Abstract
Background: Lichen sclerosus remains an elusive disease with an uncertain relationship to morphea and scleroderma. The disorder has been difficult to treat, with no consistent and reproducible efficacious therapy. Recently, a beneficial effect of treatment with oral calcitriol (1-25 dihydroxyvitamin D3) in patients with scleroderma or morphea was described. This fact could be ascribed to the immunomodulatory effects of calcitriol observed in vitro and to inhibition of fibroblastic growth. Because of the success of calcitriol in localized scleroderma, we attempted this therapy in a patient with LS.
Observation: One patient with cutaneous generalized LS resistant to different therapeutics was treated with calcitriol in an oral daily dose of 0.5 mcg. After 6 months of treatment, the skin extensibility increased, and the lesions improved. The improvement persisted after discontinuation of therapy during a follow-up period of one year. The only side effect was hypercalciuria, which resolved with dose reduction.
Conclusion: Calcitriol has shown a beneficial effect in scleroderma and morphea during open studies. A case is reported of a patient with LS who had a dramatic response to calcitriol. Double blind, placebo-con trolled trials are needed to assess the therapeutic value of calcitriol in patients with LS.
Introduction
The controversy about the relationship between cutaneous lichen sclerosis (LS) and morphea began early and continues to this day. Although most recent reports classify LS as an entity of scleroderma, this remains a topic of research and debate. Despite the administration of several therapeutic regimens, no efficient therapy for LS has been described.
Recently, several cases of morphea and scleroderma have been treated with calcitriol (1-25 dihydroxyvitamin D3) with beneficial effects. Calcitriol is the biologically active form of vitamin D and acts on target cells such as fibroblasts and lympbocytes. This observation prompted an exploration of the possible use of the hormone in the treatment of LS.
Case Report
A 53 year old man developed symptomless hypopigmented and atrophic plaques on the upper part of the chest, present since May 1995 (Figure 1). In 1997, they expanded to the back, the shoulders, and the upper part of the legs and arms (Figure 2). Lesions were hypopigmented, atrophic in the center, erythematous, and crumbling on the border. The individual lesions were small and of ivory color, with shiny papules and macules. The surface displayed prominent dilated pilosebaceous or sweat duct orifices. There was also a hemorrhagic and bullous plaque on the sacrum. The oral and genital mucosa aspects were normal. Physical examination revealed induration and sclerosis which led to discomfort, especially on the arm areas (Figure 3). This clinical aspect was in conformance with the diagnosis of cutaneous lichen sclerosis.
[FIGURES 1-3 OMITTED]
Histology confirmed the diagnosis, showing orthohyperkeratosis with keratotic plugging, epidermal atrophy with degeneration of basal cells, edema, and homogenization of the collagen in the upper dermis, as well as inflammatory infiltrate in the mid-dermis (Figure 4).
[FIGURE 4 OMITTED]
Multiple therapies have been tried without success for these conditions (topical corticosteroids, Piascledine, Amoxicillin, etc.). To prevent the skin lesion spreading to the arms and legs, we proposed a treatment trial with calcitriol (Rocaltrol[TM], from Roche), and obtained the patient's informed consent prior to beginning the trial. This was particularly important in this case due to the possible side effects, as well as the innovative aspects of the treatment, which revolves around the as-yet unknown relationship between morphea and LS, and the beneficial effects of calcitriol in morphea and scleroderma.
In August 1997, we began calcitriol therapy with an oral daily dose of 0.5 mcg. After a 4 to 6 month period, the patient felt better and noticed improvement in his skin appearance. After one year of treatment, hypopigmented lesions were lessened (Figure 5) with a corresponding decrease in infiltration (Figure 6). The bullae and hemorrhagic sacrum plaque disappeared (Figure 7) and the treatment was discontinued in September of 1998. From then through now, no new lesions have appeared and to date there is no sign of recurrence.
[FIGURES 5-7 OMITTED]
Overall, the patient responded very well to the calcitriol treatment except for a transient hypercalciuria in April of 1998 that responded immediately to a temporary (one month) interruption of the treatment.
