Objectives: Calpains are intracellular proteases, which are activated in various cerebral injuries. We studied the expression of μ-calpain in a model of focal cerebral ischemia/reperfusion and the efficacy of the calpain inhibitor A-558693.
Methods: A transient occlusion of the middle cerebral artery was produced in male Wistar rats by using the suture model with 3 hours of ischemia and 24 hours of reperfusion. Six animals were given the calpain inhibitor and six animals were treated with placebo. The infarct size was determined by the loss of the calpain substrate microtubule-associated protein-2 (MAP-2) immunohistochemistry using volumetry in serial slices of the brains. Furthermore μ-calpain positive-stained cells were detected by immunohistochemistry and western blotting.
Results: In placebo-treated animals the μ-calpain expression was significantly increased in the ischemic hemisphere compared with the contralateral non-ischemic hemisphere (88.6 versus 70.5% in the basal ganglia, 60.7 versus 10.7% in the cortex, p
Discussion: The present data indicate that μ-calpain proteolysis plays an important role in the chain of events following cerebral ischemia. However, the calpain inhibitor A-558693 failed to prevent these changes. [Neurol Res 2005; 27: 466-470]
Keywords: Calpain inhibitor; middle cerebral artery occlusion; immunohistochemistry; MAP-2
INTRODUCTION
Various mechanisms are involved in the pathophysiological alterations that result from focal cerebral ischemia. These include impaired cerebral blood flow, increased intracellular levels of Na+ and Ca^sup 2+^ and cytoskeletal degradation1-4. The increase of intracellular Ca^sup 2+^ especially contributes to an activation of some members of the calpain family that consist of neutral cysteine proteases5. Calpains represent a family of nonlysosomal cysteine proteases of which several members have been reported. The most important calpains consist of μ-calpain and m-calpain. The proteolytic activity of μ-calpain, which needs micromolar concentrations of calcium for activation, and also m-calpain, which needs millimolar concentrations of calcium, substantially increases after ischemic6,7 or traumatic8 brain injury. Activated calpain affects several substrates, many of which are cytoskeletal proteins such as spectrin, microtubule-associated protein 2 (MAP-2), as well as the neurofilament proteins NF68 and NF200(9-12).
Global inhibition of these proteases might have beneficial effects in focal cerebral ischemia. This was recently shown by our group in a model of cerebral ischemia, in which hypothermia reduced the μ-calpain expression in the ischemic hemisphere13. In addition pharmacological inhibition of calpains has been of interest in drug discovery research for many years, however up to now, no clinical trial investigating the effect of calpain inhibitors has been reported. Nevertheless, in experimental studies calpain inhibition could lead to a significant reduction in infarct size after focal cerebral ischemia. For example, it has been shown that administration of the calpain inhibitor Cbz-Val-PheH before ischemia can significantly reduce the infarct volume14. Another calpain inhibitor (AK 295) was shown to be effective even several hours after initiation of cerebral ischemia15017. However, most of the investigated calpain inhibitors are not specific against calpain, and therefore the observed effect might be due to a broad inhibition of several proteases.
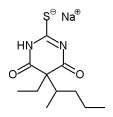
The aim of our study was to show the immunohistochemical expression of μ-calpain and its effect on the substrate MAP-2 in an experimental model of focal cerebral ischemia in rats and to evaluate the efficacy of A-558693, a novel specific benzoylalanine-derived ketoamide calpain inhibitor18, when administered 150 minutes after initiation of ischemia.
METHODS
Rat model of transient focal cerebral ischemia
Adult male Wistar rats were anesthetized with thiopental (100 mg/kg intraperitoneally), tracheotomized, and artificially ventilated with an animal ventilator. The right femoral vein was cannulated to provide fluid substitution. A catheter was inserted into the right femoral artery to allow the continuous measurement of arterial blood pressure and blood gases. The rats were kept at a constant temperature of ~37°C using a feedback heating pad.
