Atopic dermatitis affects up to 20 percent of Americans and is the most common chronic skin disease in children. (1) The majority of patients are younger than 30 years, with 90 percent reporting symptoms beginning by five years of age. (2) In this chronic condition, therapy is directed at decreasing inflammation and minimizing symptoms. Available treatments include oral antihistamines, topical emollients, topical doxepin (Zonalon), and topical corticosteroids. It may also be alleviated with attention to bathing habits and avoidance of irritants. Disease severity and location determine which therapies are used. Topical steroids are commonly used to treat moderate to severe disease, but chronic use of these agents at higher concentrations can cause skin atrophy and pigmentation changes. Chronic use of higher potency steroids can also have systemic effects on the hypothalamic/ pituitary axis and inhibit growth. These adverse events may limit corticosteroid use in young children and adults in all areas, especially the face and intertriginous zones.
More has been learned over the past few years about the pathophysiology of atopic dermatitis. The recurrent itch and dermoepidermal inflammation manifests histologically as hypertrophy of the dermis and epidermis with presence of eosinophils, macrophages, and T cells. The inflammatory response in atopic dermatitis begins when an IgE-associated Langerhans' cell in the skin binds an antigen and presents the antigen to T cells, leading to the release of numerous cytokines, including various interleukins. These mediators lead to the recruitment of more inflammatory cells, and this results in edema. Scratching causes keratinocytes to release a variety of proinflammatory cytokines, which recruits more inflammatory cells.
Acute and chronic responses in atopic dermatitis are probably caused by separate interleukins. (3-5) Targeting these pathophysiologic factors has led to the development of new therapies, such as tacrolimus (Protopic).
Tacrolimus
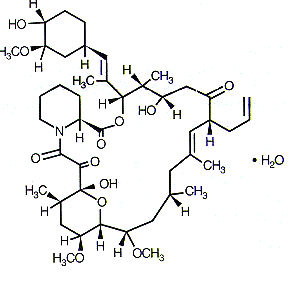
Tacrolimus is the first new topical therapy for the treatment of moderate to severe atopic dermatitis since the advent of topical corticosteroids. An immunosuppressive medication derived from macrolides, oral tacrolimus has been used since 1994 to prevent allograft rejection in liver and kidney transplants. (6) Pimecrolimus (Elidel) 1 percent cream was recently approved by the U.S. Food and Drug Administration for short-term and intermittent long-term treatment of mild to moderate atopic dermatitis in patients two years and older who do not respond well to or have side effects with conventional treatments. (7)
Cyclosporine (Sandimmune), another immunosuppressive agent, has also been used orally to treat psoriasis and atopic dermatitis, but its use is limited by the high incidence of side effects. Topical cyclosporine has shown inconsistent results. Tacrolimus has similar results to cyclosporine when administered systemically, but tacrolimus has better skin penetration (probably because of the smaller molecular mass of tacrolimus compared with cyclosporine), which makes it a better candidate for topical use. (8)
MECHANISM OF ACTION
Topical tacrolimus has been shown in vitro to bind to specific receptors on T cells. This leads to an increase in intracellular calcium that, in turn, causes a series of reactions inhibiting the transcription of several genes, mainly the cytokines (IL-2, IL-4, and IL-5). Tacrolimus also acts to decrease the production of IL-8 receptor genes and inhibits the production of receptors for IgE molecules. (9,10) Because it affects a variety of interleukins, it can be effective in the treatment of acute and chronic atopic dermatitis. Biopsy studies at three and seven days have shown diminished T-cell and eosinophilic infiltrates. (5)
PHARMACOKINETICS
Tacrolimus is metabolized in the liver but, with topical use, very little is absorbed. In a study of patients with moderate to severe atopic dermatitis, blood concentrations were below the detectable level in 80 percent of samples. Only 0.3 percent of samples had serum levels in the 5 to 20 ng per mL range, which is the target range for transplant patients, with the highest levels being 8.13 ng per mL. (11) Studies have shown that damaged skin has a sevenfold higher rate of absorption of tacrolimus. (10) Healed skin regains percutaneous barrier function, preventing the large molecule of tacrolimus from being absorbed.
