Abstract
Background: The safety of biologic agents for psoriasis treatment is of particular importance in patient groups at higher risk for adverse events. We assessed the safety and efficacy of alefacept in elderly, obese, and diabetic patients with moderate to severe chronic plaque psoriasis by integrating data from phase 2 and 3 clinical studies and their extensions.
Observations: Ninety-nine elderly, 652 obese, and 122 diabetic patients received at least 1 course of alefacept. In each cohort, accidental injury, headache, and pharyngitis were among the most common adverse events; infections were primarily common colds; and malignancies were mostly skin carcinomas. No opportunistic infections were reported. Safety was maintained over repeated courses. The safety profile of alefacept in each cohort was consistent with that of the overall population; however, additional data are needed to confirm our findings in the elderly and diabetic subgroups in the later courses due to the limited sample sizes. In course 1, 24% to 33% of patients achieved 75% or greater improvement in Psoriasis Area and Severity Index (PASI) at any time, with further enhancement of benefit with subsequent courses (eg, course 3, 41% to 58%).
Conclusions: Alefacept was well-tolerated and effective in elderly, obese, and diabetic patients with psoriasis.
Introduction
Psoriasis is a relapsing and lifelong skin disease with substantial negative impact on patient quality of life. (1,2) Psoriasis affects between 0.5% and 2.5% of the population worldwide. (3) Because of the chronic nature of psoriasis and the comparable life expectancies between those affected and the general population, the prevalence of the disease increases with age. (4) Although epidemiological data assessing the prevalence of psoriasis in the elderly are sparse, prevalence rates ranging from 3% to 10% have been reported. (4) As the elderly population increases, the number of cases of psoriasis is expected to increase.
Elderly patients may be particularly susceptible to the side effects associated with conventional systemic psoriasis therapies. (4,5) Comorbidities may also limit the use of some of these therapeutic options. Among the most common comorbidities that are diagnosed in patients with psoriasis are obesity, diabetes, hypertension, and heart failure. (3,6) For example, in a large database of more than 40,000 patients, the occurrence of each of these diseases was approximately 1.5 to 2 times more common in patients with psoriasis than in those without psoriasis, after adjusting for age and gender. (6) Both obese and diabetic patients have an increased risk for liver disease and thus added caution must be exercised when using methotrexate in these subpopulations. (7) The significant association of psoriasis with co-existing obesity, diabetes, and cardiovascular problems, including hypertension, (6) would warrant additional monitoring during cyclosporine therapy.
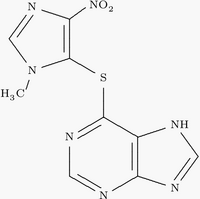
In order to address some of the limitations of traditional systemic psoriasis therapies, biologic agents that are designed to target the underlying pathophysiologic mechanisms of psoriasis have been developed. These agents may prove to offer patients a better safety profile than conventional systemic therapies; however, several adverse events, including serious infection, malignancy, and autoantibody formation, have been attributed to their use to date. (8) Data gained during ongoing clinical experience with these relatively new agents may help to more clearly define their safety profile; this information is of particular importance in patient groups with a higher risk for adverse events. In the present analysis, clinical study data were integrated to evaluate the safety and efficacy of alefacept in special patient populations including those who were elderly, obese, or diabetic.
Methods
Institutional review boards approved all study protocols. Written informed consent was obtained from all patients, and the studies were conducted in accordance with the Declaration of Helsinki and International Conference on Harmonisation guidelines.
Patients
This analysis included patients who participated in any of 9 multicenter, randomized, phase 2 and 3 clinical studies (and their extensions) that assessed the safety and efficacy of alefacept for the treatment of chronic plaque psoriasis. (9-13) In general, inclusion criteria encompassed patients who were at least 16 years of age and had chronic plaque psoriasis for at least 12 months' duration that involved at least 10% of body surface area. Patients were required to have a CD4+ lymphocyte count above 400 cells/[micro]L and to have had no serious local infection (eg, cellulitis, abscess) or systemic infection (eg, pneumonia, septicemia) within 3 months prior to the first dose of study drug. Patients with a history of malignancy, other than basal cell carcinomas or 3 or fewer cutaneous squamous cell carcinomas, were excluded. The use of phototherapy, systemic retinoids, systemic steroids, systemic fumarates, immunosuppressants (eg, methotrexate, cyclosporine, azathioprine, thioguanine), and high-potency corticosteroids was prohibited within 4 weeks prior to study drug administration and throughout the studies. The use of moderate-potency topical corticosteroids, vitamin D analogs, keratolytics, and coal tar was not allowed within 2 weeks prior to study drug administration and throughout the studies, except on the scalp, palms, groin, and soles.