Transient focal cerebral ischemia was induced by a modified method of intraluminal vascular occlusion19. Briefly, the left common carotid artery was ligated and cannulated with a polyethylene tube (Ethicon, Norderstedt, Germany), through which a 3-0 surgical nylon suture with a thickened tip was inserted ~2830 mm from the bifurcation of the common carotid artery, toward the intracranial part of the internal carotid artery to occlude the middle cerebral artery (MCA). Reperfusion was initiated by retracting the suture toward the base of the skull and allowing recirculation via the circle of Willis. At the end of the experiment, the brain was perfused with a 1 % albumin solution and was frozen at -80°C. The base of the skull was inspected to exclude hemorrhagic infarction. The brains were cut in a cryostat at -18°C, and 10-µm-thick sections were collected on pre-labeled, warm glass slides. After circa 50 consecutive sections, two sections were used for the volumetry, while the remaining sections were used for other examinations. All animal procedures were approved by the government of Upper Bavaria and were performed in accordance with the European Communities Council Directive. In accordance with these standards, every effort was made to reduce the number of animals used and to ensure that they were free of pain or discomfort.
Calpain inhibitor
The calpain inhibitor A-558693 was synthesized as described in detail18. The compound carries ketoamide as the functional group. The inhibition of human and rat μ-calpain is in the low nanomolar range with K1 values for the different species of 18.3 and 18.8 nM, respectively. The cysteine proteases cathepsin B and cathepsin L are inhibited between 5- and 8-fold less, while the yeast proteasome is not even inhibited at 100 µM concentrations by this compound. A-558693 shows considerable water-solubility at neutral pH-values, which enabled the intravenous application of aqueous solutions.
Experimental groups
Two experimental groups were set up. The first group of six animals served as controls, receiving no calpain inhibitor. The second group of six animals was treated with the calpain inhibitor A-558693. The inhibitor was given in a dose of 10 mg/kg body weight as a bolus over 5 minutes, 150 minutes after initiation of ischemia, and 30 minutes before starting reperfusion of the MCA. Afterwards a continuous infusion of 5 mg/kg body weight per hour was administered for 24 hours. All animals were subjected to 3 hours of ischemia followed by 24 hours of reperfusion.
Antibodies and immunohistochemistry
Neuronal injury was detected by immunohistochemical staining using a monoclonal antibody against MAP-2 (Boehringer Mannheim, Germany). MAP-2 is a cytoskeletal protein, which is degraded by activated proteinases in the early phases of ischemia. While the antibody used does not detect digested protein, areas with neuronal damage show a loss of staining. These areas of MAP-2 demarcation were defined as regions of interest, in which calpain activation was evaluated and compared with the contralateral hemispheres. Consecutive sections underwent immunohistochemical staining for μ-calpain to detect the presence of intracellular proteases in these defined areas. Calpainpositive cells were identified with a polyclonal rabbit μcalpain antibody against the inactive large subunit (80 kDa, R&D Laboratories, Munich, Germany).
Sections were fixed with acetone/chloroform for 5 minutes at +4°C and immersed in 100 mM/l glycine in phosphate buffer solution (PBS) for 10 minutes. Sections were rinsed in PBS wash solution and then incubated with Blotto for 20 minutes to reduce nonspecific binding. Each section was incubated with 150 µm of the primary antibody solution for over 2 hours at 37°C. The working concentration of the primary antibody was 1 : 50 for μ-calpain and 1 : 800 for MAP-2. After the sections had been washed with PBS, they were incubated with either biotinylated goat serum against rabbit IgG or biotinylated horse serum against mouse IgG for 30 minutes at 37°C (Vector Laboratories). Vectastain ABC reagent was added for 30 minutes at 37°C after rinsing the sections with PBS. Chromogen (AEC Kit Biomeda Corp.) was used to develop the peroxidase signal. All sections were counterstained with Mayer's Hematoxylin (Sigma) for 30 seconds, blued in saturated sodium bicarbonate, and mounted on crystal slides. Negative and positive controls were routinely performed in each staining experiment.
