Background: This paper addresses a specific experimental design to suggest the possible role of the greater omentum in the modulation of pain in rats.
Methods: Fifteen male Sprague-Dawley rats weighing between 275 and 325 g were selected. The animals were randomized and then anesthetized with pentobarbital (35 mg/kg) and divided into three groups: (1) sham: laparotomy followed by laminectomy with exposure of the spinal epidural space (n = 5); (2) transposition of pedicled omentum (n = 5) to the cauda equina epidural space; and (3) transposition of pedicled omentum (n = 5) to the cauda equina intradural space. The animals were operated upon and once more randomized by an independent investigator, so that the groups were thought to be similar during post-operative testing. The latency of paw withdrawal to noxious heat stimulation was tested and the values (seconds) plotted for 1, 3, 6, 11, 14 and 30 days after surgery. Randomization codes were open after the animals were euthanized. The analysis of variance (ANOVA) without replication was applied for each of the dataset and comparisons established among the different study groups involved. The omenta were removed and standard immunohistocnemistry was performed for gamma-ami no-butyric acid (GABA), serotonin, calcitonin-gene related protein (CGRP), vascular intestinal peptide (VIP) and Met-enkephalin.
Results: The response to high heating rates of stimulation favored intradural versus sham and epidural omental transpositions. High and low noxious heat stimulation suggested an increased threshold to noxious stimulation after the 3 and 30 days of omental transposition. In the low heat stimulation series, responses were comparatively higher than in the sham animals.
Conclusions: The suggested increased threshold of response to noxious stimulation after transposition of the greater omentum onto the spinal com of rats suggested a novel role of the omentum and a potential future application in the clinical arena. [Neural Res 2005; 27: 598-608]
Keywords: Omentum; pain; fibroblast growth factor; Met-enkephalin; neurotrophin; omentum transposition
INTRODUCTION
The greater omentum has been utilized in neurosurgery for the management of cerebrovascular insufficiency, in particular in Moyamoya1-3. The ubiquitous presence of vascular endothelial growth factor (VEGF) popularized its extensive use in neurosurgery and other surgical fields. Opioids, neurotransmitters, fibroblast growth factors and other substances have been found in the omentum as well.
Since the time of Hippocrates, the physiology of the greater omentum has been debated. Notwithstanding, its applications to the nervous system continue to expand, encompassing not only the realm of cerebrovascular insufficiency but also dementia and spinal cord injury4-7.
Amelioration of pain after transposition of the greater omentum to the peripheral nervous system was initially described for vascular neuropathies . The regional improvement in blood flow explained most of the effects, but failed to explain the attenuation of chronic pain observed on many occasions. Neuroplasticity in the central nervous system and, in particular, in the spinal cord pain pathways explains many of the clinical effects15,16.
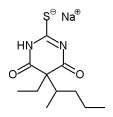
High-performance liquid chromatography (HPLC) of the venous product of the omentum demonstrated the presence of Met-enkephalin, among other substances, indicating possible alternative mechanisms of pain modulation17. Optional mechanisms are the increase in local secretion or accumulation of substances that contribute to the modulation of pain in the central nervous system, or the interaction between the increase in blood flow and the secretion or accumulation of specific substances in the periphery, ultimately leading to the subjective decrease in pain experienced by patients.
More recently, neurotrophins have been implicated in the modulation of neuropathic pain. In particular, brain-derived neurotrophic factor (BDNF) has been associated with the facilitation of synaptic transmission in lamina Il of the spinal cord of rats, an area that directly receives sensory input from the periphery18-20. More recently, the omental genes have been shown to express diverse neurotrophins, including BDNF21. Although modulation of neurotrophin expression is not yet fully understood, omental transposition may play a significant role in the modulation of neuropathic pain in the central nervous system, which would explain its prominent effect after transposition to the cauda equine of rats.
In this paper, we describe an experimental design to address the possible role of the omentum on the increase in pain thresholds in rats. The development of a unique method of transposition of the pedicled omentum to the spinal epidural or intradural spaces permitted the investigation of different effects of the transposition of the omentum for the modulation of noxious stimulation in rats. In addition, the utilization of a small animal model permitted easy experimental reproduction of the study and investigation of potential drawbacks in the study design. A thorough immunohistochemical identification of pertinent antinociceptive substances permitted the formulation of different ideas related to the possible antinociceptive mechanisms of the transposition of the omentum in patients.
MATERIALS AND METHODS
The procedures described in this section have all been in compliance with the Animal and Care Policies of the University of Illinois at Chicago. The suffering of animals was minimized in all situations. All 15 animals were handled in order to provide 15 independent samples.
Transposition of the pedicled omentum to the cauda equina
Sham operations (n=5)
Five male Sprague-Dawley rats weighing between 275 and 325 g were anesthetized with 0.5 mg/kg of intraperitoneal (i.p.) pentobarbital. The animals were then draped and prepared for a 5-cm laparotomy and a low laminectomy (L3-L5).