An anatomicopathological examination in January of 1999 presented a cicatrical aspect with a decrease of hyperkeratosis, dermis infiltration, and hyalinized dermic superficial band (Figure 8).
[FIGURE 8 OMITTED]
Discussion
Lichen sclerosis was described clinically by Hallopeau (1) in 1889 and histologically by Darier in 1892 (2). It is an inflammatory disease of unknown cause and insufficiently characterized pathogenesis (3). LS can affect all age groups (4) and while most patients described in the literature are Caucasian, the majority of whom are women, the female-to-male ratio provides a wide range which goes from 10:1 (5) to about 1:1 (6).
There are more cases of purely genital involvement than purely non-genital. There is also a well founded evidence of a link between LS and auto-immune diseases (7). Extragenital LS is most common on the neck and shoulders, is generally asymptomatic, and pruritis may occasionally occur. Less common forms of LS include infraorbital LS, (8) scarring alopecia (9), and involvement of palms and soles (10). Borda et al. proposed a vitiligoid variant in which pigmentary changes exist without plaques and papules (11).
Typically, the eruptions begin as white, polygonal papules that coalesce into plaques. There are comedo-like plugs or evenly spaced dells in the surface of the plaque that correspond to appendageal ostia. The plugs and dells may disappear with time, leaving a smooth, porcelain-white plaque. Early LS may have a vesicular component (12).
Bullous LS (13), often accompanied by intralesional hemorrhage, may be localized or generalized. Palpation shows superficial induration and atrophy. Lesions may have a tendency for spontaneous regression. LS demonstrates an isomorphic response, also described as the Koebner phenomenon (14).
Histologically, a compact orthohyperkeratosis recovers a significantly thinned epidermis. Vacuolar degeneration of the basal layer is common, especially in earlier lesions; when extensive, it may cause bullae formation. Follicular occlusion by a cornified plug may lead to atrophy and disappearance of appendageal structures (15). The papillary dermis becomes homogenized and edematous soon after onset, and hyalinized and sclerotic over time. Grouped substances composed of neutral and acidic mucopolysaccharides increasingly appear in the edematous papillary dermis (16). Elastin may be modified so as to strain poorly with orcein (17). Other ultrastructural studies have shown both degeneration of subepidermal elastin and changes in collagen (18). Melanocytes are reduced. A mononuclear lichenoid infiltrate may be dense and extensive or patchy in older lesions.
The controversy about the relationship between LS and scleroderma began early and continues to this day. These two conditions have clinical and histological features in common, including association with autoimmune diseases and in the varying phases of graft versus host disease (19). Many authors have described coexistent LS and morphea (20); morphea and LS coexisting in the same biopsy specimen has like-wise been described (21). General investigators have reported transition from LS to morphea and vice-versa (22). Borda et al. (23) and more recently Peterson et al. (24) view LS as a scleroderma of papillary dermis, and classify LS in morphea plaques. Others view LS and morphea as manifestations of the same disease, with morphea having a greater association with systemic disease (25). The proposal that LS, systemic scleroderma, morphea, and borrelial diseases are the same entity has received much recent attention (26).
However, investigators believe there are enough clinical and histologic differences between LS and morphea to argue they are distinct and that coexistent lesions are coincidental (27). For example, morphea does not have the immunoreactant deposition at the dermoepidermal junction and papillary dermis found in LS (28). Different lectin patterns have been reported (29), and the loss of elastic fibers characteristic of LS is not found in morphea (30). Changes in the dermal ground substance and dermoepidermal junction are distinct (31). Collagen biosynthesis is increased in morphea and decreased in LS (32).
Patterson and Ackermann tried to distinguish LS and morphea histologically in 24 patients, and concluded that features favoring LS were vacuolization at the dermo-epidermal junction and a lichenoid infiltration of the papillary dermis, while morphea showed dermal sclerosis and an infiltrate in the reticular dermis (33). Griffith and Presley demonstrated different reactions of fibroblasts to paraaminobenzoates with respect to morphea, LS, and normal skin, opining that LS and morphea could be respective initial anomalies of GAG and collagen (34).
