Clostridium difficile is a spore-forming, gram-positive bacillus that produces exotoxins that are pathogenic to humans. C. difficile-associated disease (CDAD) ranges in severity from mild diarrhea to fulminant colitis and death. Antimicrobial use is the primary risk factor for development of CDAD because it disrupts normal bowel flora and promotes C. difficile overgrowth. C. difficile typically has affected older or severely ill patients who are hospital inpatients or residents of long-term-care facilities. Recently, however, both the frequency and severity of health-care-associated CDAD has increased; from 2000 to 2001, the rate of U.S. hospital discharge diagnoses of CDAD increased by 26% (1). One possible explanation for these increases is the emergence of a previously uncommon strain of C. difficile responsible for severe hospital outbreaks (2). Although individual cases of CDAD are not nationally reportable, in 2005, the Pennsylvania Department of Health (PADOH) and CDC received several case reports of serious CDAD in otherwise healthy patients with minimal or no exposure to a health-care setting. An investigation was initiated by the Philadelphia Department of Public Health (PDPH), PADOH, and CDC to determine the scope of the problem and explore a possible change in CDAD epidemiology. This report summarizes the results of the investigation in Pennsylvania and three other states, which indicated the presence of severe CDAD in healthy persons living in the community and peripartum women, two populations previously thought to be at low risk. The findings underscore the importance of judicious antimicrobial use, the need for community clinicians to maintain a higher index of suspicion for CDAD, and the need for surveillance to better understand the changing epidemiology of CDAD.
Case Reports
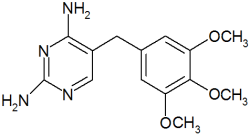
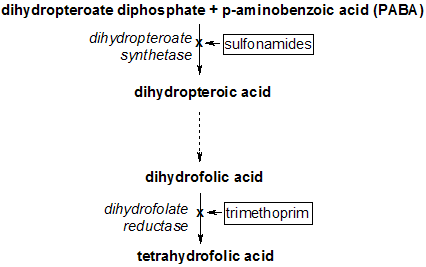
Case 1. A woman aged 31 years who was 14 weeks pregnant with twins went to a local emergency department (ED) after 3 weeks of intermittent diarrhea, followed by 3 days of cramping and watery, black stools 4-5 times daily. Stools specimens tested positive for C. difficile toxin, and the patient was admitted. Her only antimicrobial exposure during the preceding year was trimethoprim-sulfamethoxazole (for a urinary tract infection) approximately 3 months before admission. She was treated with metronidazole and discharged but was readmitted the next day for 18 days with severe colitis, receiving metronidazole, cholestyramine, and oral vancomycin. She improved on vancomycin and was allowed to return home. However, 4 days later she was readmitted with diarrhea and hypotension. She spontaneously aborted her fetuses. Despite aggressive treatment including a subtotal colectomy, intubation, and inotropic medication, the patient died on the third hospital day. Histopathologic examination of the colon demonstrated megacolon with evidence of pseudomembranous colitis.
Case 2. A girl aged 10 years (unrelated and without contact with case 1) went to a children's hospital ED because of intractable diarrhea, projectile vomiting, and abdominal pain. She had not taken antimicrobials during the preceding year. Stool specimens were positive for C. difficile toxin. The child had been healthy until 2 weeks before the ED visit, when she became symptomatic within days of her younger brother having a febrile diarrheal illness. The boy was not on antimicrobials when he became ill. His symptoms resolved within 2-3 days without medical treatment, but his sister had fever as high as 102[degrees]F (39[degrees]C), abdominal pain, and diarrhea. One week into her illness, she was examined by a clinician, who performed a rapid streptococcal antigen test on a swab from her oropharynx; the result was positive. The patient was prescribed amoxicillin but was unable to take it because of her stomach cramps and diarrhea; her symptoms worsened until she was having liquid stools up to 14 times daily. Symptoms resolved with hospital admission and the administration of intravenous fluids, electrolytes, and metronidazole.
Epidemiologic and Laboratory Investigations
In May and June 2005, a request for voluntary reports of peripartum CDAD (i.e., 4 weeks before and after delivery) was initiated by PDPH; case definitions for peripartum CDAD were developed and distributed nationally through the Epidemic Information Exchange (Epi-X) and locally through the PDPH Health Alert Network (HAN). The New Jersey Department of Health and Senior Services also distributed the alert statewide through its HAN system. A separate request for reporting of community-associated CDAD (CA-CDAD) along with a case definition was developed and distributed in June in Philadelphia and four surrounding Pennsylvania counties (Bucks, Chester, Delaware, and Montgomery) through local and statewide HANs (Box).