Epidural (n=5)
Five Sprague-Dawley rats weighing from 275 to 325 g were anesthetized with 0.5 mg of i.p. pentobarbital/kg, draped and prepared for surgery. On laparotomy, the greater omentum and its attachments to the transverse colon, the spleen and the stomach were identified. The neurovascular bundle was dissected free and the distal attachments to the spleen, transverse colon and liver were microsurgically released. The distal vascular attachments to the omentum from the spleen were dissected and cauterized. The vascular supply originating from the gastroepiploic vessels was maintained. The abdominal skin was then temporarily closed with 7.5 mm wound clips.
A low laminectomy (L5-S1) was performed, the abdominal incision reopened, and the animal positioned in a right lateral decubitus. A hemostat was then positioned on the left paravertebral space and its tip identified anteriorly, after piercing the paravertebral muscles. The omentum was then brought to the tip of the hemostat, secured and carefully brought to the cauda equina region subjacent to the laminectomy. The abdominal incision was closed by planes with 4.0 chromic gut sutures to the abdominal rectus muscle, and with 7.5 mm wound clips to the abdominal wall. The omentum was transposed to the top of the epidural space of the cauda equina, and secured to the paravertebral space with 6.0 prolene sutures. General inspection and hemostasis of the surgical site was carefully pursued. The incision was closed and the animals observed for 24 hours in the laboratory until fully recovered from surgery.
Intradural (n=5)
The dura mater was opened under a surgical microscopic view and the omentum transposed to the cauda equina regions of the animals. Anesthesia and surgery were performed similarly in Groups B and C, with the exception that, in Group C, the dura mater was opened under direct microscopic view.
Testing
Testing consisted of initial painting in black ink of the distal aspects of the paws (for better absorption of the thermal stimulus), in rats that had been lightly anesthetized. Light was directed to the lateral and medial aspects of the paws (distribution of the saphenous or sciatic nerves) and the time required for removal of the paw from the stimulus, calculated and plotted. Testing was repeated three times for each side of the paw, with the appropriate intervals between the measurements. Data was then averaged and plotted against time after transposition. Prior electrophysiological studies showed an average latency of paw withdrawal at 2.5 seconds with high heating rates (6.5°C/second), which was particularly related to Aδ fiber responses. Low skin heating rates (0.9°C/second) elicit preferential C fiber responses between 8 and 10 seconds after the stimulus. Care was taken not to over stimulate the skin (over 6 seconds for high heating rates and over 15 seconds for low heating rates).
Euthanasia
The animals were euthanized at 35 days after the initial surgery by i.p. injection of 0.8-1.2 cc of thiopental sodium. The omenta were post-fixed with 4% paraformaldehyde and refrigerated for 4 hours. The tissue was then transferred to 0.1 M phosphate buffer. Repeated dehydration was necessary, in order to remove the excessive amount of fat and for a better binding of the monoclonal antibodies.
Data analysis
Thermal responsiveness (seconds) was plotted against days after transposition of the omentum and a two-way analysis of variance (ANOVA) performed for an alpha of 5%. The null hypothesis tested was the absence of statistical difference between the sham, epidural and intradural transpositions. The data were initially analysed for the whole group and then between the sham and epidural, sham and intradural, and epidural and intradural transpositions of the omentum. The procedure was repeated for the high (Aδ fibers) and low (C fibers) thermal stimulation. Tukey, LSD and Dunnet post-hoc analyses were performed to determine whether there was any statistically significant difference between the means for each individual pair of data using version 11.01 of SPSS software (SPSS Inc., Chicago, IL).
Preparation of the tissue
Five animals were anesthetized with 5 mg/100 g of pentobarbital intraperitoneally, the abdomen was incised as previously described, and the omentum removed en bloc from the attachments to the stomach, transverse colon and spleen of all animals. The omentum was then washed copiously in a Petri dish containing PBS and heparin in order to remove most of the blood from the tissue. The omentum was then fixed overnight in paraformaldehyde at 4%, at 4°C and washed in 0.01% Triton X-100 for 20 minutes, after which it was embedded in paraffin in 10 µm microtome sections.
Immunohistochemistry for light microscopy
On the first day, the sections were deparafinized and re-hydrated in xylene and progressive dilutions of ethanol at 100, 95, 80 and 70%. Then, the endogenous peroxidase was blocked with 30% hydrogen peroxide at room temperature. The sections were then treated with 0.5 mg/ml of hyaluronidase (to permit better access of the antibodies to antigens in the tissue), washed in TBS (Tris balanced salt solution) in 0.1% BSA (bovine serum albumin), and washed in TBS-BSA. Non-specific binding was blocked with normal goat serum, and the primary antibodies were prepared at concentrations of 1:500 for GABA (gamma-amino butyric acid), 1:400 for 5-HT (serotonin), 1:2000 for CGRP (calcitonin-gene related peptide), 1:500 for Met-enkephalin and 1:2000 for VIP (vascular intestinal peptide). These concentrations were determined in preliminary experiments. All the antibodies were purchased from Sigma (Sigma Inc., St Louis, MO). The slides were incubated overnight at 4°C.