Their physiopathology is unknown and multifactorial with various components such as genetic, hormonal, autoimmune, and infective influences.
There is no established treatment for LS, and most often topical corticosteroids are first utilized. Several treatments have been tried without effectiveness: antimalarials (35), oral corticotherapy (36), antispirochetal antibiotherapy (37), oral retinoids (38), potassium paraaminobenzoate (39), cryotherapy, and PUVA therapy, to list a few. Various therapies for morphea have likewise been used with limited success (40).
Open prospective studies involving oral calcitriol (Rocaltrol[TM]) were led by Humbert et al. and showed beneficial effects in 14 cases of systemic scleroderma and 7 morphea (41-48). In these studies the oral daily dose varied from 0.5 to 1.75 mcg. After an average of one year of treatment, the mobility of the joints increased (judged by maximal oral opening and palmar flexion index); there was increased skin torsion (as measured using a torsional device); and the skin thickness showed improved intrinsic extensibility (the extensibility of a given volume of skin as measured with a 15 MHz Echometer thickness gauge). These improvements remained after a one year discontinuation of therapy. No side effects were observed with the exception of hypercalciuria and hypercalcemia which can be easily managed by a reduction in dosage.
Ballmer, Weber et al. reported 10 morphea, 1 generalized scleroderma, and 1 LS patient treated with calcitriol in a dose of 0.75 to 1.75 mcg, over a 4 to 12 month period. Their patient response was only effective in 25% of the cases (49).
An open prospective study assessed the effect of oral calcitriol for 3 generalized morphea patients receiving an oral daily dose of 0.5-0.75 microgram. After the treatment period of 4-6 months, significant clinical improvement was observed, without side effects. The follow-up period was one year (50).
Another study investigated the use of calcitriol in 27 patients (7 systemic scleroderma and 20 morphea) with 0.75 microgram/day for 9 months. Calcitriol was not more effective than placebo, but no fair conclusions regarding efficacy can be drawn because of the small group of patients.
In children, one open study assessed Calcitriol for 7 cases of linear scleroderma (0.75 meg per day; 3 months). The results indicate that Calcitriol was effective in 5 patients (clinical scoring (52). This therapeutic possibility must be defined (53).
Topical Calcipotriol ointment was also evaluated in open study with good results for morphea and linear scleroderma, alone or in association with low dose ultraviolet A1 phototherapy (54,55).
It is the opinion of the authors that double-blind, placebo-controlled trials are needed to assess the therapeutic value of calcitriol. Based on the relation between LS and morphea as well as the efficacy of calcitriol in morphea, it become logical to propose this treatment in LS. Our case is the second one treated with calcitriol but it is the first one with substantial positive results; spontaneous regression is improbable because the lesions were stable or in progression for a few years.
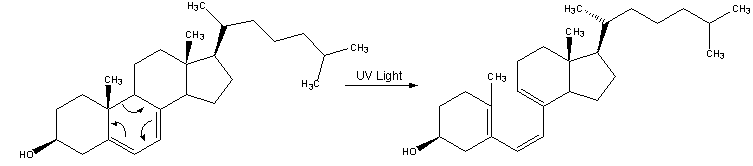
Calcitriol (1-25 OH2 D3) is the biologically active metabolite of vitamin D3, the latter being synthesized in the skin from 7-dehydrocholesterol after UV irradiation. Vitamin D3 is hydroxylated in the liver and kidney into 1-25 OH2 D3.
The skin is both the site for synthesis of vitamin D3 and a target organ for its active metabolite as it was shown keratinocytes and fibroblasts possess nuclear receptors for 1-25 OH2 D3 (56).