CLINICAL TRIALS
Several studies have examined the efficacy of topical tacrolimus in adult patients. In a double-blind, placebo-controlled study, 215 patients with moderate to severe atopic dermatitis were randomized to receive 0.03, 0.1, or 0.3 percent tacrolimus, or vehicle, applied twice daily. Patients were evaluated at three weeks using atopic dermatitis severity scores. The decrease in scores for the three groups was 67, 83, and 75 percent for the 0.03, 0.1, and 0.3 percent ointments, respectively. The vehicle group showed a 22 percent decrease in severity scores. No statistical difference was found among the three tacrolimus groups, which showed equal efficacy in face, neck, and trunk regions. The only statistically significant side effect in treatment versus vehicle groups was a sensation of local burning, but this effect resulted in no increase in the dropout rate. (12) [Evidence level A, randomized controlled trial (RCT)]
In another study of 632 patients with moderate to severe atopic dermatitis, patients were randomized for 12 weeks to receive vehicle, 0.03 percent tacrolimus, or 0.1 percent tacrolimus ointment applied twice daily. Physician assessment at 12 weeks showed 90 percent improvement in 6.6 percent of the vehicle patients, 27.5 percent of the 0.03 percent tacrolimus group, and 36.8 percent of the patients using 0.1 percent tacrolimus ointment. Both treatment groups were significantly better than the vehicle group. Greater than 50 percent improvement occurred in 19.8 percent of the vehicle group, compared with 62 and 73 percent of the 0.03 and 0.1 percent tacrolimus groups, respectively. The differences between the two tacrolimus groups were most evident in patients with more severe disease and disease involving a larger surface area, and in black patients. Discontinuation of the study because of adverse events occurred twice as often in the vehicle group. (13) [Evidence level A, RCT]
Pediatric studies also showed efficacy. In a randomized, double-blind, vehicle-controlled study, 0.03 percent, 0.1 percent, and 0.3 percent tacrolimus were compared with vehicle therapy in children seven to 16 years of age over 23 days, with twice-daily treatment. Physician assessment showed that 67 to 70 percent of patients in the three treatment groups and 38 percent in the vehicle group had greater than 75 percent improvement in their atopic dermatitis. (14) [Evidence level A, RCT]
In another study, 351 children two to 15 years of age with moderate to severe atopic dermatitis were treated for 12 weeks with 0.03 percent or 0.1 percent tacrolimus ointment, or vehicle. By physician assessment, greater than 50 percent improvement occurred in 73 and 78 percent of the tacrolimus groups, respectively, versus 27 percent in the vehicle group. A higher incidence of skin burning and varicella occurred in the two treatment groups. Side effects were not dosage dependent. (15) [Evidence level A, RCT]
A study of Dermatology Quality of Life Indexes performed on 985 adult and younger patients with moderate to severe atopic dermatitis showed significant improvement in all areas over 12 weeks in patients who used tacrolimus. Patients were randomized to vehicle, 0.03 percent, or 0.1 percent tacrolimus and evaluated at the end of 12 weeks. The surveys included such aspects as itchiness, self-consciousness, relationships, and dressing. Significant differences versus vehicle were seen in every category in adults. In children, the biggest quality-of-life differences were found in itchiness, sleeping, emotions, and activities. When patients were asked if they were "very likely to continue" using the medicine, those using both strengths of tacrolimus were more likely to want to continue the medication than those who used the vehicle in all age groups. (16) [Evidence level A, RCT]
SAFETY
In clinical trials, the most common side effect was a burning sensation of the skin, occurring in 46 to 58 percent of patients treated with tacrolimus. This side effect was most frequent early in the course of treatment. Pruritus was reported in 46 percent of patients, although this rate was not statistically different than that for vehicle. Local effects are more common in patients with a higher amount of body-surface area affected. Patients using tacrolimus reported a higher rate of herpes simplex and eczema herpeticum. No laboratory abnormalities were reported, and no skin atrophy was noted. (10)
In a one-year open-label study of children two to 15 years of age, using 0.1 percent tacrolimus ointment twice daily, the most common side effect was skin burning in 26 percent, generally early in the course of therapy. Pruritus occurred in 23 percent of patients, and there was also an increase in skin infections (11 percent), namely herpes simplex, varicella, and eczema herpeticum. No significant laboratory abnormalities were found compared with baseline. (17)
With systemic tacrolimus, the principal adverse side effects are nephrotoxicity, neurotoxicity (especially insomnia, tremor, and headache), and gastrointestinal disturbances (e.g., diarrhea, nausea, and vomiting). With all immunosuppressive treatment regimens, there is an increased rate of malignancies, especially lymphomas. (18) No topical study showed an increase in malignancy rate, but all of the studies were of short duration. Because of the increase in non-melanoma skin cancer in patients using systemic tacrolimus therapy, it would make sense to ensure good sun protection in areas treated with topical tacrolimus. The drug is listed as a pregnancy category C agent, with no adequate well-controlled studies undertaken in pregnant women. (19)
DOSAGE AND COST
Tacrolimus ointment is produced under the brand name Protopic. It comes in 0.03 percent and 0.1 percent formulations. Adults can use either strength, but only the 0.03 percent strength is approved for use in children, and then only in those two years or older. A thin coating should be applied twice daily. The average wholesale cost of a 30-g tube is $54.37 for the 0.03 percent ointment and $58.12 for the 0.1 percent strength. The cost of a 60-g tube is $108.75 for the 0.03 percent ointment and $116.25 for the 0.1 percent. (20)
The author thanks Neil Skolnik, M.D., and Mathew Clark, M.D., for editorial assistance in the preparation of the manuscript and Monica Bonitatibus for clerical assistance.