On the second day, the primary antibody was removed by washing three times from the section with TBS. The sections were then incubated with secondary antibody for 24 hours at -80°C. We utilized the ABC (avidin-biotin complex) kit by Santa Cruz. The ABC was prepared and mixed with TBS-BSA. The slides were washed in TBS-BSA for 10 minutes (2 × 5 minutes) and then washed in TBS for 20 minutes (2 × 10 minutes). Then the AEC (avidin-enzyme complex) enzyme substrate was prepared by adding 25 mg of AEC per 10 cc of dimethylformamide and dissolved to 100 cc 0.2 M sodium acetate. The slides were then placed in the solution for up to 20 minutes until the color was developed. The slides were washed again in TBS, placed under running tap water for 5 minutes, and counterstained with filtered hematoxylin for
RESULTS
High heating stimulation responses (Aδ fibers) (Figure 1)
Post-hoc analysis of the data generated on thermal paw stimulation in rats suggested a significant difference between sham and intrathecal responses at day 3 of testing (P=0.022). Follow-up data in the subacute period failed to demonstrate a significant difference among the three groups. No further difference was noted between the groups analysed.
Low heating stimulation responses (C fibers) (Figure 2)
Post-hoc analysis of pairwise differences between the means among the groups yielded a statistically significant difference of noxious thermal stimulation between sham and epidural on the third (P=0.014) and sixth (P=0.044) days after transposition, suggesting a positive effect of epidural transposition on the increase in the threshold for perception of noxious heat. In addition, there was a statistically significant difference between the epidural and intrathecal on the 30th day after transposition, suggesting a differential response to noxious heat when the C fibers were individually tested (P=0.002).
Imunohistochemistry
The immunohistochemical analyses of the omentum were qualitative and not quantitative, as the morphology of the tissue is not uniform and there was a variation in the type of cells stained at each occasion.
Examination of sections for immunoreactivity for GABA demonstrated that GABA tends to be localized in adipocites near blood vessels (Figure 3). There was no staining in the control sections (no primary antibody+secondary antibody and blocking serum).
The immunohistochemical staining for 5-HT showed that the staining was localized around the blood vessels, in specific clusters of cells, which appear to correspond to the human "milky spots", i.e. zones of maturation of T lymphocytes (Figure 4).
The distribution of CGRP was preferentially located between adipocites, and also in minor amounts in close relationship with the 'milky spots' (Figure 5).
The immunohistochemistry for Met-enkephalin showed a diffuse location of the neuropeptide in the omentum (Figure 6).
VIP tended to be localized in the 'milky spots', suggesting a specific role in the maturation of lymphocytes or in the control of an inflammatory process (Figure 7).
DISCUSSION
For over 10 years, the experimental transplantation of chromaffin cells onto the spinal epidural or subarchnoid spaces was thought to be a good alternative for the management of chronic pain in humans22-29. The development of safe transposition methods by Sagen et al.30,31, in addition to the description of direct and indirect modulation of pain fibers and potentially the production of substances such as CGRP and other gene modulators deeply involved in the modulation of neuropathic pain, suggested that the role of chromaffin cells was beyond random. The presence of Met-enkephalin and cytokines, including fibroblast growth factors, TGF-beta and several interleukins have been well described in chromaffin cells and thought to contribute to the experimental observation of amelioration of pain32-34.
Difficulty obtaining tissue, ethical issues related to transplant to humans, and potential rejection, with required immunosuppression have been ongoing problems. The inability of the chromaffin cells to be used as autografts and, in particular, the short life span after transposition to the spinal cord made this a rather unpractical transplant to be performed in many conditions. The alternative use of the omentum for pain is attractive as previous evidence showed that omentum transposition decreases pain in many clinical conditions such as peripheral neuropathies, brachial plexus injuries, neuropathic pain resulting from actinic lesions to the skin and other conditions associated with pain9,10,35. Moreover, it is an autologous transplant and will not incur the same side effects observed with chromaffin cells and other tissues. Each case needs to be analysed individually to determine whether the omentum is suitable for transposition and whether the patient will be able to tolerate the surgery. However, the development of omentum extracts may provide a better alternative to whole organ transposition and ease the surgical procedure.
We utilized the method developed by Yeomans et al. to test for response to noxious heat and differentiate between Aδ and C fibers36,37. C and Aδ fibers respond differently to noxious radiant heat.
The greater omentum has a rich vascular supply and absorptive properties that have been fascinating anatomists and physicians alike38-41. Amelioration of pain has been previously observed after transposition of the greater omentum in patients with reconstructed radionecrotic skin lesions overlying the brachial plexus9,10,35, thus suggesting that, besides the improvement of blood flow, the omentum might secrete antinociceptive substances.
VECF42-44 fibrob|ast growth factors (FGF)45-48 have been correlated with cerebral and spinal neovascularization after transposition of the omentum to the spinal cord or brain. The observation of Met-enkephain in the omentum has been described and potentially showed the role of the omentum in the decrease of pain in patients49. The combination of neovascularization and secretion of Met-enkephalin may potentially explain some of the antinociceptive effects of the omentum after transposition for diverse situations.
Many of the effects of omental transposition seem to be mediated by the interaction between growth factors and immediate early genes, which, ultimately, will lead to the production of specific substances by the omentum50.