The relevant actions of 1-25 OH2 D3 in scleroderma can be categorized in various types: immunomodulatory effects on lymphocyte and monocyte / macrophage function (inducing several cytokines released from fibroblasts, keratinocytes and immune cells) (57); inhibition of fibroblast proliferation; or direct effects on the collagen gene expression and regulation, as suggested for other steroid hormones. These actions could both explain the effectiveness of calcitriol in LS treatment. The development of less hypercalcemic analogs might open a new therapeutic area for vitamin D3.
Conclusion
Based on the relationship between LS and morphea as well as the efficacy of calcitriol in some cases of morphea, this open-label trial suggests a possible positive effect of oral calcitriol in patients with LS. This is the first case where this treatment has been proved through effective results. If this is confirmed by future controlled trials, it could offer an attractive alternative therapy with the additional benefit that the only side effects are hypercalcemia and hypercalciuria. Such side effects being controlled easily by a reduction in dosage.
Bibliography
(1.) Hallopeau H. Lichen plan sclereux. Ann Derm Syph 1889; 20:447-9.
(2.) Darier J. Lichen plan sclereux. Ann Derm Syph 1892; 23:833-7.
(3.) Jeffrey J, Meffert MC, Brian M et al. Lichen sclerosis. J Am Acad Dermatol 1995; 32/3:393-416.
(4.) Aaronson LD, Baler G, Schiff BL. Lichen Sclerosis et atrophicus occurring in childhood. Arch Dermatol 1962; 85:746-7. (Wallace HJ. Lichen Sclerosis et atrophicus. Trans St. Johns Hosp Derm Soc 1971; 57:9-30.)
(5.) Brownstein MH. Lichen sclerosis et atrophicus. Arch Dermatol 1973; 108:713-23.
(6.) Garcia Bravo B, Sanchez-Pedreno P, Rodriguez-Pichardo A et al. Lichen sclerosis et atrophicus. J Am Acad Dermatol 1988; 19: 482-5.
(7.) Meyrick Thomas RH, Ridley CM, Mc Gibbon DH, Black MM. Lichen sclerosis and autoimmunity--a study of 350 women. Br J Dermatol 1988; 108:41-6.
(8.) Klenk-Pfeifer E. Lichen sclerosis et atrophicus facei bei 12 jahrigem Madchen. Z Hautkr 1974; 49:841.
(9.) Foulds IS. Lichen Sclerosis et Atrophicus of the scalp. Br J Dermatol 1980; 103:197-200.
(10.) Purres J, Krull EA. Lichen sclerosis et atrophicus involving the palms. Arch Dermatol 1971; 104:68-9.
(11.) Borda JM, Abulafia J, Jaimovich L. Syndrome of circumscribed sclero-atrophies. Derm Ibero Lat Am 1968; 3:179-202.
(12.) Barclay DL, Macey HB, Reed RJ. Lichen sclerosis et atrophicus of the vulva in children. Obstet Gynecol 1966; 27: 637-42.
(13.) Di Silverio A, Serri F. Generalized bullous and haemorrhagic lichen sclerosis et atrophicus. Br J Dermatol 1975; 93:215-7.
(14.) Meffert JJ, Grimwood RR. Lichen sclerosis et atrophicus appearing in an old burn scar. J Am Acad Dermatol 1994; 31:671-3.
(15.) Shelley WB, Levy EJ. Histologic observations on the human apocrine sweat gland in health and disease. J Invest Dermatol 1955; 25:249-63.
(16.) Stoughton R, Wells G. A histochemical study on polysaccharides in normal and diseased skin. J Invest Dermatol 1950; 14:37-51.
(17.) Mann PR, Cowan MA. Ultrastructural changes in four cases of lichen sclerosis et atrophicus. Br J Dermatol 1973; 89:223-31.
(18.) Daroczy J, Torok E. Electronmicroscopy of lichen sclerosis et atrophicus. Trans St Johns Hosp Dermatol Soc 1974; 60:183-7.
(19.) Ridley CM. Lichen Sclerosis: a review. Eur J Dermatol 1994; 4:99-105.
