A 60-year-old man presented to an outside facility with hypercapnic respiratory failure requiring intubation and mechanical ventilation. He underwent diuresis for a presumptive diagnosis of congestive heart failure, was extubated, and was transferred to our university hospital for cardiac catheterization.
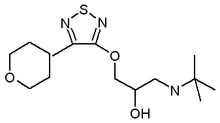
His dyspnea had been progressive over many years and was refractory to adjustments in his cardiac medications. A recent nuclear stress test showed reversible ischemia. He had a 20-year history of hypertension and diabetes mellitus with progressive nephropathy and retinopathy. He had a 100 pack-year smoking history and a remote asbestos exposure as a member of the Merchant Marine. Outpatient medications were rosiglitazone, 4 mg qd, quinapril, 10 mg qd, carvedilol, 6.25 mg bid, torsemide, 100 mg qd, metolazone, 5 mg qd, and timolol ophthalmic drops.
Cardiac catheterization revealed two-vessel coronary artery disease. Left ventricular pressures were as follows: systolic, 141 mm Hg; diastolic, 15 mm Hg; and end-diastolic, 20 mm Hg. The performance of a ventriculogram was deferred secondary to renal insufficiency. An echocardiogram demonstrated preserved left ventricular systolic function with normal chamber size and wall thickness. There was right atrial and ventricular enlargement, and pulmonary artery systolic pressure was estimated to be 30 mm Hg. Coronary stents were placed into the left anterior descending and right coronary arteries.
Several hours after undergoing the procedure, the patient's dyspnea worsened, and he required reintubation. Prior to intubation, arterial blood gas levels while breathing room air were as follows: pH, 7.20; P[CO.sub.2], 78 mm Hg; P[O.sub.2], 49 mm Hg; bicarbonate, 30 mm Hg; and oxygen saturation, 73%. He was admitted to the coronary care unit. His ECG was unchanged from baseline. Puhnonary edema secondary to procedural hydration was suspected. He did not improve despite aggressive diuresis, and a pulmonary consultation was requested.
Physical Examination
The patient was intubated and sedated. Vital signs revealed a BP of 96/57 mm Hg, a pulse of 66 beats/min, a temperature of 98.9[degrees]F, and a respiratory rate of 14 breaths/min. His neck veins were not engorged, although prominent pulsations were visible. A lung examination showed bilateral coarse crackles. He had a normal chest wall without evidence of kyphoscoliosis. A cardiovascular examination revealed a loud [S.sub.2] and a systolic ejection murmur III/VI. The results of an abdominal examination were unremarkable. His lower extremities showed 2+ edema. The results of a neurologic examination were normal without muscle weakness or focal deficit. His fingers did not demonstrate clubbing.
The patient was receiving continuous mandatory mechanical ventilation with a set tidal volume (VT) of 700 mL, a set respiration rate of 10 breaths/rain, and a positive end-expiratory pressure (PEEP) of 5 cm [H.sub.2]O. Peak inspiratory pressure (PIP) was 56 cm [H.sub.2]O, plateau pressure (Pplat) was 48 cm [H.sub.2]O. VT was lowered to 550 mL, resulting in a PIP of 45 cm [H.sub.2]O and a Pplat of 42 cm [H.sub.2]0. Static compliance of the respiratory system (Cstat,rs) was 15 mL/cm [H.sub.2]0.
Radiology
A chest radiograph demonstrated increased markings throughout both lungs fields (but more prominently at the bases), cardiomegaly, and bilateral pleural effusions, with the left being larger than the right (Fig 1). These findings were essentially unchanged from those of radiographs taken 1 year prior to hospital admission.
Laboratory Findings
The laboratory findings were as follows: serum sodium, 141 mmol/dL; potassium, 4.2 retool/dL; chloride, 102 mmol/dL; bicarbonate, 27 mmol/dL; BUN, 72 mg/dL; creatinine, 2.3 mg/dL; total WBC count, 4,400 x [10.sup.3] cells/[micro]L; and hematoerit, 32.8%. Left pleural fluid was transudative, with a WBC count of 3 cells/[micro]L, 22% neutrophils, and 78% monocytes.
Pulmonary Artery Catheter Data
A pulmonary artery catheter was placed. Waveform tracings were recorded (Fig 2), and the following measurements made: cardiac output, 3.9 L/min; cardiac index, 2.0 L/min/[m.sup.2]; central venous pressure (CVP), 2 mm Hg; pulmonary artery pressure, 49/22 mm Hg; and pulmonary artery occlusion pressure (PAOP), 8 mm Hg.
