Idiopathic pulmonary fibrosis (IPF) is a progressive, fatal lung disorder of unknown etiology. The consensus statement released by the American Thoracic Society and European Respiratory Society has provided guidelines for the diagnosis, evaluation, and management of patients with IPF. These guidelines suggest the use of conventional treatment options including therapy with corticosteroids and immunosuppressive agents. The guidelines statement acknowledged the fact that there is little good-quality evidence to support the safety and efficacy of such therapies in patients with IPF. The statement was published in 2000 and was based on an extensive review of the literature up to and including December 1998. The goal of this review is to reexamine the treatment recommendations of the guidelines statement in the context of data that has since become available.
Key words: clinical trials; idiopathic pulmonary fibrosis; treatment; usual interstitial pneumonia
Abbreviations: ACCP = American College of Chest Physicians; ATS = American Thoracic Society; DLCO = diffusing capacity of the lung for carbon monoxide; ERS = European Respiratory Society; IFN = interferon; IPF = idiopathic pulmonary fibrosis; LBW = lean body weight; NSIP = nonspecitic interstitial pneumonia
**********
Idiopathic pulmonary fibrosis (IPF) is a progressive, highly lethal disease of unknown etiology that is characterized by rapid fibrotic destruction of the lung. (1-3) On surgical biopsy specimens, IPF is associated with the histologic pattern referred to as usual interstitial pneumonia. (1,4) The prognosis for IPF patients is extremely poor, with a median survival generally reported as 2 to 3 years from the time of diagnosis. (5)
In 2000, the American Thoracic Society (ATS) and European Respiratory Society (ERS) released an international consensus statement (1) to define the diagnosis, evaluation, and management of patients with IPF. Recognizing the lack of large, randomized trials to define optimal treatment approaches for IPF patients, the ATS/ERS suggested treatment using therapy with corticosteroids in combination with either azathioprine or cyclophosphamide, for patients who were well-informed of the risks and benefits of treatment, and who "possess features consistent with a more likely favorable outcome." (1)
The corticosteroid/azathioprine treatment regimen comprised prednisone (or an equivalent) at a dose of 0.5 mg/kg lean body weight (LBW) per day orally for 4 weeks, 0.25 mg/kg LBW daily for 8 weeks, and then tapering to a dose of 0.125 mg/kg ideal body weight daily or 0.25 mg/kg LBW every other day, and azathioprine at doses of 2 to 3 mg/kg LBW per day to a maximum dose of 150 mg/d orally. The recommended dosing of azathioprine was a starting dose of 25 to 50 mg/d with increases in 25-mg increments every 7 to 14 days until the maximum dose was reached. (1)
The corticosteroid/cyclophosphamide regimen included corticosteroid therapy as described above, and cyclophosphamide at a dose of 2 mg/kg LBW to a maximum dose of 150 mg/d orally. The recommended dosing regimen for cyclophosphamide was a starting dose of 25 to 50 mg/d increasing gradually by 25-mg increments every 7 to 14 days until the maximum dose was reached. (1)
Corticosteroid therapy is usually tolerable, but adverse effects are common and can be disabling. Side effects associated with corticosteroid treatment include peptic ulcer disease, cataracts, hypertension, endocrine and metabolic alterations such as truncal obesity, moon face, hyperglycemia, hypokalemia, and impotence, musculoskeletal complications including osteoporosis, vertebral compression fracture and myopathy, and psychological changes such as euphoria, depression, or psychosis. (1)
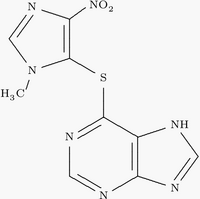
Cytotoxic therapy is also associated with numerous adverse effects. Cyclophosphamide use can lead to hemorrhagic cystitis and poses a risk of cardiotoxicity with high doses. (6) Azathioprine is considered to be less toxic than cyclophosphamide as it does not induce bladder injury and has less oncogenic potential. It can, however, induce hepatocellular injury and rash. (1,7) Both drugs are also associated with CI irritation and alopecia. (7-9) Since the use of either drug can lead to leukopenia, thrombocytopenia, or bone marrow suppression, the serial assessment of WBC and platelet counts is recommended (1,7) (Table 1).