In 1998, Spaic et al. described dorsal root entry zone (DREZ) surgery for the management of neuropathic pain51. Omental graft has been used systematically in patients with complaints of chronic back pain, or secondary arachnoiditis, or lumbar CSF leak with the consistent observation of a decrease in pain in some conditions. In 1999, Spaic et al. described the need for DREZ surgery for the management of pain after failed omental transposition to the spinal cord. The study was limited, however, and there were no controls to which the DREZ procedure could be compared. There was no histological analysis of the omentum, the number of patients was small, and the population of patients with gunshot wounds to the back may not be the most opportune to have improvement in pain after transposition of the greater omentum. DREZ may, therefore, be the best surgical alternative to be considered52. In 2002, in a follow-up study, Spaic et al. established their experience with DREZ for the management of gunshot wound lesions to the lower back, observing good results overall. Their observation suggested that the omentum might not work in all modalities of pain appreciated. In our preliminary studies, there was not only a change in the morphology of omental cells (unpublished observation) with an increase in size of the mesenchymal cells and increased vascularization, but also in the location of secretions in the omental cells after ligation of the sciatic nerve as a model for neuropathic pain. In addition, the effects were more pronounced when C fibers were tested, as opposed to Aδ, suggesting that different pain syndromes may be affected differently as well. DREZ surgery has been well established for the management of many pain conditions and proved also to be effective when the omentum transposition failed to improve nociception. In this paper, the omentum has been shown to significantly increase the threshold for thermal responsiveness for both high (Aδ fibers) and low rates (C fibers) of heating of paws. The effects of the transposition of the greater omentum to the cauda equina were more pronounced for the pedicled transplants and for the C fibers, suggesting a preferential role on the modulation of neuropathic and chronic pain in rats, in particular after transposition to the intradural space. The reason behind such an effect lies with the rich vascular supply, and the proximity to the spinal cord, with the possibility of a direct influence of the omentum over direct pain pathways in the spinal cord and, in particular, the spinothalamic tract, which modulates and integrates impulses generated in the periphery by stimulation of free or specialized encapsulated receptors.
Fibroblast growth factors have been found in the periaqueductal gray matter, raphe nucleus and the spinal cord of animals. The anatomical relationship of these areas with the modulation of chronic pain is well known. In 1996, Cuevas et al.53 described the immediate analgesic effects obtained after pharmacological injection of acidic FGF (aFGF) into the subarachnoidal spaces of rats. The authors showed that there was a significant attenuation of pain in the tail-flick test in rats after injection. The effects lasted for 15-30 minutes and progressively faded over time. The initial description of the antinociceptive effects of nitric oxide and the metabolic interaction between the latter and aFGF indicates that a similar mechanism of modulation occurs and that fibroblast growth factor participates in the maintenance of neural terminals in chronic pain54,55. Therefore, one of the explanations for the effects observed after the transposition of the greater omentum to the cauda equina is the ubiquitous secretion or accumulation of aFGF described previously48, lnterleukins, nitric oxide and VIP56-59 have been implicated in the modulation of inflammatory pain in the spinal cord. In this paper, the omentum was shown to contain VIP and CGRP, well-known proinflammatory substances. The local and central modulation of pain may be related to the abundant secretion of neuropeptides and, more importantly, the interaction between each of the components in the intracellular molecular pathways.
Growth factors, particularly BDNF, nerve growth factors (NGF) and FGF have been implicated in the development of plasticity and chronic pain, or in the modulation of chronic pain in the central nervous system60-62.
A significant amount of work has been dedicated to the physiologic roles of BDNF in the modulation of neuropathic pain in animals. It has been implicated in the facilitation of neuronal responses as a result of chronic pain by multiple mechanisms. Current evidence suggests that BDNF increases the permeability of sodium channels, providing a faster depolarization of spinal cord neurons in animal models of chronic pain and therefore contributing to the development of acute hyperalgesia in rats63. It also increases the release of substance P from neurons in rats subject to chronic constriction injury of the sciatic nerve. In the recent past, neurotrophins have been shown to play an important role in the development of systemic hyperalgesia in animals64,65. The different effects with BDNF and other neurotrophins suggest that BDNF and neurotrophin-3 participate in the decrease in hyperalgic response associated with thermal hyperalgesia in animals. The effects seem to be mediated by GABA20,66,67 in the dorsal horn of rats. More recently, neurotrophin-3 has been implicated in the decrease of pain thresholds after induction of thermal hyperalgesia in rats, suggesting a modulation of genes directly related to the modulation of pain in the spinal cord of rats68. Long-term modulation of pain is probably associated with the degree of plasticity obtained after the initial insult. Current evidence suggests that plasticity is directly related to the initial activity of neurotrophins in the spinal cord neurons by modulation of neurotrophin receptors69-71. Dujovny et al. recently showed that the omentum holds all neurotrophin genes and their expression may eventually explain the results in our experimental transposition model21. Other recent papers addressed similar issues associated with the transcription of specific genes in the omentum secondary to diverse external influences, including the interaction with the external environment. In the majority of the studies, the omentum is regarded as a potential central organ in the control of obesity. This is mostly related to diverse genes present in omental cells and capable of producing diverse substances that, ultimately, will promote cell growth and transformation72,73. From our perspective, the omentum participates in the modulation of pain by secretion of anti-algic substances and by promoting central control of pain by inducing neuronal plasticity once cells are exposed to noxious stimuli.