Detailed, open-ended interviews were conducted with patients who were reported by hospital personnel to state and local health departments after distribution of the notices. Medical details, such as type of antimicrobial agent and duration, were confirmed with treating clinicians whenever possible. To determine the minimum population rate and rate per antimicrobial prescription of CA-CDAD, the number of cases reported from Philadelphia and four surrounding counties were divided by 2004 U.S. census population estimates for these five areas. The number of antimicrobial prescriptions were calculated on the basis of census estimates of the population surveyed, multiplied by national prescribing rate estimates (3). Available toxin-positive stool samples were cultured for C. difficile using standard methods. Isolates underwent pulsed-field gel electrophoresis (PFGE), toxinotyping, and detection of binary toxin and deletions in tcdC, a putative negative regulator of toxin production (2,4).
Ten peripartum and 23 CA-CDAD cases were reported from four states during May-June 2005 (Table 1), with onset dates ranging from February 26, 2003, to June 28, 2005. All but one of the cases occurred during 2004-2005. Age of nonperipartum cases ranged from 6 months to 72 years (mean: 26 years; median: 23 years). Peripartum cases occurred in patients from New Hampshire, New Jersey, Ohio, and Pennsylvania; because CA-CDAD surveillance was conducted only in the greater Philadelphia area, these cases were only from this area. Transmission to close contacts was evident for four cases: two were in children of CDAD patients with peripartum exposures, one was in an adult caring for a hospitalized parent with confirmed CDAD, and one was in an adult who visited a parent with confirmed CDAD in a nursing home. One peripartum mother who transmitted C. difficile to her child also transmitted CDAD to a family friend.
Eight (24%) of 33 patients reported no exposure to antimicrobial agents within 3 months before CDAD onset. Five of these were children, three of whom required hospitalization. Three of the eight cases without exposure to antimicrobial agents occurred in patients who had close contact with a person with diarrheal illness; two of these persons had confirmed CDAD. An additional three (9%) of 33 patients contracted CDAD after receiving [less than or equal to] 3 doses of antimicrobials; two received only 1 dose of clindamycin for group B streptococcus prophylaxis before CDAD onset. Clindamycin was the most common antimicrobial exposure noted; overall, 10 (30%) of 33 cases were in patients who reported exposure to the drug before disease onset; these 10 patients included the two who had [less than or equal to] 3 doses of antimicrobials. Fifteen (46%) patients required hospitalization or an ED visit. Thirteen (39%) patients had a relapse of disease and required antimicrobials.
The estimated minimum annual incidence of CA-CDAD in Philadelphia and its surrounding four counties during July 2004-June 2005 was 7.6 cases per 100,000 population, with one case of CDAD for every 5,549 outpatient antimicrobial prescriptions; this figure is based on national estimates of antimicrobial prescribing in ambulatory settings applied to the Philadelphia area. Two patient isolates were available for characterization and were compared with the recently described "epidemic strain" that has been detected as the cause of either severe hospital outbreaks or hospital-endemic cases of CDAD in 16 states (2; CDC, unpublished data, 2005). Neither shared the same toxinotype as the epidemic strain, but both were binary toxin positive; one isolate, from an Ohio peripartum CDAD case, was >80% related by PFGE to the epidemic strain, and the other, from a Philadelphia-area CA-CDAD case, had an 18-bp deletion in tcdC (Table 2).
Acknowledgments
This report is based, in part, on contributions by the New Hampshire Dept of Health. C Tan, MD, C Booker, MD, E Bresnitz, MD, New Jersey Dept of Health and Senior Svcs. R Nieman, MD, K Klemick, Abington Memorial Hospital, Abington, Pennsylvania. R Plotinsky, MD, EIS Officer, CDC.
Editorial Note: Considered in the context of recent high-morbidity, hospital-associated outbreaks in North America, Great Britain, and the Netherlands (5), these cases of severe CDAD disease in populations previously thought to be at low risk might further reflect the changing epidemiology of CDAD. Certain features of CDAD that have been uncommon in the past, such as close-contact transmission, high recurrence rate, young patient age, bloody diarrhea, and lack of antimicrobial exposure, might be changing.