The ATS/ERS recognized that responses to therapy might not be evident until the patient had received [greater than or equal to] 3 months of therapy. The guidelines, therefore, called for the continuation of combined therapy for at least 6 months unless complications or adverse events forced earlier termination. At the end of the 6-month treatment period, the patient's response to treatment could be assessed by the performance of repeat studies. (1)
The ATS/ERS committee suggested that drug therapy is not indicated for all patients and that the risk of complications of treatment must be weighed against the potential benefit. The committee also suggested that the response to treatment might be higher early in the course of the disease before irreversible fibrosis has occurred. They recommended that treatment be initiated at the first identification of clinical or physiologic evidence of impairment or the demonstration of decline in lung function. (1)
REVIEW OF IPF CLINICAL TRIALS
The role of pharmacologic intervention in the treatment of IPF has been evaluated in numerous clinical trials. However, as acknowledged in the ATS/ERS statement, (1) these studies have been limited by numerous factors including a lack of understanding of the natural history of the disease, variable study designs (including heterogeneous patient populations and variable study durations), differences in medication formulations, dosages, routes of administration and durations of treatment, lack of placebo control subjects, disputable diagnostic certainty, and variable assessment criteria and intervals between evaluations. (1)
Since the ATS guidelines statement, there has been one additional publication (10) on the risks and potential benefits of treatment with high-dose corticosteroids. This was a prospective study in which all 41 patients with IPF received steroids. (10) The first 24 patients were treated with the same dose of prednisone (100 mg/d) for 3 months. The other 17 patients received a lesser dose (60 mg/d) for the first month followed by 40 mg/d for the following 2 months. Therapeutic response was measured at 3 months using a composite score that included clinical, radiographic, and physiologic measures. (10) The results revealed somewhat greater mean total pathology scores and interstitial disease scores on CT scans in the 24 patients who received the higher dose of prednisone from the start of the study. All patients experienced at least one steroid-related adverse effect. Eleven of 41 patients (27%) responded to therapy, 19 (46%) remained stable, and 11 (27%) were nonresponders, (10) Nineteen patients (46%; high-dose group, 15 of 24 patients; lower dose group, 4 of 17 patients) died during the 3-year follow-up period. Survival was greatest among stable patients, followed by responders, then nonresponders, with statistically significant differences in the survival of nonresponders vs stable patients (p < 0.001), nonresponders vs responders (p = 0.02), and responders vs stable patients (p = 0.05).m The authors concluded that corticosteroid therapy was associated with substantial morbidity, and that patients who remained stable or improved had better survival times than patients who manifested disease progression. It appears somewhat paradoxical that the so-called "responders" did worse than the "stable" patients. This underscores our lack of understanding and inability to predict the natural history of disease in many patients with IPF. It is possible that the differences in the three groups represented the natural history of the disease and that there was no treatment effect. The fact that the nonresponders did worse is consistent with data showing that patients who manifest physiologic deterioration over the course of 6 to 12 months have a significantly worse prognosis than those whose condition remains stable or who improve their lung function. (5,11,12)
Since the ATS/ERS statement, there have been no additional publications on the utility of combination therapy with prednisone/azathioprine. It is worthwhile to reflect on the more recent of the two articles supporting this recommendation that are cited in the ATS/ERS statement. That article (13) was a prospective, double-blind, randomized, placebo-controlled study that compared combined therapy with prednisone/azathioprine with prednisone therapy alone in 27 IPF patients. Prednisone therapy was started at 1.5 mg/kg/d for 2 weeks followed by a taper to 20 rag/d, and azathioprine was administered at a daily dose of 3 mg/kg. Patients were evaluated at 1, 3, 6, 9, and 12 months for adverse effects and for response to therapy. The primary end points were the measurable change in lung function at 1 year and survival. (13) Improvement in lung function was defined as a [greater than or equal to] 10% improvement in FVC, a [greater than or equal to] 20% improvement in the diffusing capacity of the lung for carbon monoxide (DLCO), or [greater than or equal to] 10% improvement in resting alveolar-arterial oxygen pressure difference. (13) No statistically significant changes in pulmonary function were observed at 1 year. A comparison of survival curves for the two treatment groups by Cox regression model analysis showed no statistically significant differences. However, analysis based on adjustment for age showed a marginally significant survival advantage for the prednisone/azathioprine group. (13) Noteworthy is the fact that this article was published prior to the description and understanding of nonspecific interstitial pneumonia (NSIP) as a separate distinct clinical entity. (14) It therefore is quite possible that some of the patients in both groups had this disease, which would cloud the results, especially since the numbers in the study were so small. Inspection of the Kaplan-Meier survival curve from this study attests to any difference in survival between the two groups only being seen after about 4 years. Therefore, if there is any survival benefit related to this combination therapy, most patients will have died by the time any benefit might be manifested. The conclusion of the authors of this article (13) that a larger, randomized study was needed to confirm the efficacy of the prednisone/azathioprine combination therapy, unfortunately, remains unfilfilled.