However, the establishment of novel circuits54,74,75 may be pivotal for the modulation of chronic pain in the spinal cord, as well as in the thalamus and other CNS structures. Future trends in omentum research include analysis of the molecular biology of pain before and after transplant of the omentum to the central nervous system. This would particularly involve immediate early genes, and their interaction with intracellular messengers and other cell components and cascades ultimately participating in the modulation of pain, as well as in the promotion of neovascularization of the nervous system.
A significant amount of work has been carried out on gene expression in the omentum. Recently, FGF, NGF, BDNF and other neurotrophins have been identified in the omental genetic material, again emphasizing the important role of the greater omentum in the modulation of neurological conditions76.
Stem cells have been recently identified in the omentum77-79. Although not yet directly related to pain modulation, future perspectives may further explain the effects of transposition of the greater omentum for modulation of chronic pain in animals.
Our main initial problem was to develop a model that would sustain perfusion for long enough. From our perspective, the free graft failed to work for a prolonged period of time due to the progressive decrease in perfusion and subsequent death of omental cells. Recently, Pap-Szekeres et al. developed a microsurgical anastomosis model of the free graft omentum to the spinal cord of dogs80. In rats, however, there are no papers to our knowledge that address free graft microsurgical anastomosis to the spinal cord, since the vessels are significantly smaller and the technical difficulties overcome the potential advantages of the method when maintenance of the omental pedicle is technically easier.
We observed that the effects of transposition of the omentum to the cauda equina of rats were short-lived. Our personal experience suggests that stretching of the vasculature and subsequent ischemic necrosis of the omental tissue permitted "normalization" of the physiologic response to thermal stimuli, as well as the non-adaptation of the omentum. Adaptation to the new environment is a possible reason for the results observed. In addition, the possible persistent local opioid production permitted modulation of peripheral nociceptive stimuli. Antagonist drugs should be attempted, in many situations, to modulate the response of the omentum, if this were the true antinociceptive effect. In order to understand the fate of the omentum, a detailed molecular analysis of the ultrastructure, as well as of the molecular biology of the omental cells, would help to identify the possible reasons for the overwhelming effects of the transplant or transposition of the omentum to the central nervous system. The data suggest that a larger sample will be necessary to determine whether the effects are real or exaggerated by the small sample in this preliminary experiment, even though the average indicated a statistically significant increase in reaction to noxious heat in those animals. Moreover, selection of a larger number of animals and a longer observation period may help in identifying the chronic tendency of attenuation of thermal responsiveness in animals. In addition, transposition of the greater omentum onto cauda equina regions of other animals may help identify future ideas for the management of chronic pain in a select group of patients. Identification of specific substances secreted by the omentum may justify extraction of lipid fractions with direct injection into rats' epidural or intradural spaces. Identification of specific neuropeptides secreted by the omentum would permit a better understanding of the physiopathology of the omentum in modulating neuropathic pain in humans.
CONCLUSIONS
The preliminary data presented in this paper suggests that the omentum has acute effects on the increase in pain threshold in rats. Additionally, we were able to show that the omentum produces/accumulates several substances that may have a role in the modulation of pain in the central nervous system, including 5-HT, CGRP, VIP, GABA and Met-enkephalin. The effects were more pronounced and prolonged when the omentum was attached to its pedicle, which indicates that perfusion is required to promote optimal secretion of substances by the omentum.
More research needs to be conducted to understand the mechanisms of pain modulation after the transposition or transplant of the omentum to the spinal subarachnoid or epidural spaces in rats. Further investigation on the modulation of pain by growth factors is underway. The failure of medical management of pain and the large incidence of pain in the society at large triggers the development of alternative modalities of treatment and the transposition of the greater omentum to the cauda equina or spinal cord may be one of them.
As the study is in its preliminary phase, several points need to be addressed in continuation. The first step is to determine how long the omentum survives in situ or if the secretion decreases overtime, which may significantly alter its clinical application in pain management. Also, the cells will need to be individually separated and their secretion products isolated. This, per se, can determine if the omentum should be transplanted as a whole or if just a fraction of it, i.e. specific cells, should be transplanted into the spinal epidural or intradural spaces, where different components would be able to circulate freely. Also, the injection of specific antagonists or agonists of GABA, Met-enkephalin, VIP, 5-HT and CGRP at different phases of the testing would be able to show with which kinds of pain the transplant is more effective, as well as which specific substance would be more responsible for the modulation of specific pain syndromes at the level of the central nervous system.
