INTRODUCTION: Pulmonary nodules are a typical radiographic finding in patients with pulmonary Langerhans' cell histiocytosis (PLCH). Langerhans' cell histiocytosis (LCH) is a rare disorder that is characterized by an uncontrolled accumulation of Langerhans' cells in various organs. In addition to pulmonary complications, there does appear to be an association with an increased risk of developing malignant neoplasms. We present a case of a patient with PLCH with typical radiographic findings who subsequently developed metastatic bronchogenic carcinoma originating in an area with nodules presumed to be secondary to PLCH.
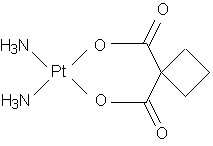
CASE PRESENTATION: A 32 year old white male was initially diagnosed with LCH at age 4. He had several episodes of recurrent bony involvement, which were treated with a combination of surgery, radiation therapy, and chemotherapy. At age 30, the patient presented with dyspnea. Pulmonary involvement of his LCH was suspected, with typical CT findings of nodules and upper lobe predominant cystic lesions. The patient also had an obstructive pattern on pulmonary function studies. He entered into a smoking cessation program and was able to reduce his use but was unable to quit. His pulmonary symptoms and lung function did stabilize without further interventions. He presented two years later with headaches and increasing dyspnea. A brain MRI was performed that revealed multiple ring enhancing lesions. A chest x-ray and CT were obtained that showed a 3x4 cm left lower lobe mass. Tissue obtained by CT-guided fine needle aspiration showed a well differentiated adenocarcinoma consistent with a primary lung cancer. The patient began brain irradiation and palliative chemotherapy with taxol and carboplatin.
DISCUSSIONS: Pulmonary nodules are typical findings in PLCH that have been associated with early disease. Over time the nodules may cavitate and result in thin-walled cavities that are often described in PLCH. These nodules, however, may represent a diagnostic dilemma. Though in most cases these nodules will represent the usual radiographic findings of PLCH, malignant lesions cannot be entirely excluded. There is a clear association with LCH and malignancy. Lymphoma and leukemia are most frequently seen, but solid organ malignancy, particularly lung cancer, has been reported. It appears that between 5 and 14% of patients with pulmonary Langerhans' cell histiocytosis will be diagnosed with lung cancer. (1,2,3) There appears to be an increased tendency for malignancy in all forms of LCH. Cumulative tobacco exposure and previous chemotherapy and radiation therapy confer additional risk of developing cancer. These factors suggest that more aggressive cancer screening may be warranted in patients with LCH. This case is noteworthy because the lung cancer occurred in an area of a nodule seen on the initial CT scan. Though pulmonary nodules are commonly seen in radiology studies in PLCH, this case suggests that these nodules may need to be followed closely by serial CT scans and may require histologic confirmation. The overall approach to appropriate surveillance for lung cancer in these patients needs further elucidation.
CONCLUSION: Lung cancer screening is an essential component to the long-term management of patients with PLCH.
REFERENCES:
(1) Sadoun D, Vaylet F, Valeyre D, et al. Bronchogenic Carcinoma in Patients with Pulmonary Histiocytosis X. Chest 1992; 101:1610-1613
(2) Tomashefski JF, Khiyami A, Kleinerman J. Neoplasms Associated with Pulmonary Eosinophilic Granuloma. Archives of Pathology & Laboratory Medicine 1991; 115:499-506
(3) Vassallo R, Ryu JH, Schroeder DR, et al. Clinical Outcomes of Pulmonary Langerhans'-Cell Histiocytosis in Adults. New England Journal of Medicine 2002; 346:484-490
DISCLOSURE: Bradley Harrold, None.
Bradley R. Harrold MD * Maria R. Lucarelli MD The Ohio State University, Columbus, OH
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group