The second cytotoxic agent suggested to be used in combination with steroids was cyclophosphamide. At the time of the ATS/ERS statement, (1) there was one randomized, controlled study of 43 IPF patients that compared treatment with alternate-day prednisolone therapy (at an initially high dose) to therapy with cyclophosphamide plus alternate-day low-dose prednisolone. (15) In the prednisolone-only group, prednisolone was administered at a dose of 60 mg daily for 1 month and then was reduced by 5 mg/wk to 20 mg on alternate days. Patients in the cyclophosphamide/prednisolone group received 100, 110, or 120 mg of cyclophosphamide daily plus 20 mg of prednisolone on alternate days. (15) Patients were assessed at 1 and 3 months after starting treatment, and subsequently at 3-month intervals for 2 years and every 6 months thereafter. Improvement was defined as a change from baseline in lung function, radiographic appearance, and breathlessness scores, while deterioration was defined as equivalent worsening of the three measurements. (15) Seven of 22 patients in the prednisolone group and 5 of 21 patients in the cyclophosphamide/prednisolone group showed improvement at one or more assessments. (15) After 3 years, 5 of 22 patients in the prednisolone group remained either stable or improved, as did 5 of 21 patients in the cyclophosphamide/prednisolone group. (15) An analysis of the time to failure of the first allocated treatment regimen or death showed an advantage to patients receiving cyclophosphamide/prednisolone (p < 0.05), possibly due to better lung volumes in this group at hospital admission. (15) A suggestion of improved survival time was detected among patients in the cyclophosphamide/ prednisolone group, but it was not significant (p > 0.1). At 3 years, 10 of 22 patients in the prednisolone group and 3 of 21 patients in the cyclophosphamide/prednisolone group had died; however, by the end of the study there had been 15 deaths in both groups. (15) The authors concluded that the combination of cyclophosphamide with prednisolone could be an alternative to high-dose prednisolone therapy alone, although both drugs were effective only in a small group of patients. However, any statement attesting to efficacy, even in a small group of patients, is difficult to support, with no overall survival benefit having been observed. Also, without a placebo control group, it is unknown whether any of the observations noted were within the realm of the natural history of the disease. This study also has the same historical problem as the azathioprine study, in that it was performed prior to our understanding and description of NSIP. It is not only likely, but highly probable that a significant number of the study subjects had NSIP. Indeed, five patients in each group (23%) had an underlying connective tissue disorder rather than true IPF as defined in the ATS statement.
There have been two additional studies over the last 6 years that have examined the utility of cyclophosphamide in IPF. The first of these studies (16) reported a series of 19 patients who were treated with cyclophosphamide alone after being tapered off steroid treatment. (16) Only 1 of the 19 patients was deemed to have had a sustained response. Whether this was treatment effect or the natural history of the disease cannot be answered without a control group. The authors appropriately concluded that cyclophosphamide is of limited efficacy in patients with IPF. The second study (17) was a retrospective study that compared survival times in a large group of patients treated with combined cyclophosphamide and corticosteroid therapy (n = 82) administered to untreated age-matched and baseline FVC (percent predicted)-matched patients (n = 82). (17) Treatment consisted of corticosteroids (prednisone or its equivalent at an initial dose of 0.5 to 1.0 mg/kg) with the addition of cyclophosphamide (2 mg/kg/d orally at a total dose < 200 mg/d). (17) There was no difference in survival time from the time of the initial visit between patients treated with the combination of cyclophosphamide and corticosteroids and untreated patients. A subgroup analysis of patients with an FVC of [greater than or equal to] 60% predicted similarly failed to show a difference in outcomes between the two groups. These authors suggested that chronic inflammation plays only a minimal role in the progression of IPF, and they emphasized the importance of weighing the risks and benefits of this and other treatment approaches.