Videoimaging and microscopy
For the analyses light microscopy was used (Zeiss, Axioskop 2, Germany), together with a photo camera (Sony, PowerHAD, Japan). The numbers of peroxidasestained cells were calculated with a computerized videoimaging system (Optimas Software, Version 6.5 from Media Cybernetics Silver Spring, USA). To determine the calpain-positive cells, the relative intensity of the staining coefficient algorithm (RISC) was used20. RISC was determined by calculating the decimal logarithm of the quotient of the background staining to the staining by calpain-positive cells.
Western blotting
Protein isolation and western blotting were performed as described elsewhere21. Blots were first incubated with rabbit anti-μ-calpain antibodies at a dilution of 1:1000 (R&D Laboratories, Munich, Germany), and subsequently with biotinylated anti-rabbit antibody (Vector Laboratories, Burlingame, CA, USA). Each blot 'is representative of at least three experiments. An optical analysis program (Tina version 2.08, Raytest lsotopenmessgerate GmbH, Munich, Germany) was used to compare the different bands by optical densitometry. Results were displayed on an arbitrary optical density scale. To allow comparison over multiple samples run in different gels, the amount of proteins in the ischemic side was normalized by dividing it by the amount of protein in the non-ischemic side.
Ischemic and non-ischemic material from the same animal was analyzed in the same gel to allow unbiased calculation of the ratio ischemic side to non-ischemic side.
Volumetry
To calculate the lesion volume, all sections for volumetry with MAP-2 immunohistochemistry were first scanned using a standard flatbet scanner. The files were imported into Optimas 6.5-imaging software, the lesioned areas delineated, and the size converted to the metric system. Next, for every detection method, the partial volume between two adjacent sections was computed using the formula for a conic section:
(Area^sub i-1^ + Area^sub i^ +,/Area^sub i-1^ × Area^sub i^)/3 × (distance between sections)^sub i-1,i^
with Area^sub 1,2,3^,...,n-i being the area of the lesion of the serial sections detected by the same method, and Area^sub 0^ and Arean are the first and last section without a lesion. Then all partial volumes were added to find the total lesion volume22.
Statistical analysis
Data were expressed as mean+ SD. Comparisons between values from infarcted and control areas as well as comparisons of cerebral infarct size and calpain breakdown between the calpain inhibitor and placebotreated animals were made with the ?-test using a level of significance of 5%.
RESULTS
Expression of μ-calpain in cerebral ischemia by immunohistochemistry and western blotting
Calpain-positive-stained cells were rarely determined in the non-ischemic hemisphere. Basal ganglia and the cortex of placebo-treated animals showed a significant increase of calpain expression on the ische;mic side (88.6 versus 10.5% in basal ganglia, 60.7 versus 10.7% in the cortex, p
Effect of calpain inhibitor A-558693 on the calpain expression and the infarct size
A-558693-treated animals showed a trend for fewer calpain-positive cells in the basal ganglia of the ischemic side. RISC in the basal ganglia was 0.22±0.09 in animals receiving the calpain inhibitor (CI) and 0.34 ± 0.10 in the placebo-treated animals (p=0.06). The RISC in the cortex of Cl rats was 0.11+0.07 compared with 0.22±0.09 in placebotreated animals (n.s.). The ratio of calpain-positive and total cells in the basal ganglia and the cortex did not significantly differ between these two groups (Figures 1 and 2).
The western blot analysis for anti-μ-calpain revealed no significant difference between the A-558693-treated animals in the ischemic hemisphere compared with the placebo-treated animals, whether in the cortex or in the basal ganglia. The amount of calpain in the cortex was increased to 170±32% in A-558693, and to 141 ±11% in the placebo-treated animals (n.s.). The increase of calpain in the ischemic basal ganglia of the calpaininhibitor group was 171 ±30% compared with 164± 26% in the placebo group (n.s.), see Figure 3.
