Here we report the case of a patient who presented with acute cardiac tamponade due to drug-induced systemic lupus erythematosus (SLE). The patient had been treated for a seizure disorder with carbamazepine, a drug that has previously been demonstrated to cause SLE-like syndromes. Further serologic analysis demonstrated the likelihood of drug-induced SLE in this patient, with the rare presentation of cardiac tamponade.
(CHEST 2000; 117:597-598)
Key words: carbamazepine; systemic lupus erythematosus; tamponade
Abbreviations: dsDNA = double-stranded DNA; SLE = systemic lupus erythematosus
Carbamazepine is a medication commonly employed for the treatment of seizure disorders, chronic, pain syndromes, trigeminal neuralgia, and psychiatric illness. Although carbamazepine is usually well tolerated by most people, the potential side effects of therapy can vary from mild symptoms to severe systemic reactions. Common side effects include drowsiness, ataxia, diplopia, nausea, and vomiting. More serious adverse reactions include drug-induced systemic lupus erythematosus (SLE), pseudolymphoma syndrome, aplastic anemia, agranulocytosis, and hypersensitivity.[1] Here we describe the case of a patient who developed cardiac tamponade as a severe manifestation due to carbamazepine-induced SLE-like syndrome.
CASE REPORT
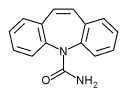
A 45-year-old white man with a medical history of a generalized seizure disorder whose anticonvulsant therapy had been changed from phenytoin to carbamazepine 8 months prior to this admission presented to the emergency department with the chief complaint of chest discomfort and dyspnea. Although his symptoms had been present for several days, a sudden worsening of his pain and new onset shortness of breath prompted his seeking medical attention. His initial vital signs were BP of 90/60 mm Hg; heart rate, 114 beats/min; respiratory rate, 26 to 30 breaths/min; and temperature, 36.5 [degrees] C. In addition, the patient had a pulsus paradoxus of 20 mm Hg. On physical examination, the patient's chest was clear to auscultation bilaterally, and cardiac auscultation revealed distant heart sounds, with S1, S2, and S3 gallop present. Pertinent laboratory data included a carbamazepine level of 7.8 [micro]g/mL (therapeutic range, 4 to 10 [micro]g/mL); BUN, 18 mg/dL; creatinine, 0.7 mg/dL; total bilirubin, 0.9 mg/dL; aspartate aminotransaminase (serum glutamic oxalacetic transaminase), 13 IU/L; alanine aminotransaminase (serum glutamic pyruvate transaminase), 9 IU/L; albumin, 2.8 g/dL; creatinine phosphokinase, 53 IU/L; WBC count, 10.5 x [10.sup.3]/[micro]L with a normal differential; hemoglobin 12.1 g/dL; and hematocrit, 35.5%. A chest radiograph revealed a "waterbottle" cardiac silhouette (Fig 1), a right-sided pleural effusion without evidence of pulmonary infiltrate. The ECG demonstrated sinus tachycardia and low voltages without electrical alternans. An emergent echocardiogram showed a large circumferential pericardial effusion, persistent inversion of the right atrium, and right ventricular diastolic collapse, all consistent with tamponade physiology.
[Figure 1 ILLUSTRATION OMITTED]
An urgent therapeutic pericardiocentesis was performed with approximately 850 mL of fluid removed. The patient immediately began to feel relief of pain in addition to improved breathing. A follow-up echocardiogram demonstrated substantial reduction in the pericardial effusion with the elimination of tamponade physiology. The patient was subsequently transferred from the emergency department to the coronary care unit for further observation. Routine pericardial fluid studies showed a pH of 7.28; RBC count, 6,215 cells/[micro]L; WBC count, 3,030 cells/[micro]L (neutrophils 25%, lymphocytes 72%, monocytes 3%); protein, 5,013 mg/dL; glucose, 72 mg/dL; and lactate dehydrogenase, 238 IU/L. Further laboratory studies including bacterial, mycobacterial, viral, fungal, and cytologic studies indicated no evidence of infection or malignancy. Blood serologic studies showed antinuclear antibodies positive (1:320 dilutions), anti-double-stranded-DNA (dsDNA) negative, antihistone antibodies positive, and Smith autoantibody negative, all highly suggestive of a drug-induced SLE syndrome. Serum studies for echovirus, Coxsackie-virus, Lyme disease, and HIV were all negative. Complement levels of C3, C4, and CH50 were all within normal limits. The patient was subsequently switched to phenobarbital for antiseizure therapy and was discharged with an uneventful hospital stay.