C. difficile exotoxins A and B cause colonic dysfunction and cell death. The epidemic strain produces 16 times more toxin A and 23 times more toxin B compared with other common strains (5). The increased severity of epidemic CDAD might result from this level of toxin production; however, the actual role of tcdC deletions in increased toxin production has not been determined. C. difficile toxinotype 0 is the historical standard type; variant toxinotypes have previously accounted for <20% of U.S. hospital isolates (6). Although the role of this binary toxin in human disease is unknown, it was previously detected in only 6% of clinical isolates but now is found uniformly in the epidemic strain (6). The isolates recovered during this investigation were both variant toxinotypes and carried the gene for binary toxin; one also carried the same 18-bp deletion in tcdC as the epidemic strain.
Virulent strains, which cause more severe disease in populations at high risk, might also cause more frequent, severe disease in populations previously at low risk (e.g., otherwise healthy persons with little or no exposure to health-care settings or antimicrobial use). Although the minimum annual incidence cited in this report is similar to previous estimates in ambulatory populations (eight to 12 cases per 100,000 population), the CA-CDAD case definition more stringently excluded hospital-acquired CDAD (7,8). The estimated case rate per antimicrobial prescription is twice as high as the <1 case per 10,000 incidence cited in these earlier studies (7,8). Because reporting in this investigation was voluntary, the true incidence of community CDAD is probably higher. Because historic surveillance data are not available, determining whether CDAD rates in peripartum women are changing is not possible; however, the only available report suggests a low baseline incidence, with only three obstetric cases identified among 74,120 obstetrics and gynecology admissions to one North Carolina hospital during 1985-1995 (9).
The findings in this report are subject to at least two limitations. First, because the report describes a convenience sample, the results are subject to reporting and selection biases. Second, because this sample was collected in a limited geographic region, results might not be generalizable to other regions. Moreover, although a single national estimate for ambulatory prescribing rates was applied to this region, substantial variation in these rates might exist.
Further investigation into the scope of CA-CDAD acquisition and related risk factors is warranted. Nonetheless, the cases described in this report demonstrate the need for clinicians to consider the diagnosis of CDAD in patients with severe diarrhea even if the patients do not necessarily have traditional risk factors such as recent hospitalization or antimicrobial use. Patients should seek medical attention for diarrhea lasting longer than 3 days or accompanied by blood or high fever. The findings underscore the fact that antimicrobial exposure is not benign and that judicious antimicrobial use in all health-care settings should continue to be emphasized.
References
(1.) McDonald CL, Banerjee S, Jernigan DB. Increasing incidence of Clastridium difficile-associated disease in U.S. acute care hospitals, 1992-2001 [Abstract]. In: Proceedings of the 14th Annual Scientific Meeting of the Society for Healthcare Epidemiology of America, Philadelphia, PA; April 17-20, 2004.
(2.) McDonald LC, Killgore GE, Thompson A, et al. Emergence of an epidemic, toxin gene variant strain of Clastridium difficile responsible for outbreaks in the United States between 2000 and 2004. N Engl J Med 2005 (in press).
(3.) McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescriptions in ambulatory care settings, United States, 1992-2000. Emerg Infect Dis 2003;9:432-7.
(4.) Rupnik M, Avesani V, Janc M, Eichel-Streiber C, Delmee M. A novel toxinotyping scheme and correlation of toxinotypes with serogroups of Clostridium difficile. J Clin Microbiol 1998;36:2240-7.
(5.) Warny M, Pepin J, Fang A, et al. Increased toxins A and B production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet 2005;366:1079-84.
(6.) Geric B, Rupnik M, Gerding DN, Grabnar M, Johnson S. Distribution of Clostridium difficile variant toxinotypes and strains with binary toxin genes among clinical isolates in an American hospital. J Med Microbiol 2004;53:887-94.
(7.) Levy DG, Stergachis A, McFarland LV, et al. Antibiotics and Clostridium difficile diarrhea in the ambulatory care setting. Clin Ther 2000;22:91-102.
(8.) Hirschhorn L, Trnka Y, Onderdonk A, Lee M, Platt R. Epidemiology of community-acquired Clostridium difficile-associated diarrhea. J Infect Dis 1994;169:127-33.
(9.) James A, Katz V, Dotters D, Rogers R. Clostridium difficile infection in obstetric and gynecologic patients. South Med J 1997;90:889-92.
Reported by: E Chernak, MD, CC Johnson, MD, Philadelphia Dept of Public Health; A Weltman, MD, Pennsylvania Dept of Health. LC McDonald, MD, L Wiggs, G Killgore, DrPH, A Thompson, MSSc, Div of Healthcare Quality Promotion, National Center for Infectious Diseases; M LeMaile-Williams, MD, E Tan, MBBS, FM Lewis, MD, EIS officers, CDC.
COPYRIGHT 2005 U.S. Government Printing Office
COPYRIGHT 2005 Gale Group