Two recent reviews published in the Cochrane Database of Systematic Reviews evaluated recent trials of corticosteroids and immunomodulatory agents in the treatment of IPF. Richeldi et al (18) reviewed 15 randomized controlled trials and controlled clinical trials of therapy with corticosteroids alone. On analysis, all 15 studies were excluded due to inadequate methodologies. This review (18) concluded that there was no evidence for the efficacy of corticosteroid treatment in patients with IPF and suggested that therapies with immunomodulatory rather than antiinflammatory or immunosuppressive effects may be a more promising approach in the treatment of IPF. This hypothesis was explored in a review of clinical trials utilizing noncorticosteroid immunosuppressive, antifibrotic, or immunomodulatory agents in patients with histologic evidence of IPF. (4) Of 59 studies identified, only 3 (including Raghu et al, (13) Ziesche et al, (3) and Douglas et al (19)) were considered suitable for inclusion in a meta-analysis. The authors found that since each high-quality trial used a different agent (ie, azathioprine, colchicine, and interferon [IFN]-[gamma]-lb), meaningful comparisons were not possible. They concluded that, despite the large number of clinical trials identified, there was little good-quality information regarding the efficacy of immunosuppressive, antifibrotic, or immunomodulatory agents in the management of IPF, and that there is little evidence to support the routine use of noncorticosteroid agents in the management of IPF. (4) This conclusion is in accordance with the ATS/ERS guidelines, (1) which had caveats attesting to these same limitations, and with acknowledgment that their recommendations were largely based on expert opinion.
The agent that has drawn most interest over the last 5 years as a potential therapy for IPF has been IFN-[gamma]-lb. IFN-[gamma]-lb inhibits the proliferation of lung fibroblasts in vitro and down-regulates transforming growth factor-[beta]1-mediated transcription of profibrotic molecules. Transforming growth factor-[beta]1 has been shown to cause fibrosis in animals. (3) Clinical interest in the drug was sparked by a small pilot study (3) that purported to show that IFN-[gamma]-lb was effective in patients with IPF who had been resistant to 3 months of therapy with high-dose glucocorticoids. In this study, the combination therapy of low-dose prednisolone and IFN-[gamma]-1b administered to nine patients (200 [micro]g, three times per week, subcutaneously) was compared to therapy with low-dose prednisolone alone in a control group of nine patients. Lung function was evaluated at baseline and after 3, 6, 9, and 12 months of treatment. (3)
At the end of the study, there appeared to be evidence of improvement in physiologic indices among patients receiving IFN-[gamma]-lb/prednisolone relative to those receiving prednisone alone, suggesting that the combination therapy with IFN-[gamma]-1b/ prednisolone possibly not only arrested but actually reversed the disease process.
This study provided the impetus for a large, randomized, double-blind, multinational study of IFN-[gamma]-1b efficacy in 330 patients with IPF who were unresponsive to corticosteroid therapy. (20) Eligible patients were between 20 and 79 years of age, and had experienced clinical symptoms of IPF for at least 3 months and worsening disease over the past year. Patients were randomized to receive IFN-[gamma]-lb (200 [micro]g, three times per week, subcutaneously) or placebo for a minimum of 48 weeks. The primary efficacy end point was progression-free survival, which was defined as the time to death or disease progression, with progression defined as a decrease of at least 10% in the predicted FVC or an increase of at least 5 mm Hg in the resting alveolar-arterial oxygen pressure difference. (20) One hundred sixty-two patients received IFN-[gamma]-1b and 168 received placebo, with a mean duration of treatment of 383 days in the IFN-[gamma]-1b group and 374 days in the placebo group. Primary efficacy analysis revealed no significant differences in the duration of progression-free survival between the two groups. However, with the physiologic end points extracted, in the intent-to-treat analysis there was a trend toward enhanced survival observed in patients who had been treated with IFN-[gamma]-lb (p = 0.08). (20) This difference was more apparent in treatment-adherent patients (ie, those who received at least 80% of the scheduled doses of study drug), who showed an absolute reduction in the risk of death of 9% in the IFN-[gamma]-1b group compared to the placebo group, and a relative risk reduction of 66% (p = 0.02). Among patients with an FVC above the median of the group (FVC > 62% predicted), there also appeared to be a survival benefit for the IFN-[gamma]-1b group (4% mortality rate vs 12% for the placebo group; p = 0.04). There was no difference between the two groups in any of the measured physiologic indices, including the FVC, single-breath DLCO, or the alveolar-arterial oxygen pressure difference. The results of this study have generated some controversy since, although it was a study with negative results based on its design and chosen end points, the apparent mortality benefit in the subgroup analyses raises the notion of a true treatment effect in patients with less advanced disease. This study continues to provide valuable information on the natural history of the disease. It has raised questions about our conventional physiologic measures as adequate predictors of mortality, since 43% of the deaths occurring during the course of the study were without prior physiologic evidence of disease progression. A follow-up study is currently under way to further assess this possible mortality benefit of IFN-[gamma]-1b therapy in patients with less advanced disease, as defined by an FVC of > 55% predicted and a DLCO of > 35% predicted.
