Definition
Bronchitis is an inflammation of the air passages between the nose and the lungs, including the windpipe, or trachea, and the larger air tubes called bronchi that bring air into the lungs from the trachea. When bronchitis is mild and brief in duration, it is called acute. Chronic bronchitis is recurrent, has a prolonged course, and is often a sign of a serious underlying lung disease.
Description
Acute bronchitis
Bronchitis is an inflammation of the breathing airways accompanied by coughing and spitting up of phlegm. It can be caused by exposure to a cold or the flu, infection, or irritants. Although the symptoms of acute and chronic bronchitis are similar, their causes and treatments are different. Acute bronchitis is most common in winter. It usually follows an upper respiratory infection, and may be accompanied by a secondary bacterial infection. Acute bronchitis usually resolves within two weeks, although the cough may persist longer. Like any upper airway inflammatory process, acute bronchitis can increase a person's likelihood of developing pneumonia.
Anyone can get acute bronchitis, but infants, young children, and the elderly are more likely to come down with the disease. Smokers and people with heart or lung diseases are at a higher risk of developing acute bronchitis. Individuals exposed to chemical fumes or high levels of air pollution also have a greater chance of developing acute bronchitis.
Chronic bronchitis
Chronic bronchitis is one of a group of diseases that fall under the name chronic obstructive pulmonary disease (COPD). Other diseases in this category include emphysema and chronic asthmatic bronchitis. Chronic bronchitis is a major cause of disability and death in the United States. The American Lung Association estimates that about 14 million Americans suffer from the disease. Chronic bronchitis shows symptoms similar to acute bronchitis, but it recurs and is present for at least three months a year. Until recently, more men than women developed chronic bronchitis, but as the number of women who smoke has increased, so has their rate of chronic bronchitis. Because this disease progresses slowly, middle-aged and older people are more likely to be diagnosed with chronic bronchitis.
Causes & symptoms
Acute bronchitis
Acute bronchitis usually begins with the symptoms of a cold, such as a runny nose, sneezing, and dry cough. However, the cough soon becomes deep and painful. Coughing brings up a greenish yellow phlegm or sputum. These symptoms may be accompanied by a fever of up to 102°F (38.8°C). Wheezing after coughing is common. About 90% of acute bronchitis is caused by a bacterial infection.
In uncomplicated acute bronchitis, the fever and most other symptoms, except the cough, disappear after three to five days. Coughing may continue for several weeks. Acute bronchitis is often complicated by a bacterial infection, in which case the fever and a general feeling of illness persist.
Chronic bronchitis
Chronic bronchitis is caused by inhaling respiratory tract irritants; it may also be due to recurrent bouts of acute bronchitis. The most common cause, however, is the irritation of cigarette smoke. The cells that line the respiratory system contain fine, hair-like outgrowths called cilia. Normally, the cilia of many cells beat rhythmically to move mucus along the airways. When smoke or other irritants are inhaled or when there is irritation from repeated dry coughing, the cilia become paralyzed or snap off and the airways become inflamed, narrowed, and clogged. This leads to difficulty breathing and can progress to the life-threatening disease emphysema. A mild cough is usually the first visible sign of chronic bronchitis. Coughing brings up phlegm, and wheezing and shortness of breath may accompany the cough.
Diagnosis
General
Initial diagnosis of bronchitis is based on observing the patient's symptoms and health history. The physician will do chest examination with a stethoscope for specific sounds that indicate lung inflammation and airway narrowing. A sputum culture may be performed, particularly if the sputum is green or has blood in it, to determine whether a bacterial infection is present and to identify the disease-causing organism so that an appropriate antibiotic can be selected. Occasionally, in diagnosing a chronic lung disorder, the sample of sputum is collected using a procedure called a bronchoscopy.
Chronic bronchitis
A pulmonary function test is important in diagnosing chronic bronchitis and other variations of COPD. This test uses an instrument called a spirometer to measure the volume of air entering and leaving the lungs. The doctor may do a chest x ray, an electrocardiogram (ECG), and blood tests as well. Other tests may be used to measure how effectively oxygen and carbon dioxide are being exchanged in the lungs.
Treatment
The treatment of chronic bronchitis is complex and depends on the stage of chronic bronchitis and whether other health problems are present. Lifestyle changes, such as quitting smoking and avoiding secondhand smoke or polluted air, are an important first step. Controlled exercise performed on a regular basis is also important.
There are a multitude of botanical and herbal medicines that can be used to treat bronchitis. Examples from aromatherapy include essential oils of any of the following: benzoin, Styrax benzoin; camphor, Cinnamomum camphora; eucalyptus, Eucalyptus globulus; lavender, Lavandula officinalis; pine, Pinus sylvestris; sandalwood, Santalum album; or thyme, Thymus vulgaris. Any one or combination of these oils should be added to water and inhaled in a warm steam. They can also be dabbed on to a cloth, and the aroma can be breathed in deeply through the nose. A mixture of the essential oils of clove, Eugenia aromaticum; cinnamon, Cinnamomum zeylanicum; lemon balm , Melissa officianalis; and lavender, Lavandula officinalis, is reported to be particularly effective when taken as a steam inhalation.
