal absolute FEV[.sub.1] AMN achieved was 89 percent of the maximal FEV[.sub.1] albuterol achieved for phase 1 and 91 percent for phase 2. However, if the different time of maximum bronchodilation and the rising placebo baseline are taken into account, the AMN response was only 52.9 percent of that of albuterol. This difference in apparent response arises because the FEV[.sub.1] on the placebo day had risen only 5.9 percent at the time of maximum albuterol response compared with 19.1 percent at the time of maximal bronchodilator response to AMN. The rising baseline on placebo days may be attributed to the bronchodilator effect of theophylline and to circadian variation in pulmonary function. The maximal bronchodilator dose of albuterol produced equivalent bronchodilatation to the combination of albuterol and AMN. This latter finding was not expected since albuterol and AMN have different sites and mechanisms of action. The combination would therefore have been expected to have a greater bronchodilator effect than either drug alone. (1)
The duration of effect is another important characteristic of a bronchodilator. This was studied by comparing pulmonary function levels after administration of AMN or albuterol with those on placebo days. In all parameters studied, the albuterol response was significantly superior to the placebo response up to and including the fourth study hour, but not different from the placebo for the fifth or sixth study hours. The AMN response was significantly superior to the placebo response for all parameters studied up to and including the third study hour. It was better than the placebo response through the fourth study hour for PEFR and better than the placebo response through the sixth study hour for FEF25-75%. This was an interesting finding since many clinicians use the FEF25-75% as an indicator of small airway function and AMN is thought to have its major effect on the large airways. Similar results also were seen for the FEV[.sub.1]/FVC data (not shown) which was significantly better than placebo except at the fourth hour. In this study there was no significant difference between bronchodilatation with AMN and albuterol during the fifth or sixth hours. Thus, AMN alone in this study as opposed to earlier reports did not have a more prolonged effect than beta-adrenergic agonists. (16,18)
The combination of maximal bronchodilator doses of each medication gave a significant bronchodilator response for all pulmonary function parameters throughout the duration of testing. The superior response to the combination than to albuterol alone could be recognized as early as the third hour but did not become statistically significant until the fourth hour for the FEF25-75% and the sixth hour for PEFR and FEV[.sub.1]. Our findings suggest that combination therapy includes benefits from each medication since there is a greater duration of effect from the combination therapy than with albuterol alone, despite no difference in the maximal effect. The duration of effect also may be increased by increasing the medication doses. A further increase in albuterol dosage was not feasible in most patients because of side effects (nine of 17 patients). However, it is possible that larger doses of AMN than had been employed in phase 2 could be used since side effects were not limiting. With larger doses, the duration of action from AMN might have been longer since it has been demonstrated that duration of effect from other anticholinergic agents, such as glycopyrolate (19,20) and ipratropium bromide, (5) are dose-dependent. For glycopyrrolate, bronchodilation can last up to 12 h if a sufficient dose is administered. (20) The relative lack of benefit from the combination therapy (ipratropium bromide and albuterol) over albuterol alone in studies by Ruffin et al (21) and Boner et all could possibly be due to an inadequate dose of ipratropium bromide.
Individualization of medications is especially important in severe asthmatic patients. The manufacturer's recommended doses often are administered without titrating the medication to the individual patient. When mean data are examined, 200 [mu]g of albuterol through a metered dose inhaler has been shown to cause near maximal bronchodilatation, (16) but this dose is unlikely to achieve maximal possible bronchodilatation in many patients. (15) Instead of increasing the dose of beta-adrenergic agonists, additional medications are often added without establishing their efficacy.
The longer duration of the combination therapy may be helpful in the chronic asthmatic patient whose response to a beta-adrenergic agonist is of inadequate duration or in whom adverse effects prevent the use of larger doses. The addition of an anticholinergic medication also may be effective in the treatment of nocturnal asthma since oxitropium bromide provides beneficial effects. (22) However, before combination therapy can become accepted as standard care for either of these clinical situations, multiple-dose studies documenting the superiority of combination therapy need to be performed. The response to therapy must be reassessed on an ongoing basis since prolonged use of beta-adrenergic drugs, (23,24) atropine sulfate (25) and AMN (26) all may result in subsensitivity.
We conclude that AMN is an effective bronchodilator in some children with moderately severe to severe asthma. Overall the maximal AMN response was less than the albuterol response in all parameters studied and both drugs had a similar duration of action. However, AMN may be most useful in combination with optimal doses of albuterol since the combination may produce a more prolonged bronchodilator effect than albuterol alone. However, it is perhaps prudent to reserve routine use of anticholinergic therapy for those who do not adequately respond to an optimal conventional treatment regimen until more data become available documenting its effectiveness and safety during chronic therapy in children.