METHODOLOGY AND GRADING FOR EVIDENCE REVIEW AND GUIDELINE DEVELOPMENT
As more information and study results regarding therapies for IPF become available, it will be important to integrate the information and place new study results in the appropriate context. The American College of Chest Physicians (ACCP) recently developed a set of two-tiered, evidence-based, clinically relevant guidelines (21) for the diagnosis and treatment of pulmonary hypertension that can be applied to the evaluation of therapeutic trials in IPF. The ACCP expert panel identified and evaluated clinical trial evidence on each of five topics for review and analysis. Literature search results were reviewed by physicians with methodological and content area expertise. The expert panel produced recommendations on the five topics, each related to a distinct set of patient-management issues. The recommendations were graded using the ACCP Health and Science Policy Grading System, which is based on the following two components: the quality of the evidence; and the net benefit of the therapeutic or diagnostic procedure. Evidence was graded according to the methodologies used in the study. Net benefit was based on the risk/benefit ratio for the patient population as defined in the recommendation and not for individual patients. (21) The level of recommendation was defined by the interaction of the strength of the evidence and the net benefit (Table 2).
If a similar systematic approach was applied to the therapies available for IPF, it would allow previously suggested therapeutic regimens and future therapies to be appropriately ranked. With the notable, well established side effect profile of steroids and cyto-toxic agents, the concept of net benefit would appear to necessitate a significant treatment effect of these drugs for IPF. Accordingly, it is interesting to speculate how the ATS/ERS recommendations for therapy might be graded with the currently available data.
MONITORING THE CLINICAL COURSE AND RESPONSE TO THERAPY IN IPF
Because of marked variability in the extent and rate of disease progression from one individual to the next, it is difficult to monitor the clinical responses to therapy. Standardization of the clinical monitoring of IPF has been hampered by the lack of uniformity in the pulmonary function parameters used to differentiate responders from nonresponders. In some studies, increases of 10 to 15% from pretreatment baseline have been considered favorable responses. There are data to support this concept, specifically those patients who manifest a serial increase in their FVC levels of 10% have been shown to have a better prognosis. (3,12) Whether or not this is a treatment effect or is indicative of a subgroup of patients who will have a favorable response, independent of any therapies, remains uncertain. In other studies, a lack of change or stabilization among patients previously exhibiting deterioration has been considered a favorable response. (1) While such patients appear to have a better prognosis than those who manifest a serial decrement, they still are at risk of dying due to their disease. In addition, as previously alluded to, 43% of the deaths in the 2004 study by Raghu et al (20) occurred prior to meeting the predefined criteria for disease progression. Thus, these studies demonstrate that clinical measures of the stability of lung function do not necessarily mirror disease stability.
It is apparent, therefore, that more refined clinical tools are needed to monitor and predict the disease course. The 6-min walk test is one such tool that has been shown to provide useful prognostic information. (22) Serial changes in 6-min walk test parameters might provide additional prognostic information and prove to be a more accurate gauge of treatment effect, but this remains to be validated. Composite scores utilizing clinical criteria, radiographic scores, pathologic features, and physiologic criteria have been incorporated into various models of survival. (23-25) These might also prove to be useful in monitoring the response to therapy. However, complex models are difficult and impractical in most clinical settings. (26)
The ATS/ERS recognized that responses to therapy might not be evident until the patient had received [greater than or equal to] 3 months of therapy. The guidelines, therefore, called for the continuation of combined therapy for at least 6 months unless complications or adverse events forced an earlier termination. At the end of the 6-month treatment period, the patient's response to treatment could be assessed by the performance of repeat studies. (1) However, it is possible that there may be occult salutary effects of various agents that are not manifested with clinical, radiographic, or physiologic improvement. (27) The discontinuation of therapy based on a lack of perceived improvement is an issue that remains unresolved and will require further study, including the identification of biomarkers of disease activity.