The author indicates that he does not have any conflicts of interest. Sources of funding: none reported.
REFERENCES
(1.) Laughter D, Istvan JA, Tofte SJ, Hanifin JM. The prevalence of atopic dermatitis in Oregon schoolchildren. J Am Acad Dermatol 2000;43:649-55.
(2.) Lapidus CS, Honig PJ. Atopic dermatitis. Pediatr Rev 1994;15:327-32.
(3.) Tofte SJ, Hanifin JM. Current management and therapy of atopic dermatitis. J Am Acad Dermatol 2001;44(1 suppl):S13-6.
(4.) Boguniewicz M. Advances in the understanding and treatment of atopic dermatitis. Curr Opin Pediatr 1997;9:577-81.
(5.) Leung DY, Soter NA. Cellular and immunologic mechanisms in atopic dermatitis. J Am Acad Dermatol 2001;44(1 suppl):S1-12.
(6.) Tacrolimus (FK506) for organ transplants. Med Lett Drugs Ther 1994;36:82-3.
(7.) Pimecrolimus (Elidel). Facts & Comparisons: DrugLink. 2002;VI(1):1.
(8.) Nasr IS. Topical tacrolimus in dermatology. Clin Exp Dermatol 2000;25:250-4.
(9.) Bieber T. Topical tacrolimus (FK506): a new milestone in the management of atopic dermatitis. J Allergy Clin Immunol 1998;102(4 pt 1):555-7.
(10.) Ruzicka T, Assmann T, Homey B. Tacrolimus: the drug for the turn of the millennium? Arch Dermatol 1999;135:574-80.
(11.) Soter NA, Fleischer AB Jr, Webster GF, Monroe E, Lawrence I. Tacrolimus ointment for the treatment of atopic dermatitis in adult patients: part II, safety. J Am Acad Dermatol 2001;44(1 suppl):S39-46.
(12.) Ruzicka T, Bieber T, Schopf E, Rubins A, Dobozy A, Bos JD, et al. A short-term trial of tacrolimus ointment for atopic dermatitis. European Tacrolimus Multicenter Atopic Dermatitis Study Group. N Engl J Med 1997;337:816-21.
(13.) Hanifin JM, Ling MR, Langley R, Breneman D, Rafal E. Tacrolimus ointment for the treatment of atopic dermatitis in adult patients: part I, efficacy. J Am Acad Dermatol 2001;44(1 suppl):S28-38.
(14.) Boguniewicz M, Fiedler VC, Raimer S, Lawrence ID, Leung DY, Hanifin JM. A randomized, vehicle-controlled trial of tacrolimus ointment for treatment of atopic dermatitis in children. J Allergy Clin Immunol 1998;102(4 pt 1):637-44.
(15.) Paller A, Eichenfield LF, Leung DY, Stewart D, Appell M. A 12-week study of tacrolimus ointment for the treatment of atopic dermatitis in pediatric patients. J Am Acad Dermatol 2001;44(1 suppl):S47-57.
(16.) Drake L, Prendergast M, Maher R, Breneman D, Korman N, Satoi Y, et al. The impact of tacrolimus ointment on health-related quality of life of adult and pediatric patients with atopic dermatitis. J Am Acad Dermatol 2001;44(1 suppl):S65-72.
(17.) Kang S, Lucky AW, Pariser D, Lawrence I, Hanifin JM. Long-term safety and efficacy of tacrolimus ointment for the treatment of atopic dermatitis in children. J Am Acad Dermatol 2001;44(1 suppl):S58-64.
(18.) Plosker GL, Foster RH. Tacrolimus: a further update of its pharmacology and therapeutic use in the management of organ transplantation. Drugs 2000;59:323-89.
(19.) Protopic. Packet insert. Fujisawa Pharmaceuticals. Retrieved May 2002, from: http://www.protopic. com/img/protopic_pi.pdf.
(20.) 2001 Drug Topics Red Book. Montvale, N.J.: Medical Economics Co., 2001:486.
Richard W. Sloan, M.D., R.Ph., coordinator of this series, is chairman and residency program director of the Department of Family Medicine at York (Pa.) Hospital and clinical associate professor in family and community medicine at the Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pa.
JOHN J. RUSSELL, M.D., is associate director of the Family Practice Residency Program at Abington Memorial Hospital, Abington, Pa., and assistant clinical professor in the Department of Family Medicine at Temple University School of Medicine, Philadelphia. Dr. Russell is a graduate of Pennsylvania State University College of Medicine, Hershey, and completed a family practice residency at Abington Memorial Hospital.
Address correspondence to John J. Russell, M.D., 817 Old York Rd., Jenkintown, PA 19046. Reprints are not available from the author.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group