Herbalists recommend taking a tea, syrup or tincture of any of the following: mullein, Verbascum thapsus; coltsfoot, Tussilago farfara; aniseed, Pimpinella anisum; hyssop, Hyssopus officinalis; elecampane, Inula helenium; and garlic, Allium sativum. The Chinese herb ephedra, also called ma huang or Ephedra sinica, may be recommended as long as heart disease or high blood pressure is not a problem. Ephedra is only used in herbal combinations and when coughing and wheezing are present. There are many remedies in traditional Chines medicine for coughing and phlegm.
Recommended homeopathic remedies include Aconite 6c, Kali bichromicum 6c, and Phosphorus 6c.
Acupuncture can be useful in preventing chronic bronchitis attacks and in resolving colds that lead to acute attacks.
For a mild case of acute bronchitis over-the-counter remedies of homeopathic medicine, traditional Chinese medicine , and Ayurveda are widely available and quite helpful. Practitioners of these disciplines can be very effective and should be consulted in dealing with more severe or chronic cases. Hydrotherapy and massage with tapping and cupping is also recommended in bronchitis to loosen mucus, improve breathing, and heighten the immune response to the condition.
The juice of a lemon squeezed into a cup of water should be consumed to clear out mucus. Hot, spicy foods can help open the air passages. These foods include garlic, onions, chili peppers, and horseradish, and should be consumed liberally.
Allopathic treatment
Acute bronchitis
When no secondary infection is present, acute bronchitis is treated in the same way as the common cold . Home care includes drinking plenty of fluids, resting, not smoking, increasing moisture in the air with a cool mist humidifier, and taking acetaminophen (Datril, Tylenol, Panadol) for fever and pain. Aspirin should not be given to children because of its association with seizures in children. Cough syrups are recommended to reduce coughing, soothe irritation, and increase expectoration of mucus.
It is important for mucus to be cleared from the lungs. The use of cough suppressants should be limited because when coughing is suppressed, the mucus accumulates in the plugged airways and may become a breeding ground for pneumonia bacteria. If the patient is coughing up phlegm, the cough should be allowed to continue to bring up mucus and irritants from the lungs. Cough medicines with expectorants may, therefore, be helpful. Expectorant cough medicines are used to thin the mucus in the lungs, making it easier to cough up and expel. People who are unsure about what type of medications are in over-the-counter cough syrups should ask their pharmacist for an explanation.
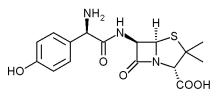
If a secondary bacterial infection is present, the infection is treated with an antibiotic. Patients need to take the entire amount of antibiotic prescribed. Tetracycline or ampicillin are often used to treat adults. Children under age eight are usually given amoxicillin (Amoxil, Pentamox, Sumox, Trimox), because tetracycline discolors permanent teeth that are still under the gums.
Chronic bronchitis
Drug therapy uses bronchodilators to relax the muscles of the bronchial tubes and allow increased airflow. They can be taken by mouth or inhaled using a nebulizer. Common bronchodilators include albuterol (Ventolin, Proventil, Apo-Salvent) and metaproterenol (Alupent, Orciprenaline, Metaprel, Dey-Dose). Anti-inflammatory medications are added to reduce swelling of the airway tissue. Corticosteroids, such as prednisone, can be taken orally or intravenously. Other steroids are inhaled. Medications are also given to reduce the quantity of mucus. As the disease progresses, the patient may need supplemental oxygen. A one-time pneumonia vaccination may also be recommended.
Expected results
When treated, acute bronchitis normally resolves in one to two weeks without complications, although a cough may continue for several more weeks. Unfortunately, there is no cure for chronic bronchitis, and the disease can often lead to or coexist with emphysema. On the whole, all forms of COPD are a leading cause of death.
Prevention
The best way to prevent bronchitis is not to begin smoking or to stop smoking. Smokers are 10 times more likely to die of COPD than non-smokers. Smokers who stop show improvement in lung function. Other preventative steps include avoiding chemical and environmental irritants, such as air pollution, and maintaining good overall health.
Supplementation with vitamins A, C, and E, zinc and bioflavonoids may also be helpful in preventing recurrence and secondary infections. Dairy products, sugar foods and eggs should be avoided, as they may increase the tendency to form mucus in the lungs.
Key Terms
- Bronchoscopy
- An examination of the lungs and airway passages using a flexible fiberoptic instrument.
- Emphysema
- A disease involving destruction of air sacs in the lungs, so that they do not take in oxygen easily and have the tendency to retain air within the lungs.
- Mucus
- The slippery secretion of the mucous membranes of the respiratory tract.
- Phlegm
- A thick secretion of mucus produced in response to irritation that may clog the airway passages.
- Sputum
- Mucus and other substances coughed up from the lungs.
- Trachea
- A cartilage tube in the area of the throat that carries air to the lungs.
Further Reading
For Your Information
Books
- The Burton Goldberg Group. Alternative Medicine: The Definitive Guide. Washington: Future Medicine Publishing, 1995.
- The Editors of Time-Life Books. The Medical Advisor: The Complete Guide to Alternative and Conventional Treatments. VA: Time-Life, Inc., 1996.
Periodicals
- Tiep, Brian L. "Disease Management of COPD with Pulmonary Rehabilitation." Chest (December 1997).
Organizations
- National Heart, Lung, and Blood Institute Information Center. P.O. Box 30105, Bethesda, MD 20824-0105.
- National Jewish Center for Immunology and Respiratory Medicine. 1400 Jackson Street, Denver, CO 80206.
Gale Encyclopedia of Alternative Medicine. Gale Group, 2001.