REFERENCES
1 Goldsmith HS, Duckett S, Chen WF, Prevention of cerebral infarction in the monkey by omental transposition to the brain. Stroke 1978; 9: 224-229
2 Goldsmith HS, Saunders RL, Reeves AG, et al Stroke 1979; 10: 471-472
3 Herold S, Frackowiak RS, Neil-Dwyer C. Studies on cerebral blood flow and oxygen metabolism in patients with established cerebral infarcts undergoing omental transposition. Stroke 1987; 18: 46-51
4 Goldsmith HS. Acute spinal cord injuries: A search for functional improvement. Surg Neural 1999; 51: 231-233
5 Gonzalez-Darder JM, Barcia-Salorio JL, Barbera J, et al. Intraventricular transplantation of omentum for treatment of hydrocephalus. An experimental study in dogs. Acta Neurochir Suppl (Wien) 1988; 43: 159-161
6 Gruss JS, Antonyshyn O, Phillips, JH. Early definitive bone and soft-tissue reconstruction of major gunshot wounds of the face. Plast ReconstrSurg 1991; 87: 436-450
7 Havlik RJ, Fried I, Chyatte D. et al. Encephalo-omental synangiosis in the management of moyamoya disease. Surgery 1992; 111: 156-162
8 Ala-Kulju K, Virkkula L. Use of omental pedicle for treatment of Buerger's disease affecting the upper extremities. A modified technique. Vasa 1990; 19: 330-333
9 Brunelli G. Neurolysis and free microvascular omentum transfer in the treatment of postactinic palsies of the brachial plexus, lnt Surg 1980; 65: 515-519
10 Brunelli G, Brunelli F. Surgical treatment of actinic brachial plexus lesions: Free microvascular transfer of the greater omentum. J Reconstr Microsurg 1985; 1: 197-200
11 Herrera HR, Geary J, Whitehead P, et al. Revascularization of the lower extremity with omentum. CHn Plast Surg 1991; 18: 491-495
12 Laszlo G. [Management of critical ischemia of the leg by omentum transplantation in Buerger's disease] Buerger-korosok kritikus vegtagischaemiajanak kezelese csepleszatultetessel. Orv Hetil 1989; 130: 1993-1994
13 Laszlo G. [Follow up studies on patients with Buerger's disease treated with omentum transplantation (letter)] Csepleszatulteteses mutettel kezelt Buerger-koros betegek utanvizsgalata. Orv Hetil 1992; 133: 254
14 Piano G Massad MG, Amory DW Jr, et al. Omental transfer for salvage of the moribund lower extremity. Am Surg 1998; 64: 424-427
15 Neuroplasticity and repair in the central nervous system. Implications for health care. WHO Offset Publ 1983; 73: 1-56
16 de la Torre JC, Goldsmith HS. Increased blood flow enhances axon regeneration after spinal transection. Neurosci Lett 1988; 94: 269-273
17 Goldsmith HS, Mclntosh T, Vezina RM, et al. Vasoactive neurochemicals identified in omentum: A preliminary report. Br J Neumsurg 1987; 1: 359-364
18 Fukuoka T, Kondo E, Dai Y, et al. Brain-derived neurotrophic factor increases in the uninjured dorsal root ganglion neurons in selective spinal nerve ligation model. J Neurosci 2001; 21: 4891-4900
19 Garraway SM, Petruska JC, Mendell LM. BDNF sensitizes the response of lamina Il neurons to high threshold primary afferent inputs. Eur J Neurosci 2003; 18: 2467-2476
20 Pezet S, Malcangio M, McMahon SB. BDNF: A neuromodulator in nociceptive pathways? Brain Res Brain Res Rev2002; 40: 240-249
21 Dujovny M, Ding YH, Ding Y, et al. Current concepts on the expression of neurotrophins in the greater omentum. Neurol Res 2004; 26: 226-229
22 Bes JC, Tkaczuk J, Czech KA, et al. One-year chromaffin cell allograft survival in cancer patients with chronic pain: Morphological and functional evidence. Cell Transplant 1998; 7: 227-238
23 Buchser E, Goddard M, Heyd B, et al, Immunoisolated xenogenic chromaffin cell therapy for chronic pain. Initial clinical experience. Anesthesiology 1996; 85: 1005-1012
24 Hama AT, Sagen J. Reduced pain-related behavior by adrenal medullary transplants in rats with experimental painful peripheral neuropathy. Pain 1993; 52: 223-231
25 Hama AT, Sagen J. Alleviation of neuropathic pain symptoms by xenogeneic chromaffin cell grafts in the spinal subarachnoid space. Brain Res 1994; 651: 183-193.