To determine the infarct volume, MAP-2 a substrate of the calpains was used. MAP-2 immunohistochemistry revealed that the infarct volume, determined by volumetric analysis based on a conic section, in the A558693-treated animals tended to be smaller than in the control animals (148±84 versus 207±110 mm^sup 3^). Due to a large standard deviation this difference was not significant (p=0.34).
DISCUSSION
The main finding of this study is that the calpain inhibitor A-558693, administered 150 minutes after initiation of ischemia, had no significant effect on the infarct size or the expression of calpain in this animal model of focal cerebral ischemia. However, there was a trend to smaller infarcts and also fewer calpain-positive cells in the calpain-inhibitor group.
Our data on the increased calpain expression in the ischemic area agree with the breakdown of the calpain substrate MAP-2 in the placebo group, as well as in the calpain-inhibitor-treated group. The calpain-positive cells were mainly detected in the basal ganglia, but also in the cortex on the ischémie side. This pattern of μ-calpain expression is in accordance with the timedependent increase of m-calpain7 and μ-calpain13 expression in focal cerebral ischemia in rats and the increase of μ-calpain in an animal model of cerebral venous thrombosis23. The increase in μ-calpain expression in the ischemic area was accompanied by a loss of its substrate MAP-2. It is well known that prolonged calpain-mediated breakdown of substrates occurred after experimental traumatic brain injury or after focal cerebral ischemia in rats6'24, thus our data are in accordance with these reports.
The calpain inhibitor A-558693 had no significant effect on the infarct size or on the expression of calpains after 150 minutes of ischemia and 24 hours of reperfusion, despite a trend to smaller infarcts and less calpainpositive cells. Our results contradict those of other studies, reporting a reduction of infarct size by calpain inhibitors. When MDL281 70/Cbz-Val-Phe-H was given 30 minutes before vessel occlusion, the rats exhibited significantly smaller volumes of cerebral infarction14. Bartus and co-workers also showed that the administration of calpain inhibitors AK 275 and AK 295 after initiation of ischemia can reduce the infarct volume up to 75 and 30%, respectively15,16. Markgraf and his group postulated a period of ~6 hours for calpain inhibition in focal cerebral ischemia in rats17. All of these studies measured the infarct volume by the TTC method, a macroscopic method that does not permit evaluation of cell damage on a microscopic scale. In contrast, our results were based on a more detailed histological analysis of the post-ischemic damage. We determined the volumetric infarct by the breakdown of the calpain substrate MAP-2, and also performed a quantitative analysis of the calpain expression in the ischemic hemisphere by immunohistochemistry and western blotting. Despite these various techniques for identifying cerebral injury we were not able to show any significant effect of the calpain inhibitor. In contrast to our data, one group showed a reduction of the necrotic cells in the cortex in an animal model of global cerebral ischemia using the calpain inhibitor MDL28170, although these authors did not directly assess the effect on the calpain expression25.
There might be several reasons for our failure to demonstrate the efficacy of this new calpain inhibitor A558693. First, the calpain inhibitor A-558693 is a very potent and specific inhibitor against calpains. This is in contrast to other inhibitors with a broader spectrum and inhibition of other proteases, like cathepsins. Therefore, inhibition of calpains might not be effective enough to stop the progression of the infarct size. However, specific calpain inhibition might be an effective strategy in other cerebral diseases like traumatic brain injury, as one study was able to demonstrate a reduction in the total numbers of damaged neurons by 41 % by the use of a ketoamid-calpain inhibitor18. Another reason might be that the calpain inhibitor was given 150 minutes after ischemia, while most of the previous studies administered the inhibitor before or shortly after initiation of ischemia. However, one study showed a significant reduction of infarct size even 6 hours after initiation of ischemia with the calpain inhibitor MDL28, 1 70. But as mentioned before MDL28, 170 has a more broad inhibitory effect and might be therefore effective even after late administration.