For the purpose of analysis, elderly patients were at least 65 years of age at the time of the first dose, obese patients had a body mass index of 30 kg/[m.sup.2] or greater, and diabetic patients had a prior history of diabetes. A psoriasis patient may have had more than 1 comorbidity and thus would have been included in multiple cohorts.
Dosing
Patients received a variety of alefacept doses. In the phase 2 studies, patients generally received alefacept 0.025 mg/kg, 0.075 mg/kg, 0.15 mg/kg, or 7.5 mg by intravenous (IV) injection once weekly for 12 weeks. The phase 3 studies used intramuscular (IM) doses of 10 mg or 15 mg and an IV dose of 7.5 mg, each of which was administered once weekly for 12 weeks. The 12-week treatment period was followed by a treatment-free observation period of at least 12 weeks; both phases defined a course of therapy. Some patients received subsequent courses of alefacept as part of the original protocol or as part of an extension phase.
Safety Assessments
Data from all 9 phase 2 and 3 studies (and their extensions) and all dose groups were integrated for the analysis of safety. Treatment-emergent adverse events were monitored and assessed for severity throughout the studies. For patients in re-treatment studies, adverse events were collected during monthly interim visits between courses of alefacept. The period of time in interim visits ranged from 1 month to more than 1 year. Particular attention was focused on assessments of any new or ongoing viral, bacterial, or fungal infections and the incidence of malignancies. The incidence of infections was also stratified according to CD4+ lymphocyte counts (<250/[micro]L vs [greater than or equal to]250/[micro]L) and CD8+ lymphocyte counts (<100/[micro]L vs [greater than or equal to]100/[micro]L).
Efficacy Assessments
The 2 phase 3 studies and their extensions were included in the analysis of efficacy. Efficacy was assessed using the Psoriasis Area and Severity Index (PASI) and the Physician Global Assessment (PGA). The PASI is determined using a formula that includes lesion severity weighted by the proportion of body surface involved, resulting in a score ranging from 0 to 72. (14) The percentage of patients with a 75% or greater reduction (improvement) from baseline in PASI at any time (PASI 75) was a clinical endpoint. Since PASI was evaluated over all IV but not IM courses, data from the IV studies only were included in the PASI analysis. The PGA used a 7-point scale to assess the overall extent of psoriatic involvement ranging from 0 (clear) to 6 (very marked plaque elevation, scaling, or erythema). The percentage of patients with a score of 0 or 1 on the PGA ("clear" or "almost clear") at any time was a clinical endpoint. The PGA was evaluated over all IV and IM courses and thus data from all studies and across all dose groups were integrated for the PGA analysis.
Results
Patients
The safety population comprised 99 elderly patients, 652 obese patients, and 122 diabetic patients who received at least 1 course of alefacept. In course 1, the PASI analysis comprised 46 elderly, 273 obese, and 51 diabetic patients, and the PGA analysis included 92 elderly, 469 obese, and 100 diabetic patients.
Safety
Table 1 summarizes those adverse events that were reported in at least 10% of alefacept-treated patients in the first course. For all 3 patient cohorts, the most commonly reported events were accidental injury, headache, pharyngitis, rhinitis, and infection. Overall adverse events rates tended to decrease with each subsequent course of alefacept. Similarly, across the 3 patient subgroups, serious adverse event rates ranged from 6% to 11% in course 1 and from 5% to 8% in courses 2 and 3, with no occurrences in course 4 (data not displayed in Table 1). These events included diabetes mellitus, cholelithiasis, cardiovascular events, and malignancies. The incidences of cardiovascular events observed in our study population are within the expected age- and gender-based ranges. (15) The vast majority of serious adverse events were judged to be unrelated to the study drug.