(20.) Miller JL. Scleroderma en bande and lichen sclerosis et atrophicus. Arch Dermatol 1987; 123:485-8.
(21.) Natarajan S, Green ST. Generalized morphea, lichen sclerosis et atrophicus, and primary biliary cirrhosis. Clin Exp Dermatol 1986; 11:304-8.
(22.) Gitto J, Santa Cruz DJ, Bauer EA et al. Morphea and lichen sclerosis et atrophicus. J Am Acad Dermatol 1980; 271-9.
(23.) Borda JM, Abulafia J, Jaimovich L. Syndrome of circumscribed sclero-atrophies. Derm Ibero Lat Am 1968; 3:179-202.
(24.) Peterson LS, Nelson AM, Su WPD. Classification of morphea. Mayo Clin Proc 1995; 5:5-13.
(25.) Lewis GM. Scleroderma: Lichen scerosus et atrophicus? Arch Dermatol 1961; 84:146-8.
(26.) Abele DC, Anders KH. The many faces and phases of borreliosis. J Am Acad Dermatol 1990; 23:401-10.
(27.) Senear FE. Lichen sclerosis et atrophicus. Arch Dermatol Syph 1948; 58:540.
(28.) Chorzelski T, Jablonska S. Coexistence of lupus erythematosus and scleroderma in light of immunopathological investigations. Acta Derm Venereol 1970; 50:81-5.
(29.) Shono S, Imura M, Ota Met al. Lichen sclerosis et atrophicus, morphea, and coexistence of both diseases. Arch Dermatol 1991; 127:1352-6.
(30.) Winer LH. Elastic fibers in unusual dermatoses. Arch Dermatol 1955; 71:338-48.
(31.) Stoughton R, Wells G. A histochemical study on polysaccarides in normal and diseased skin. J Invest Dermatol 1950; 14:37-51.
(32.) Panizzon R, Vuorio T, Bruckner-Tuderman L. Collagen biosynthesis and type I and type III procollagen mRNA in lichen sclerosis et atrophicus. Arch Dermatol Res 1990; 282:480-3.
(33.) Patterson JAK, Ackerman AN. Lichen sclerosis et atrophicus is not related to morphea. A clinical and histological study of 24 patients in whom both conditions were reputed to be present simultaneously. Am J Dermatopathol 1984; 6:323-5.
(34.) Griffiths MR, Priestley GC. A comparison of morphea and lichen sclerosis et atrophicus in vitro: the effects of para amino benzoate on skin fibroblasts. Acta Derm Venereol 1992; 72:15-18.
(35.) Scully JP. Lichen sclerosis et atrophicus. Arch Dermatol 1958; 77:763.
(36.) Connelly MG, Winkelmann RK. Coexistence of lichen sclerosis. morphea and lichen planus. J Am Acad Dermatol 1985; 12:844-51
(37.) Buechner SA, Winkelmann RK, Lautenschlager S et al. Localized scleroderma associated with Borrelia Burgdorferi infection. J Am Acad Dermatol 1993; 29:190-6.
(38.) Bousema MT, Romppanen U, Geiger JM et al. Acitretin in the treatment of severe lichen sclerosis et atrophicus of the vulva: a double bind, placebo-controlled study. J Am Acad Dermatol 1994; 30:225-31.
(39.) Coskey RJ. Dermatologic therapy: December 1983 through November 1984. J Am Acad Dermatol 1985; 12:1045-71.
(40.) Sapadin AN, Fleischmajer R. Treatment of Scleroderma. Arch Dermatol 2002; 138: 99-105.
(41.) Humbert P, Aubin F, Dupont JL et al. Oral calcitriol as a new therapeutic agent in localized and systemic scleroderma. Arch Dermatol 1995; 131(7): 850-51.
(42.) Hulshof MM, Pavel S, Breedveld FC et al. Oral calcitriol as a new therapeutic modality for generalized morphea. Arch Dermatol 1994; 130(10): 1290-93.