LUNG TRANSPLANTATION
In light of the dire prognosis associated with IPF, the ATS/ERS (1) recommended that lung transplantation be considered for IPF patients who experience progressive physiologic deterioration despite optimal medical management and who meet the established criteria. With growing waiting lists and median waiting list times as long as 4 years, earlier listing appears to be prudent. Although physiologic deterioration clearly carries a worse prognosis, by only recommending transplant listing for these patients, those who are physiologically stable risk missing the window of opportunity for transplantation. With regard to optimal medical management, there remains no therapy that has been definitively shown to alter the natural history and disease course in IPF patients. Therefore, if patients appear to be appropriate candidates, they should be referred for transplantation consideration and possibly listed, rather than waiting and assessing them for a response to therapy.
A new allocation system for lungs has been accepted and has been in effect since April 2005. (28) The new system assigns a lung allocation score to each patient based on the difference between a patient's projected transplant benefit and the patient's waitlist urgency. This new system should benefit IPF patients who currently are the most likely to die while awaiting a transplant. How this will impact the need for earlier listing remains to be determined. Until the impact of this new allocation system is fully assimilated and assessed, early referral to a local transplant center will remain the prudent course of action. Unfortunately, the prognosis following lung transplantation remains mostly unchanged, with a 5-year survival rate of 40% in transplant recipients who have IPF. (29)
CONCLUSIONS
The limitations of therapeutic trials in IPF highlight the importance of quality evidence, and the need for additional and better clinical trials to investigate the safety and efficacy of treatment options. The suggestion that early-stage patients are more responsive to treatment indicates a need for additional future studies that are focused on patients in the early disease stages before fibrosis has become irreversible. Additional population-based studies are needed to obtain epidemiologic data and to gain information about the influence of occupational, environmental, and genetic factors in IPF. Prospective, double-blind, randomized, placebo-controlled, multicenter studies will require large numbers of well-matched patients to adequately evaluate future potential therapies while minimizing any potential bias from heterogeneous disease expression. These high-quality studies would provide the greatest opportunity to gain a better understanding of the natural history of IPF and to allow for the identification of effective therapeutic regimens.
REFERENCES
(1) American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment; international consensus statement-American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med 2000; 161:646-664
(2) Selman M, Carrillo G, Salas J, et al. Colchicine, D-penicillamine, and prednisone in the treatment of idiopathic pulmonary fibrosis: a controlled clinical trial. Chest 1998; 114:507-512
(3) Ziesche R, Hofbauer E, Wittmann K, et al. A preliminary study of long-term treatment with interferon gamma-1b and low-dose prednisolone in patients with idiopathic pulmonary fibrosis. N Engl J Med 1999; 341:1264-1269
(4) Davies HR, Richeldi L, Waiters EH. Iminunomodulatory agents for idiopathic pulmonary fibrosis. Cochrane Database Syst Rev (database online). Issue 3, 2003
(5) Collard HR, King TE Jr, Bartelson BB, et al. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2003; 168: 538-542
(6) Goldberg MA, Antin JH, Guinan EC, et al. Cyclophosphamide cardiotoxicity: an analysis of dosing as a risk factor. Blood 1986; 68:1114-1118
(7) National Jewish Medical and Research Center. Interstitial lung disease. Available at: http://www.nationaljewish.org/ a4.html. Accessed October 26, 2004
(8) IMURAN (azathioprine) [package insert]. San Diego, CA: Prometheus Laboratories Inc, 2003
(9) Lynch JP, Wurfel M, Flaherty K, et al. Usual interstitial pneumonia. Available at: http://www.medscape.com/viewartitle/410887_print. Accessed October 26, 2004