Infections were reported in 11% to 14% of patients in the 3 cohorts during the first course of alefacept (Table 1). As in the overall patient population, the vast majority of events coded to the term "infection" were common colds. The most frequent event coded to the term "infection" was nasopharyngitis, accounting for approximately 60% to 70% of all infections across the 3 patient subgroups. No opportunistic infections were reported in any patient. Serious infections were infrequent. During the first course of alefacept, serious infections were reported in 0%, 1.1%, and 1.6% of elderly, obese, and diabetic patients, respectively (Table 2). There was no apparent increase in the frequency of serious infections with repeated treatment courses. In addition, there was no apparent association of infections with CD4+ lymphocyte counts, as 15 (26%) elderly, obese, or diabetic patients with CD4+ counts <250 cells/[micro]L developed infections during the first course of treatment, compared with 316 (47%) elderly, obese, or diabetic patients with CD4+ counts [greater than or equal to]250 cells/[micro]L. Results were consistent across all 3 cohorts. Similarly, there was no apparent association between infections and CD8+ lymphocyte counts (<100 cells/[micro]L vs [greater than or equal to]100 cells/[micro]L) in any cohort.
In course 1, malignancies included skin carcinoma (n = 3), skin melanoma (n = 2), and prostatic carcinoma (n = 1) among elderly patients; skin carcinoma (n = 5), carcinoma not specified (n = 2), and prostatic carcinoma (n = 1) among obese patients; and skin carcinoma (n = 1) among diabetic patients (Table 2). There was no indication that the risk of malignancy increased with repeated treatment courses. In the elderly cohort, a 68-year-old female with a 64-year history of chronic plaque psoriasis and previous treatment with methotrexate, retinoids, and psoralen/ultraviolet A phototherapy was diagnosed with a follicular cell lymphoma during her second course of alefacept. The patient received 17 total doses of alefacept prior to the diagnosis.
Efficacy
Alefacept was associated with substantial clinical improvements in the elderly, obese, and diabetic subgroups (Figures 1A and 1B). In course 1, the degree of clinical improvement among patients receiving alefacept was numerically superior to placebo across all 3 cohorts. Between 24% and 33% of alefacept-treated patients achieved a PASI 75 at any time during the first course, with 17% to 26% achieving a PGA of "clear" or "almost clear." The benefits of an initial course of alefacept were generally enhanced with subsequent treatment courses (Figures 1A and 1B). For example, among those who received 3 courses of alefacept, 41% to 58% of patients in the 3 cohorts achieved a PASI 75 and 33% to 37% achieved a PGA of "clear" or "almost clear."
Discussion
Based on their safety record and demonstrated efficacy and quality-of-life improvements, biologic therapies are playing an increasingly important role in the treatment of psoriasis. (16,17) Expanded clinical experience following the approval of alefacept in January 2003 has allowed for the continued collection of data on the safety profile of this agent. The current subanalyses suggest that the type, frequency, and severity of adverse events reported among elderly, obese, and diabetic patients are similar to those observed among all psoriasis patients treated with alefacept in randomized clinical studies. (9-13,18) Additional data are needed to confirm our findings in the elderly and diabetic patient cohorts in the later courses due to the limited sample sizes.
The overall incidence of serious adverse events was relatively low, considering that the analyzed population had a number of risk factors for comorbidities, such as hypertension and coronary artery disease, and the vast majority of those that did occur were judged to be unrelated to study medication. Notably, the present analysis provides evidence that multiple courses of alefacept are not associated with increased adverse safety consequences in the geriatric, diabetic, and obese cohorts studied. Thus, alefacept could be considered for the long-term management of psoriasis in higher-risk patient populations, those who are particularly sensitive to the adverse effects of long-term conventional systemic therapy. (19)
Our results also suggest that alefacept provides clinically significant efficacy among these patient subgroups, producing rates of response similar to that seen for the overall patient population; 28% to 33% of patients achieved PASI 75 and 23% to 24% achieved a PGA of "clear" or "almost clear" in the phase 3 trials, (10,12) In the current analysis, obese patients tended to have slightly lower PASI 75 and PGA responses after the first course of therapy (24% and 17%, respectively) compared with elderly (30% and 23%) or diabetic (33% and 26%) patients. However, with subsequent courses of therapy, efficacy among obese patients progressively improved and tended to "catch up" to the other cohorts.
In summary, alefacept is a well-tolerated and effective treatment for psoriasis in special populations including elderly, obese, and diabetic patients. These data are particularly relevant given that safety becomes more of a concern as a patient ages and that a high clustering of comorbidities is common in the psoriasis population.