[FIGURE 2 OMITTED]
Based on the clinical presentation and pulmonary artery catheter information (including the interpretation of the waveforms):
1. What is the physiologic cause of this patient's respiratory failure?
2. Which diagnostic/therapeutic procedure is indicated?
Answer: Cause of respiratory failure is chest wall restriction
A marked rise on the PAOP waveform during inspiration and a low Cstat,rs strongly implicate an abnormality of the chest wall. As the thoracic cage had no gross deformity, pleural disease was suspected. A chest CT scan demonstrated loculated pleural effusions and pleural thickening without calcification. (Fig 3). An exploratory thoracotomy revealed a fusion of the visceral and parietal pleura resulting in severe restriction of the lung.
[FIGURE 3 OMITTED]
Final diagnosis is bilateral diffuse pleural fibrosis, likely asbestos-related
A left thoracotomy was performed. The visceral and parietal pleura were fused and thickened. This process extended throughout the chest and involved the pericardium. The pleura were described as feeling like a "leather bag." A pleural biopsy specimen showed fibrosis without active inflammation (Fig 4). No asbestos fibers were seen. An attempt at decortication was unsuccessful in expanding the lung volumes to any measurable degree. The patient underwent tracheostomy placement and was transferred to the long-term ventilator unit. He died 2 months later from pneumonia.
[FIGURE 4 OMITTED]
An autopsy confirmed the operative findings. Both lungs were entrapped by a constricting fibrosis (Fig 5). The lung parenehyma was normal, except for mild subpleural fibrosis. The pericardium was involved, encircling the heart, but the epicardium was normal, without evidence of constrictive pericarditis. There were no asbestos bodies or calcification in the pleura. Pathologically, the process was most compatible with asbestos-related diffuse pleural fibrosis.
[FIGURE 5 OMITTED]
DISCUSSION
A careful interpretation of the physiologic data was instrumental in determining the cause of respiratory failure in this patient. Patients in the ICU are connected to multiple monitoring devices, but the data are often not fully analyzed. Patients with hypercapnic respiratory failure have abnormalities of the central drive, ventilatory muscle dysfunction, or increased respiratory workload, and patients may have a combination of all three. The elevated inspiratory respiratory workload is from increased elastic, resistive, inertial, or threshold forces. Increased elastic load was a major contributor to this patient's respiratory failure, as was evident from the severely reduced Cstat,rs.
Parenchymal lung disease is the cause of low Cstat,rs in most patients with acute respiratory failure. However, abnormalities of the chest wall are common in patients with chronic respiratory failure. Chest wall disease is usually overt on physical examination or chest radiography (eg, morbid obesity, kyphoscoliosis, or pleural effusions). The relationship of Cstat,rs to static lung compliance (Cstat,lung) and static chest wall compliance (Cstat,chest wall) is as follows: 1/Cstat,rs = 1 / Cstat,lung + 1/Cstat,chest wall.
During mechanical ventilation, the extent that alveolar pressure is transmitted to the pleura is determined by the elasticity of the lung and chest wall. The index of transmission (IT), which is calculated as (end-inspiratory pleural pressure--end-expiratory pleural pressure)/(Pplat - PEEP), is equal to (Cstat,lung)/(Cstat,lung + Cstat,chest wall). IT is normally 50%, as the lung and chest wall have similar static compliance at functional residual capacity. Patients with stiff lungs have less transmission and a lower IT, and patients with a stiff chest wall have more transmission and a higher IT.
An IT of alveolar pressure to the PAOP (IT,PAOP) also can be calculated, as follows: IT,PAOP = (end-inspiratory PAOP [PAOPend-inspiratory]end-expiratory PAOP [PAOPend-expiratory])/ (Pplat - PEEP). When a pulmonary artery catheter balloon is inflated, there is no flow distal to the balloon. PAOPend-expiratory equals left atrial pressure in the absence of PEEP. PAOP rises during mechanical ventilation. PAOPend-inspiratory is dependent on Pplat and on the degree of pressure transmission across the pulmonary vasculature. The extent of transmission is proportional to Cstat,lung. The concordance between IT and IT,PAOP has not been fully evaluated.
Using the data from Figure 2, top, pressure of 25 mm Hg (PAOPend-inspiratory, 34 mm Hg; PAOPend-expiratory, 9 mm Hg) was transmitted to the vaseulature by a mechanical breath that raised the alveolar pressure by 37 cm [H.sub.2]O (Pplat, 42 cm [H.sub.2]O; PEEP, 5 cm [H.sub.2]O). Using the conversion of 1.34 cm [H.sub.2]O = 1 mm Hg, IT,PAOP was 91% (ie, 25 mm Hg X 1.34/37 cm [H.sub.2]O). This is consistent with a normal Cstat,lung. The reduction in Cstat,rs therefore must be explained by a severely reduced Cstat,chest wall.