Our study has some limitations. First, the administration of the calpain inhibitor 150 minutes after initiation of ischemia seems to be too late, as the time window for this specific calpain inhibitor might be shorter; however, we tried to be as close to human settings, and therefore administration before or shortly after initiation of ischemia might be effective, but clinically irrelevant. secondly, we cannot exclude that the determination of the infarct size by one substrate of the calpains will be representative for the infarct size. Therefore, our tissuesaving volumetric access of determination of the infarct size might not be strictly comparable with other studies that showed a reduction in infarct volume, for example by TTC staining. However, in our previous study we found a good correlation between the loss of MAP-2 and infarct size using MRI22. In addition, as MAP-2 is a substrate of activated calpains, the effect of calpain inhibitors might be even more pronounced by determination of directly related substrates. Therefore, we consider the loss of MAP-2 to be a relevant postischemic event.
The present data indicate that μ-calpain proteolysis plays an important role in the chain of events following experimental cerebral ischemia and the subsequent loss of its substrate MAP-2. On the basis of measurements of infarct volumetry by the loss of the calpain substrate MAP-2, the expression of calpains by immunohistochemistry and western blotting, we were not able to establish a neuroprotective effect of the calpain inhibitor A-558693 in our model.
ACKNOWLEDGEMENTS
This work was supported in part by the Deutsche Forschungsgemeinschaft Ha.2078/8-1. Calpain inhibitor A-558693 was performed from Abbott GmbH, Ludwigshafen.
REFERENCES
1 Croall DE, DeMartino GN. Calcium-activated neutral protease (calpain) system: Structure, function, and regulation. Physiol Rev 1991; 7T: 813-847
2 Takagaki Y, Itoh Y, Aoki Y, ef al. Inhibition of ischemia-induced fodrin breakdown by a novel phenylpyrimidine derivative NS-7: An implication for its neuroprotective action in rats with middle cerebral artery occlusion. J Neurochem 1997; 68: 2507-2513
3 Saatman KE, Bozyczko CD, Marcy V, et ai. Prolonged calpainmediated spectrin breakdown occurs regionally following experimental brain injury in the rat. J Neuropathol Exp Neurol 1996; 55: 850-860
4 Siman R, Card JP, Davis LG. Proteolytic processing of beta-amyloid precursor by calpain I. J Neurosci 1990; 10: 2400-2411
5 Zivin JA, Choi DW. Stroke therapy. Sd Am 1991; 265: 56-63
6 Bartus RT, Dean RL, Cavanaugh K, et al. Time-related neuronal changes following middle cerebral artery occlusion: Implications for therapeutic intervention and the role of calpain. J Cereb Blood FlowMetab 1995; 15: 969-979
7 Liebetrau M, Staufer B, Auerswald EA, et al. Increased intracellular calpain detection in experimental focal cerebral ischemia. Neuroreport 1999; 10: 529-534
8 Kampfl A, Posmantur RM, Zhao X, et al. Mechanisms of calpain proteolysis following traumatic brain injury: Implications for pathology and therapy: A review and update. ) Neurotrauma 1997; 14: 121-134
9 Saido TC, Sorimachi H, Suzuki K. Calpain: New perspectives in molecular diversity and physiological-pathological involvement. FASEB J 1994; 8: 814-822
10 Dawson DA, Hallenbeck JM. Acute focal ischemia-induced alterations in MAP2 immunostaining: Description of temporal changes and utilization as a marker for volumetric assessment of acute brain injury, y Cereb Blood Flow Metab 1996; 16: 170-174