[FIGURE 1 OMITTED]
Disclosure: Dr. Gottlieb is a consulting investigator and speaker for Biogen Idec. Dr. Boehncke is a member of the German Amevive Advisory Board and received honoraria from Biogen Idec as a speaker. Dr. Darif is employed by Biogen Idec. Acknowledgement: This analysis and the clinical trials were funded by Biogen Idec, Inc., Cambridge, Mass, USA.
References
1. Krueger G, Koo J, Lebwohl M, et al. The impact of psoriasis on quality of life. Results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137:280-284.
2. Mukhtar R, Choi J, Koo JY. Quality-of-life issues in psoriasis. Dermatol Clin. 2004;22:389-395.
3. Christophers E. Psoriasis--epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314-320.
4. Yosipovitch G, Tang MB. Practical management of psoriasis in the elderly. Epidemiology, clinical aspects, quality of life, patient education and treatment options. Drugs Aging. 2002; 19:847-863.
5. Boffa MJ, Chalmers RJ. Methotrexate for psoriasis. Clin Exp Dermatol. 1996;21:399-408.
6. Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol. 1995;32:982-986.
7. Lebwohl M, Ali S. Treatment of psoriasis. Part 2. Systemic therapies. J Am Acad Dermatol. 2001;45:649-661.
8. Callen JP. New psoriasis treatments based upon a deeper understanding of the pathogenesis of psoriasis vulgaris and psoriatic arthritis: a personal appraisal of their use in practice. J Am Acad Dermatol. 2003;49:351-356.
9. Ellis CN, Krueger GG, for the Alefacept Clinical Study Group. Treatment of chronic plaque psoriasis by selective targeting of memory effector T lymphocytes. N Engl J Med. 2001;345:248-255.
10. Krueger GG, Papp KA, Stough DB, et al. A randomized, double-blind, placebo-controlled phase III study evaluating efficacy and tolerability of 2 courses of alefacept in patients with chronic plaque psoriasis. J Am Acad Dermatol. 2002; 47:821-833.
11. Lowe NJ, Gonzalez J, Bagel J, et al. Repeat courses of intravenous alefacept in patients with chronic plaque psoriasis provide consistent safety and efficacy. Int J Dermatol. 2003;42:224-230.
12. Lebwohl M, Christophers E, Langley R, et al. An international, randomized, double-blind, placebo-controlled phase 3 trial of intramuscular alefacept in patients with chronic plaque psoriasis. Arch Dermatol. 2003;139:719-727.
13. Gordon KB, Langley RG. Remittive effects of intramuscular alefacept in psoriasis. J Drugs Dermatol. 2003;6:624-628.
14. Fredriksson T, Pettersson U. Severe psoriasis--oral therapy with a new retinoid. Dermatologica. 1978;157:238-244.
15. Thom TJ, Kannel WB, Silbershatz H, D'Agostino RB Sr. Cardiovascular diseases in the United States and prevention approaches. In: Fuster V, Alexander RW, O'Rourke RA, eds. Hurst's The Heart. 10th ed. New York, NY: McGraw-Hill; 2001.
16. Callen JP, Krueger GG, Lebwohl M, et al. AAD consensus statement on psoriasis therapies. J Am Acad Dermatol. 2003;49:897-899.
17. Sterry W, Barker J, Boehncke WH, et al. Biological therapies in the systemic management of psoriasis: International Consensus Conference. Br J Dermatol. 2004;151(suppl 69):3-17.
18. Data on file, Biogen Idec.
19. Ashcroft DM, Li Wan Po A, Griffiths CE. Therapeutic strategies for psoriasis. J Clin Pharm Ther. 2000;25:1-10.
Address for Correspondence
Alice B. Gottlieb MD PhD
UMDNJ-Robert Wood Johnson
Medical School
51 French Street
New Brunswick, NJ 08901-0019
Phone: 732-418-8479
e-mail: gottliab@umdnj.edu
Alice B. Gottlieb MD PhD, (a) Wolf-Henning Boehncke MD, (b) Mohamed Darif PhD (c)
a. UMDNJ-Robert Wood Johnson Medical School, New Brunswick, NJ
b. Department of Dermatology, Johann Wolfgang Goethe University, Frankfurt am Main, Germany
c. Biogen Idec, Inc., San Diego, CA
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group