Care must be taken regarding the definition of the terms lung and chest wall. Generally, the thorax is considered to be a single compartment. The increase in lung volume during inspiration affects other intrathoracic structures. Compliant intrathoracic structures are compressed and transmit a rise in pressure.
This patient's pleura were fused, and his pleural space was obliterated. During inspiration, an expanding lung would only compress those structures within the encircling band of extraparenchymal fibrosis. The high IT,PAOP seen in the pulmonary artery tracing during balloon occlusion was due to compression of the downstream pulmonary vasculature. CVP, right ventricular pressure, and pulmonary artery pressure mirrored the inspiratory rise in PAOP (Fig 2), suggesting that the heart and great vessels were similarly compressed by lung inflation. At autopsy, the parietal pericardium was fused tightly to the pleura. Structures outside the fibrotic pleura were not compressed by lung inflation and would not be expected to transmit a rise in pressure. In this patient, IT calculated using esophageal pressure would likely have been very low as the esophagus was outside the pleural fibrosis at autopsy.
CVP monitoring is commonly performed in the ICU and provides very useful information. CVP has been shown to be more predictive than PAOP in predicting fluid responsiveness, and the importance of CVP in assessing cardiac function has been stressed. In this patient, the proper interpretation of the large inspiratory swings in CVP with mechanical ventilation would have argued strongly against pulmonary edema by demonstrating a normal Cstat,lung.
Pleural thickening and fibrosis can occur from infection, radiation, trauma, connective tissue diseases, drugs, malignancy, and asbestos exposure. Asbestos is the most common cause of bilateral pleural fibrosis and is the most likely agent to cause restrictive impairment in the absence of significant radiologie evidence. Cryptogenic bilateral pleural fibrosis has been reported in four patients without asbestos exposure who presented with elevated erythrocyte sedimentation rate and chest pain, and responded to therapy with cortieosteroids. An inflammatory cause for the condition was postulated.
Patients with bilateral fibrothorax may develop hypercapnic respiratory failure, cor pulmonale, and pulmonary hypertension. The highly negative pleural pressure causes transudative effusions in areas in which the pleura are not fused. Diffuse pleural thickening should be considered if (1) there is a smooth uninterrupted pleural opacity over at least one quarter of the chest wall or (2) pleural thickening extends > 8 cm craniocaudally and 5 cm laterally, and is 3 mm thick. Puhnonary function testing reveals reduced lung volmnes that are consistent with restrictive dysfunction.
Thoracotomy with pleurectomy is recommended for treatment, provided there is a plane of separation between the visceral pleura and adjacent lung. Although a clinical response to decortication has been reported, the morbidity and mortality of this procedure is high, and patients have significant residual restrictive dysfunction. When the peel is adherent such that no tissue plane can be developed, subpleural resection has been proposed, provided that a limited surface area is involved. Others have proposed crisscross, grid-like incisions allowing the lung to expand with limited success. One series reported a benefit from long-term noninvasive mechanical ventilation for patients with hypercapnic respiratory insufficiency from asbestos-related pleural fibrosis.
CLINICAL PEARLS
1. In patients' receiving mechanical ventilation, a reduced static compliance is indicative of parenchymal disease, chest wall disease, or both.
2. In patients, with chest wall diseases, there is a high transmission of alveolar pressure to the pulmonary vasculature, resulting in dramatic pulmonary artery pressure swings' during inspiration. In patients with parenchymal diseases, the transmission is attenuated.
3. A careful interpretation of hemodynamic and physiologic data is essential in the evaluation and management of critically ill patients. An analysis hemodynamic waveforms provides useful information above and beyond the filling pressure.
4. In patients with asbestos-related pleural fibrosis, the radiographic findings can be subtle even when the process is sufficient to cause hypercapnic respiratory failure.
* From the Division of Pulmonary and Critical Care Medicine (Drs. Baram, Degene, Amin, and Smaldone), and the Division of Cardiothoraeic Surgery (Dr. Bilfinger), State University of New York-Stony Brook, Stony Brook, NY.