REFERENCES
1 Gross NJ, Skorodin MS. Anticholinergic, antimuscarinic bronchodilators. Am Rev Respir Dis 1984; 129:856-70
2 Storms WW, DoPico GA, Reed CE. Aerosol Sch 1000, an anticholinergic bronchodilator. Am Rev Respir Dis 1975; 111:419-22
3 Gross NJ. Sch 1000: a new anticholinergic bronchodilator. Am Rev Respir Dis 1975; 112:823-28
4 Easton PA, Jadue C, Dhingra S, Anthonisen NR. A comparison of the bronchodilating effects of a beta-2 adrenergic agent (albuterol) and an anticholinergic agent (ipratropium bromide), given by aerosol alone or in sequence. N Engl J Med 1986; 315:735-39
5 Baigelman W, Chodosh S. Bronchodilator action of the anticholinergic drug, ipratropium bromide (Sch 1000), as an aerosol in chronic bronchitis and asthma. Chest 1977; 71:324-28
6 Tashkin DP, Ashutosh K, Bleecker ER, Britt EJ, Cugell DW, Cummiskey JM, et al. Comparison of the anticholinergic bronchodilator ipratropium bromide with metaproterenol in chronic obstructive pulmonary disease: a 90-day multi-center study. Am J Med 1986; 81(suppl 5A):81-89
7 Cropp GJA. The role of the parasympathetic nervous system in the maintenance of chronic airway obstruction in asthmatic children. Am Rev Respir Dis 1975; 112:599-605
8 Groggins RC, Milner AD, Stokes GM. Bronchodilator effects of clemastine, ipratropium bromide, and salbutamol in preschool children with asthma. Arch Dis Child 1981; 56:342-44
9 Boner AL, De Stefano G, Niero E, Vallone G, Gaburro D. Salbutamol and ipratropium bromide solution in the treatment of bronchospasm in asthmatic children. Ann Allergy 1987; 58:54-58
10 Lenney W, Evans NAR Nebulized salbutamol and ipratropium bromide in asthmatic children. Br j Dis Chest 1986; 80:59-65
11 Lin MT, Lee-Hong E, Collins-Williams C. A clinical trial of the bronchodilator effect of SCH 1000 aerosol in asthmatic children. Ann Allergy 1978; 40:326-32
12 American Thoracic Society. Chronic bronchitis, asthma, and pulmonary emphysema: a statement by the committee on diagnostic standards for nontuberculous respiratory diseases. Am Rev Respir Dis 1961; 85:762-8
13 Newcomb R, Tashkin DP Hui KK, Conolly ME, Lee E, Dauphinee B. Rebound hyperresponsiveness to muscarinic stimulation after chronic therapy with an inhaled muscarinic antagonist. Am Rev Respir Dis 1985; 132:12-15
14 Suez D, Chai H. A standard method of intermittent inhaled therapy via a jet nebulizer. Ann Allergy 1986; 57:245-48
15 Nelson HS, Spector SL, Whitsett TL, George RB, Dwek JH. The bronchodilator response to inhalation of increasing doses of aerosolized albuterol. J Allergy Clin Immunol 1983; 72:371-75
16 Pierce RJ, Allen CJ, Campbell AH. A comparative study of atropine methyinitrate, salbutamol, and their combination in airways obstruction. Thorax 1979; 34:45 50
17 Altounyan REC. Variation of drug action on airway obstruction in man. Thorax 1964; 19:406-15
18 Elwood RK, Abboud RT. The short-term bronchodilator effects of fenoterol and ipatropium in asthma. J Allergy Clin Immunol 1982; 69:467-73
19 Walker FB IV Kaiser DL, Kowal MB, Suratt PM. Prolonged effect of inhaled glycopyrrolate in asthma. Chest 1978; 91:49-51
20 Schroeckenstein DC, Bush RK, Chervinsky P, Busse WW Twelve-hour bronchodilation in asthma with a single aerosol dose of the anticholinergic compound glycopyrrolate. J Allergy Clin Immunol 1988; 82:115-19
21 Ruffin RE, Fitzgerald JD, Rebuck AS. A comparison of the bronchodilator activity of Sch 1000 and salbutamol. J Allergy Clin Immunol 1977; 59:136-41
22 Coe CI, Barnes PJ. Reduction of nocturnal asthma by an inhaled anticholinergic drug. Chest 1986; 90:485-88
23 Nelson HS, Raine D Jr, Doner HC, Posey WC. Subsensitivity to the bronchodilator action of albuterol produced by chronic administration. Am Rev Respir Dis 1977; 116:871-78
24 Weber RW, Swith JA, Nelson HS. Aerosolized terbutaline in asthmatics: development of subsensitivity with long-term administration. J Allergy Clin Immunol 1982; 70:417-22
25 Mansfield LE, Vaughn TR, Haverly RW, Ting S. The development of subsensitivity to nebulized atropine sulfate. Ann Allergy 1986; 57:426-28
26 Vaughan TR, Bowen RE, Goodman DL, Weber RW, Nelson HS. The development of subsensitivity to atropine methyinitrate. Am Rev Respir Dis 1988; 138:771-74
Table 1 - Phase 1 Dosage Schedule
COPYRIGHT 1990 American College of Chest Physicians
COPYRIGHT 2004 Gale Group