(10) Flaherty KR, Toews GB, Lynch JP III, et al. Steroids in idiopathic pulmonary fibrosis: a prospective assessment of adverse reactions, response to therapy, and survival Am J Med 2001; 110:326-328
(11) Latsi PI, DuBois R, Nicholson G, et al. Fibrotic idiopathic interstitial pneumonia: the prognostic value of longitudinal functional trends. Am J Respir Crit Care Med 2003; 168:531-537
(12) Flaherty K, Mumford J, Murray S, et al. Prognostic implications of physiologic and radiographic changes in idiopathic interstitial pneumonia. Am J Respir Crit Care Med 2003; 168:543-548
(13) Raghu G, Depaso WJ, Cain K, et 'al. Azathioprine combined with prednisone in the treatment of idiopathic pulmonary fibrosis: a prospective double-blind, randomized, placebo-controlled clinical trial. Am Rev Respir Dis 1991; 144:291-296
(14) Katzenstein AL, Myers JL. Nonspecific interstitial pneumonia/fibrosis: histologic features and clinical significance. Am J Surg Pathol 1994; 18:136-147
(15) Johnson MA, Kwan S, Snell NJ, et al. Randomized controlled trial comparing prednisolone alone with cyclophosphamide and low dose prednisolone in combination in cryptogenic fibrosing alveolitis. Thorax 1989; 44:280-288
(16) Zisman DA, Lynch JP, Toews GB, et al. Cyclophosphamide in the treatment of idiopathic pulmonary fibrosis: a prospective study in patients who failed to respond to corticosteroids. Chest 2000; 117:1619-1626
(17) Collard HR, Ryn JH, Douglas WW, et al. Combined corticosteroid and cyclophosphamide therapy does not alter survival in idiopathic pulmonary fibrosis. Chest 2004; 125:2169-2174
(18) Richeldi L, Davies HR, Ferrara G, et al. Corticosteroids for idiopathic pulmonary fibrosis. Cochrane Database Syst Rev (database online). Issue 3, 2003
(19) Douglas WW, Ryu JH, Swensen SJ, et al. Colchicine versus prednisone in the treatment of idiopathic pulmonary fibrosis: a randomized prospective study; Members of the Lung Study Group. Am J Respir Crit Care Med 1998; 158:220-225
(20) Raghu G, Brown KK, Bradford WZ, et 'al. A placebo-controlled trial of interferon [gamma]-1b in patients with idiopathic pulmonary fibrosis. N Engl J Med 2004; 350:125-133
(21) McCrory DC, Lewis SZ. Methodology and grading for pulmonary hypertension evidence review and guideline development. Chest 2004; 126(suppl):11S-13S
(22) Lama VN, Flaberty KR, Toews GB, et al. Prognostic value of desaturation during 6-minute walk test in idiopathic interstitial pneumonia. Am J Respir Crit Care Med 2003; 168:1084-1090
(23) King TE, Tooze JA, Schwarz MI, et al. Predicting survival in idiopathic pulmonary fibrosis: scoring system and survival model. Am J Respir Crit Care Med 2001; 164:1171-1181
(24) Wells AU, Desai SR, Rubens MB, et al. Idiopathic pulmonary fibrosis: a composite index derived from disease extent observed by computed tomography. Am J Respir Crit Care Med 2003; 167:962-969
(25) Mogulkoc N, Brutsche MH, Bishop PW, et al. Pulmonary function in idiopathic pulmonary fibrosis and referral for lung transplantation. Am J Respir Crit Care Med 2001; 164:103-108 26 Perez A, Rogers RM, Dauber JH. The prognosis of idiopathic pulmonary fibrosis. Am J Respir Cell Mol Biol 2003; 29:S19-S26
(27) Strieter RM, Starko KM, Enelow RI, et al. Idiopathic Pulmonary Fibrosis Biomarkers Study Group: effects of interferon-[gamma]1b on biomarker expression in patients with idiopathic pulmonary fibrosis Am J Respir Crit Care Med 2004; 170: 133-140
(28) United Network for Organ Sharing. News release. Available at: http://www.unos.org/SharedContentDocuments/Lung Policy_Release.doc. Accessed January 13, 2005
(29) The International Society for Heart and Lung Transplantation. Heart/Lung Transplant Registry. Available at: http://www. ishlt.org/registries/slides.asp. Accessed December 20, 2004
* From the Lung Transplant and Advanced Lung Disease Programs, Inova Fairfax Hospital, Falls Church, VA.
Dr. Nathan has received speaking honoraria from InterMune. Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Steven D. Nathan, MD, FCCP, Heart and Lung Transplant Center, Inova Heart and Vascular Institute, 3300 Gallows Rd, Falls Church, VA, 22042: e-mail: Steven.nathan@inova.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group