SUGGESTED READING
Aldrich TK, Prezant DJ. Indications for mechanical ventilation. In: Tobin MJ, ed. Principles and practice of mechanical ventilation. New York, NY: McGraw-Hill, 1994; 155-189
Buchanan DR, Johnston ID, Kerr IH, et al. Cryptogenic bilateral fibrosing pleuritis. Br J Dis Chest 1988; 82:186-193
Chapin JC, Down JB, Douglas ME, et al. Lung expansion, airway pressure transmission and positive end-expiratory pressure. Arch Surg 1979; 114:1193-1197
Dernevik L, Gatzinsky P. Long-term results of operation for shrinking pleuritis with atelectasis. Thorax 1985; 40:448-445
Gamsu G, Aberle DR, Lynch D. Computed tomography in the diagnosis of asbestos-related disease. J Thorac Imaging 1989; 4:61-67
Hall DR, Morrison JB, Edwards FR. Pleural fibrosis after practolol therapy. Thorax 1978; 33:822-824
Hasan F, Weiss WB, Braman S, et al. Influence of lung injury on pulmonary wedge-left atrial pressure correlation during positive end-expiratory pressure ventilation. Am Rev Respir Dis 1985; 131:246-250
Hindle W, Posner E, Sweetnam MT, et al. Pleural effusion and fibrosis during treatment with methysergide. BMJ 1970; 1:605-606
Jardin F, Genevray B, Brun-Ney D, et al. Influence of lung and chest wall compliances on transmission of airway pressure to the pleural space in critically ill patients. Chest 1985; 88:653-656
Macfarlane JD, Dieppe PA, Rigden BG, et al. Pulmonary and pleura lesions in rheumatoid disease. Br J Dis Chest 1978; 72:39-56
Magder S, Georgiadis G, Cheong T. Respiratory variations in right atrial pressure predict the response to fluid challenge. J Crit Care 1992; 7:76-85
Magder S. More respect for the CVP. Intensive Care Med 1998; 24:651-653
Miller A, Tierstein AST, Selikoff IJ. Ventilatory failure due to asbestos pleurisy. Am J Med 1983; 75:911-919
Munoz X, Roger A, Pallisa E, et al. Ventilatory insufficiency due to asbestos-related diffuse pleural fibrosis successfully treated with noninvasive home mechanical ventilation. Respiration 2001; 68:533-536
O'Quin R, Marini JJ. Pulmonary artery occlusion pressure: clinical physiology, measurement and interpretation. Am Rev Respir Dis 1983; 128:319--326
Petro W, Maassen W, Greschuchna D, et al. Regional and global lung function in unilateral fibrothorax after conservative therapy and decortication. Thorac Cardiovasc Surg 1982; 30:137-141
Pien GW, Gant MJ, Washam CL, et al. Use of an implantable pleural catheter for trapped lung syndrome in patients with malignant pleural effusion. Chest 2001; 119:1641-1646
Scannell JG: Indications for and techniques of decortication. In: Deslaurier J, Laquet LK, eds. Trends in general thoracic surgery (vol 6): thoracic surgery; surgical management of pleural diseases. St. Louis, MO: Mosby, 1990
Schwartz DA, Fuortes LJ, Galvin JR, et al. Asbestos-induced pleural fibrosis and impaired lung function. Am Rev Respir Dis 1990; 141:321-326
Sharma S, Smith R, Al-Hameed F. Fibrothorax and severe lung restriction secondary to lupus pleuritis and its successful treatment by pleurectomy. Can Respir J 2002; 9:335-337
Teboul JL, Pinsky MR, Mercat A, et al. Estimating cardiac Filling pressure in mechanically ventilated patients with hyperinflation. Crit Care Med 2000; 28:3631-3636
Venus B, Cohen LE, Smith RA. Hemodynamic and intrathoracic pressure transmission during controlled mechanical ventilation and positive end-expiratory pressure in normal and low compliant lungs. Crit Care Med 1998; 16:686-690
Wiggins J, Skinner C. Bromocriptine-induced pleuropulmonary fibrosis. Thorax 1986; 41:328-330
Wright PH, Hanson A, Kreel L, et al. Respiratory function changes after asbestos pleurisy. Thorax 1980; 35:31-36
Yates DH, Browne K, Stidolph PN, et al. Asbestos-related bilateral diffuse pleural thickening: natural history of radiographic and lung function abnormalities. Am J Respir Crit Care 1996; 153:301-306
Young D, Simon J, Pomerantz M. Current indications for and status of decortication for "trapped lung." Ann Thorac Surg 1972; 14:631-634
Manuscript received November 6, 2003; revision accepted January 20, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@ehestnet.org).
Correspondence to: Daniel Baram, MD, FCCP, Assistant Professor of Medicine Division of Pulmonary and Critical Care Medicine, SUNY-Stony Brook T-17 040 HSC Stony Brook, NY 11794-8172; e-mail: daniei.baram@stonybrook.edu
Daniel Baram, MD; FCCP; Aklilu Degene, MD; Mohammad Amin, MD; Thomas Bilfinger, MD, ScD, FCCP; and Gerald Smaldone, MD, PhD, FCCP
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2005 Gale Group