(43.) Humbert P, Delaporte E, Dupont JL et al. Treatment of localized scleroderma with oral 1-25 dihydroxyvitamin D3. Eur J Dermatol 1994; 4(1): 21-23.
(44.) Humbert P, Dupont JL, Agache P et al. Treatment of scleroderma with oral 1-25 dihydroxyvitamin D3: Evaluation of skin involvement using non-invasive techniques. Results of an open prospective trial. Acta Derm Venereol 1993; 73(6): 449-451.
(45.) Delaporte E, Humbert P, Dupont JL et al. Sclerodermie en plaques: efficacite remarquable du 1-25 dihydroxycholecalciferol. Rev Med Interne 1993; 14(6):498.
(46.) Matsuoka LY, Dannenberg MJ, Worstman J et al. Cutaneous vitamin D3 formation in progressive systemic sclerosis. J Rheumatol 1991; 18(8):1196-98.
(47.) Dupont JL, Humbert P, Rochefort A et al. Treatment of systemic sclerosis and localized scleroderma with 1-25 dihydroxycholecalciferol Rev Med Interne 1991; 12:S26.
(48.) Humbert P, Dupont J, Rochefort A et al. Localized scleroderma, response to 1-25 dihydroxyvitamin D3. Clin Exp Dermatol 1990; 15(5):396-98.
(49.) Ballmer-Weber BK, Berchtold B. Calcitriol: an effective therapy for the treatment of morphea? Dermatology 1996; 193(2):162.
(50.) Caca-Bilijanovska NG, Vlckova-Laskosta MT, Dervendi DV, Pesic NP, Kaskoski DS. Treatment of generalized morphea with oral 1,25-dihydroxyvitamin D3. Adv Exp Med Biol 1999; 455:299-304.
(51.) Hulshof MM, Bouwes bavinck JN, Bergman W, Masclee AA et al. Double bind, placebo controlled study of oral calcitriol for the treatment of localized and systemic scleroderma. J Am Acad Dermatol 2000; 43: 1017-23.
(52.) Elst EE, Van Suijlekom Smit LWA, Oranje AP. Treatment of Linear Sceroderma with oral 1,25. Dihydroxyvitamin D3 (Calcitriol) in seven children. Pediatric Dermatology 1999; 16:53-58.
(53.) Bodemer C, Amoric JC, Hamel Teillac D, De Prost Y. Localized scleroderma in children and a therapeutic trial using calcitriol: a therapeutic possibility to define. Ann Dermatol Venereol 1999; 126:725-726.
(54.) Kreuter A, Gambichler T, Avermaete A, Jansen T, Hoffmann M, Hoffmann K et al. Combined treatment with calcipotriol ointment and low dose ultraviolet A1 phototherapy in childhood morphea. Pediatric Dermatol 2001; 18:241-45.
(55.) Cunningham BB, Landells ID, Langman C, Sailer DE, Pallet AS. Topical calcipotriene for morphea/linear scleroderma. J Am Acad Dermatol 1998; 39:211-215.
(56.) Boelsma E, Pavel S, Ponec M. Effects of Calcitriol on fibroblasts derived from skin of scleroderma patients. Dermatology 1995; 191/3:226-233
(57.) Lemire J. 1,25 Dihydroxyvitamin D3: a hormone with immunomodulatory properties. Z Rheumatol 2000; 59: 24-27.
ADDRESS FOR CORRESPONDENCE:
Luc Thomas
Hotel Dieu Hospital
1 place de l' Hopital
69288 Lyon cedex 02, France
E-mail: luc.thomas@chu-lyon.fr
S RONGER MD, AM VIALLARD MD, F MEUNIER-MURE MD, B CHOUVET MD, B BALME MD, L THOMAS MD
DEPARTMENT OF DERMATOLOGY, HOTEL DIEU HOSPITAL, LYON, FRANCE.
COPYRIGHT 2003 Journal of Drugs in Dermatology
COPYRIGHT 2003 Gale Group