DISCUSSION
Several major criteria have been used to make the diagnosis of drug-induced SLE. These criteria include the following: (1) the development of SLE-like symptoms during drug therapy; (2) the cessation of the SLE-like symptoms within weeks of discontinuing the drug therapy; (3) no clinical or laboratory evidence of SLE prior to beginning the drug therapy; and (4) the presence of antihistone antibodies with the absence of high titers of anti-dsDNA antibodies.[2,3] The presence of these criteria is highly suggestive of drug-induced SLE, and serologic studies are often the most helpful clinically. Antihistone antibodies are present in only 50% of patients with idiopathic SLE, but are present in 95% of patients with drug-induced SLE; while anti-dsDNA antibodies are usually absent in drug-induced SLE and present in 85% of patients with idiopathic SLE.[4,5] Antinuclear antibodies are not helpful in making this distinction, since they are present in [is greater than] 85% of patients afflicted with either idiopathic or drug-induced SLE.[4,5]
In addition to laboratory criteria, drug-induced SLE has characteristic clinical manifestations that distinguish populations of patients with drug-induced SLE from those with idiopathic SLE. Utilizing the 80 eases of drug induced SLE-like syndrome reported to Ciba-Geigy from 1963 to 1990 in countries from all over the world, several clinical findings can be noted.[6] Cutaneous manifestations, as with idiopathic SLE, represented the most frequent finding, accounting for 34% of reported cases. Unfortunately, cutaneous manifestations are also present in [is greater than] 80% of patients with idiopathic SLE. Renal and CNS manifestations were extremely rare in drug induced-SLE while being common in idiopathic SLE. Pericarditis and pericardial effusions accounted for 5% of cases.
Subsequent follow up after 1 year demonstrated the return of this patient's serology to negative antinuclear antibodies, anti-dsDNA, and antihistone antibodies, without recurrence of pericardial effusion. The development of drug-induced SLE is a well-described adverse reaction to carbamazepine therapy. Both the clinical and laboratory findings supporting the diagnosis of drug-induced SLE are present in this patient. Although the development of cardiac tamponade is a rare complication of drug-induced SLE, it has been noted with other medications.[7] In patients receiving carbamazepine who develop chest pain and dyspnea, it is imperative to consider the possibility of drug induced cardiac tamponade/pericarditis, since its prompt recognition and treatment can be lifesaving.
REFERENCES
[1] Hardman JG, Limbird LE, Molinoff PB, et al. Goodman & Gilman's pharmacological basis of therapeutics. 9th ed. New York, NY: McGraw-Hill, 1996
[2] Cohen MG, Prowse MV. Drug-induced rheumatic syndromes: diagnosis, clinical features and management. Med Toxicol Adverse Drug Exp 1989; 4:199-218
[3] Meyer O, Cyna L, Haim T, et al. IgG Antibodies to histones: diagnostic value in rheumatoid arthritis, progressive systemic sclerosis, and spontaneous or drug induced systemic lupus erythematosus. Rev Rhum 1984; 51:303-310
[4] Epstein A, Barland P. The diagnostic value of anti-histone antibodies in drug-induced lupus erythematosus. Arthritis Rheum 1985; 518:158-162
[5] Frazier MJ, Tan EM. Antibodies to histones in drug-induced and idiopathic lupus erythematosus. J Clin Invest 1978; 62:60-567
[6] Jain KK. Systemic lupus erythematous (SLE)-like syndromes associated with carbamazepine therapy. Drug Saf 1991; 6:350-360
[7] Mohindra SK, Udeani GO, Abrahamson D. Cardiac tamponade associated with drug induced systemic lupus erythematosus. Crit Care Med 1989; 17:961-962
(*) From the Renal Electrolyte and Hypertension Division (Dr. Verma), University of Pennsylvania School of Medicine, Philadelphia, PA; and the Department of Medicine (Drs. Yunis, Lekos, and Crausman), Brown University School of Medicine Providence, RI. Manuscript received May 21, 1999; revision accepted August 26, 1999.
Correspondence to: Sunil P. Verma, MD, MPH, University of Pennsylvania School of Medicine, Renal Electrolyte and Hypertension Division, 700 Clinical Research Building, 415 Curie Blvd, Philadelphia, PA 19104-6144; e-mail: sunilv@att.net
COPYRIGHT 2000 American College of Chest Physicians
COPYRIGHT 2000 Gale Group