26 Lazorthes Y, Bes JC, Sagen J, et al. Transplantation of human chromaffin cells for control of intractable cancer pain. Acta Neurochir Suppl (Wien) 1995; 64: 97-100
27 Pappas GD, Lazorthes Y, Bes JC, et al. Relief of intractable cancer pain by human chromaffin cell transplants: Experience at two medical centers. Neurol Res 1997; 19: 71-77
28 Sagen J. Cellular transplantation for intractable pain. Adv Pharmacol 1998; 42: 579-582
29 Yu W, Hao JX, Xu XJ, et al. Long-term alleviation of allodynia-like behaviors by intrathecal implantation of bovine chromaffin cells in rats with spinal cord injury. Pain 1998; 74: 115-122
30 Sagen J, Pappas GD, Perlow MJ. Adrenal medullary tissue transplants in the rat spinal cord reduce pain sensitivity. Brain Res 1986; 384: 189-194
31 Sagen J, Pappas GD, Pollard HB. Analgesia induced by isolated bovine chromaffin cells implanted in rat spinal cord. Proc Natl Acad Sci USA 1986; 83: 7522-7526
32 Sagen J, Kemmler JE. Increased levels of Met-enkephalin-like immunoreactivity in the spinal cord CSF of rats with adrenal medullary transplants. Brain Res 1989; 502: 1-10
33 Unsicker K, Krieglstein K. Growth factors in chromaffin cells. Prog Neurobiol 1996; 48: 307-324
34 Lu Y, Jing R, Yeomans DC et al. Porcine chromaffin cells, culture, and transplant for antinociceptive effects in rodents and primates. Neurol Res 2004; 26: 707-712
35 Bostwick J, Stevenson TR, Nahai F, et al. Radiation to the breast. Complications amenable to surgical treatment. Ann Surg 1984; 200: 543-553
36 Yeomans DC, Proudfit HK. Characterization of the foot withdrawal response to noxious radiant heat in the rat. Pain 1994; 59: 85-94
37 Yeomans DC, Proudfit HK. Nociceptive responses to high and low rates of noxious cutaneous heating are mediated by different nociceptors in the rat: Electrophysiological evidence. Pain 1996; 68: 141-150
38 Goldsmith HS, Chen WF, Duckett SW. Brain vascularization by intact omentum. Arch Surg 1973; 106: 695-698
39 Jurkiewicz MJ, Arnold PG. The omentum: An account of its use in the reconstruction of the chest wall. Ann Surg 1977; 185: 548-554
40 Micheau P. (The greater omentum. Its role in reconstructive plastic surgery] Le grand epiploon. Sa place en chirurgie plastique reparatrice. Ann Chir Plast. Esthet 1995; 40: 192-207
41 Ramstrom J, Jaramillo A, Cadavid E, et al. A 'new' intraabdominal artery. The pedicled right gastroepiploic artery for myocardial revascularization. Eur J Surg 1992; 158: 25-28
42 Howdieshell TR, RiegnerC, Gupta V, et al. Normoxic wound fluid contains high levels of vascular endothelial growth factor. Ann Surg 1998; 228: 707-715
43 Wakabayashi Y, Shono T, lsono M, et al. Dual pathways of tubular morphogenesis of vascular endothelial cells by human glioma cells: Vascular endothelial growth factor/basic fibroblast growth factor and interleukin-8. Jpn J Cancer Res 1995; 86: 1189-1197
44 Zhang QX, Magovern CJ, Mack CA, et al. Vascular endothelial growth factor is the major angiogenic factor in omentum: Mechanism of the omentum-mediated angiogenesis. J Surg Res 1997; 67: 147-154
45 Bikfalvi A, Alterio J, Inyang AL, et al. Basic fibroblast growth factor expression in human omental microvascular endothelial cells and the effect of phorbol ester. J Cell Physiol 1990; 144: 151-158
46 Konturek SJ, Brzozowski T, Majka I, et al. Omentum and basic fibroblast growth factor in healing of chronic gastric ulcerations in rats. Dig Dis Sci 1994; 39: 1064-1071
47 Mydlo JH, Krai JG, Macchia RJ. Preliminary results comparing the recovery of basic fibroblast growth factor (FGF-2) in adipose tissue and benign and malignant renal tissue. J Urol 1998; 159: 2159-2163
48 Ohtaki T, Wakamatsu K, Mori M, et al. Purification of acidic fibroblast growth factor from bovine omentum. Biochem Biophys Res Commun 1989; 161: 169-175
49 Goldsmith HS, Marquis JK, Siek G. Choline acetyltransferase activity in omental tissue. Br J Neurosurg 1987; 1: 463-466
50 Kopernik G. The effect of a high partial pressure of carbon dioxide environment on metabolism and immune functions of human peritoneal cells-relevance to carbon dioxide pneumoperitoneum. Am J Obstet Gynecol 1998; 179: 1503-1510
51 Spaic M, Tadic R. [Surgical treatment of chronic neurogenic painclinical use of the DREZ operation] Hirursko lijecenje hronicnog neurogenog bola-klinicka primjena DREZ operacije. Vojnosanit Pregl 1998; 55: 533-540
52 Spaic M, Petkovic S, Tadic R, et al. DREZ surgery on conus medullaris (after failed implantation of vascular omental graft) for treating chronic pain due to spine (gunshot) injuries. Acta Neurochir (Wien) 1999; 141: 1309-1312
53 Cuevas P, Prieto R, Saenz de Tejada I, et al. Analgesic effects of fibroblast growth factor in the rat. Neurosci Lett 1996; 207: 175-178
54 Nilsson J, von Euler AM, Dalsgaard CJ, et al. Stimulation of connective tissue cell growth by substance P and substance K. Nature 1985; 315: 61-63
55 Rohovsky S, Kearney M, Pieczek A, et al. Elevated levels of basic fibroblast growth factor in patients with limb ischemia. Am Heart J 1996; 132: 1015-1019