11 Posmantur R, Kampfl A, Siman R, et al. A calpain inhibitor attenuates cortical cytoskeletal protein loss after experimental traumatic brain injury in the rat. Neuroscience 1997; 77: 875-888
12 Lofvenberg L, Backman L. Calpain-induced proteolysis of betaspectrins. FfBS Lett 1999; 443: 89-92
13 Liebetrau M, Burggraf D, Martens HK, et al. Delayed moderate hypothermia reduces calpain activity and breakdown of its substrate in experimental focal cerebral ischemia in rats. Neurosci Lett 2004; 357: 17-20
14 Hong SC, Goto Y, Lanzino G, et al. Neuroprotection with a calpain inhibitor in a model of focal cerebral ischemia. Stroke 1994; 25: 663-669
15 Bartus RT, Baker KL, Heiser AD, et al. Postischemic administration of AK275, a calpain inhibitor, provides substantial protection against focal ischemic brain damage. J Cereb Blood Flow Metab 1994; 14: 537-544
16 Bartus RT, Hayward NJ, Elliott PJ, et al. Calpain inhibitor AK295 protects neurons from focal brain ischemia. Effects of postocclusion intra-arterial administration. Stroke 1994; 25: 2265-2270
17 Markgraf CG, Velayo NL, Johnson MP, et al. Six-hour window of opportunity for calpain inhibition in focal cerebral ischemia in rats. Stroke 1998; 29: 152-158
18 Lubisch W, Beckenbach E, Bopp S, et al. Benzoylalanine-derived ketoamides carrying vinylbenzyl amino residues: Discovery of potent water-soluble calpain inhibitors with oral bioavailability. J Med Chem 2003; 46: 2404-2412
19 Longa EZ, Weinstein PR, Carlson S, et al. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 1989; 20: 84-91
20 MollerJC, Klein MA, Haas S, et al. Regulation of thrombospondin in the regenerating mouse facial motor nucleus. CHa 1996; 17: 121-132
21 Hamann GF, Liebetrau M, Martens H, et al. Microvascular basal lamina injury after experimental focal cerebral ischemia and reperfusion in the rat. J Cereb Blood Flow Metab 2002; 22: 526533
22 Kloss CU, Thomassen N, Fesl G, et al. Tissue-saving infarct volumetry using histochemistry validated by MRI in rat focal ischemia. Neurol Res 2002; 24: 713-718
23 Liebetrau M, Gabriejcic-Geiger D, Meyer P, et al. Increased calpain expression following experimental cerebral venous thrombosis in rats. Thromb Res 2003; 112: 239-243
24 Pettigrew LC, Holtz ML, Craddock SD, ef ai. Microtubular proteolysis in focal cerebral ischemia. I Cereb Blood Flow Metab 1996; 16: 1189-1202
25 Li PA, Howlett W, He QP, et al. Postischemic treatment with calpain inhibitor MDL 281 70 ameliorates brain damage in a gerbil model of global ischemia. Neurosci Lett 1 998; 247: 1 7-20
Martin Liebetrau, Helge Martens, Nora Thomassen, Dorothe Burggraf*, Dusica Gabrijelcic-Geiger[dagger], Wolfgang Lubisch[dagger], Achim Möller and Gerhard F. Hamann
Department of Neurology, Klinikum Crosshadern, Ludwig-Maximilians-University, Munich, Germany, *Department of Clinical Chemistry and Clinical Biochemistry of the Surgery Clinic, Klinikum Innenstadt, Ludwig-Maximilians-University, Munich, Germany and tNeuroscience Discovery Research, Abbott GmbH and Co. KG, Ludwigshafen, Germany
Correspondence and reprint requests to: Prof. Dr G. F. Hamann, Department of Neurology, Klinikum Grosshadern, LudwigMaximilians University, Marchioninistr. 15, 81377 Munich, Germany, [gerhard.hamann@med.uni-muenchen.de] Accepted for publication October 2004.
Copyright Maney Publishing Jul 2005
Provided by ProQuest Information and Learning Company. All rights Reserved