56 Basbaum Al, Glazer EJ. Immunoreactive vasoactive intestinal polypeptide is concentrated in the sacral spinal cord: A possible marker for pelvic visceral afferent fibers. Somatosens Res 1983; 1: 69-82
57 Kawatani M, Erdman SE, de Groat WC. Vasoactive intestinal polypeptide and substance P in primary afferent pathways to the sacral spinal cord of the cat. J Comp Neurol 1985; 241: 327-347
58 Kawatani M, Nagel J, de Groat WC. Identification of neuropeptides in pelvic and pudendal nerve afferent pathways to the sacral spinal cord of the cat. I Comp Neurol 1986; 249: 117-132
59 Often U, Lorez HP. Nerve growth factor increases substance P, cholecystokinin and vasoactive intestinal polypeptide immunoreactivities in primary sensory neurones of newborn rats. Neurosci Lett 1982; 34: 153-158
60 Jacobs EW, Hoffman S, Kirschner P, et al. Reconstruction of a large chest wall defect using greater omentum. Arch Surg 1978; 113: 886-887
61 Goldsmith HS. Omental transposition for peripheral vascular insufficiency. Rev Surg 1967; 24: 379-380
62 Fried SK, Bunkin DA, Greenberg AS. Omental and subcutaneous adipose tissues of obese subjects release interleukin-6: Depot difference and regulation by glucocorticoid. J Clin Endocrinol Metab 1998; 83: 847-850
63 Could HJ III, Gould TN, England JD, et al. A possible role for nerve growth factor in the augmentation of sodium channels in models of chronic pain. Brain Res 2000; 854: 19-29
64 Ueda M, Hirose M, Takei N, et al. Nerve growth factor induces systemic hyperalgesia after thoracic burn injury in the rat Neurosci Lett 2002; 328: 97-100
65 Meyer-Tuve A, Malcangio M, Ebersberger A, et al. Effect of brain-derived neurotrophic factor on the release of substance P from rat spinal cord. Neuroreport 2001; 12: 21-24
66 Lever I, Cunningham J, Grist J, et al. Release of BDNF and CABA in the dorsal horn of neuropathic rats. Eur J Neurosci 2003; 18: 1169-1174
67 Pezet S, Cunningham J, Patel J, et al. BDNF modulates sensory neuron synaptic activity by a facilitation of GABA transmission in the dorsal horn. Mol Cell Neurosci 2002; 21: 51-62
68 Wilson-Gerwing TD, Dmyterko MV, Zochodne DW, et al. Neurotrophin-3 suppresses thermal hyperalgesia associated with neuropathic pain and attenuates transient receptor potential vanilloid receptor-1 expression in adult sensory neurons. J Neurosci 2005, 25: 758-767
69 McMahon SB, Jones NC. Plasticity of pain signaling: Role of neurotrophic factors exemplified by acid-induced pain. J Neurobiol 2004; 61: 72-87
70 Csillik B, Janka Z, Boncz I, ef al. Molecular plasticity of primary nociceptive neurons: Relations of the NGF-c-jun system to neurotomy and chronic pain. Ann Anat 2003; 185: 303-314
71 Chao MV. Neurotrophins and their receptors: A convergence point for many signalling pathways. Nat Rev Neurosci 2003; 4: 299-309
72 Gomez-Ambrosi J, Catalan V, Diez-Caballero A, et al. Gene expression profile of omental adipose tissue in human obesity. FASEB J 2004; 18: 215-217
73 Vohl MC, Sladek R, Robitaille J, et al. A survey of genes differentially expressed in subcutaneous and visceral adipose tissue in men. Obesity Res 2004; 12: 1217-1222
74 DeLeo JA, Colburn RW, Rickman AJ. Cytokine and growth factor immunohistochemical spinal profiles in two animal models of mononeuropathy. Brain Res 1997; 759: 50-57
75 Lichtenberg J, Hjarnaa PJ, Kristjiansen PE, et al. The rat Subcutaneous Air Sac model: A quantitative assay of antiangiogenesis in induced vessels. Pharmacol Toxicol 1999; 84: 34-40
76 Agner C, Yeomans D, Dujovny M. The neurochemical basis for the applications of the greater omentum in neurosurgery. Neurol Res 2001; 23: 7-15
77 Van Harmelen V, Rohrig K, Hauner H. Comparison of proliferation and differentiation capacity of human adipocyte precursor cells from the omental and subcutaneous adipose tissue depot of obese subjects. Metabolism 2004; 53: 632-637
78 Bakker AH, Van Dielen FM, Greve JW, et al. Preadipocyte number in omental and subcutaneous adipose tissue of obese individuals. Obesity Res 2004; 12: 488-498
79 Kubai L, Auerbach R. A new source of embryonic lymphocytes in the mouse. Nature 1983; 301: 154-156
80 Pap-Szekeres J, Cserni G, Furka I, et al. Transplantation and microsurgical anastomosis of free omental grafts: Experimental animal model of a new operative technique in dogs. Microsurgery 2003; 23: 414-418
Celso Agner*, Manuel Dujovny[dagger] and David C. Yeomans[double dagger]
* Department of Neurosurgery, Albany Medical Center, Albany, NY, USA
[dagger] Department of Neurosurgery, Wayne State University, Detroit, MI, USA
[double dagger] Department of Anesthesia, Stanford University, Stanford, CA, USA
Correspondence and reprint requests to: Celso Agner, MD, MSc, 66 Ten Eyck Avenue, #2-Albany, NY 12209, USA. [cagner@nycap.rr. com] Accepted for publication April 2005.
Copyright Maney Publishing Sep 2005
Provided by ProQuest Information and Learning Company. All rights Reserved