What types of drugs are found in transdermal preparations?
* Many doctors choose to combine two or more types of medications in the transdermal preparation.
* Adjunct pain relievers: These medications are not anesthetics but reduce pain by blocking transmission of a pain signal to the brain. These include antidepressants such as amitriptyline and many other types of drugs.
* Anesthetics: Anesthetics relieve pain, and when used transdermally can be applied directly to a specific problem area. The most commonly used transdermal pain relievers are benzocaine, lidocaine, and tetracaine.
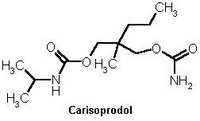
* Muscle relaxants: A muscle relaxant reduces the contractility of the muscle by blocking the transmission of nerve impulses. Common prescription examples include carisoprodol and cyclobenzaprine.
* Nonsteroidal anti-inflammatory drugs (NSAIDs): While NSAIDs act quickly and can relieve mild pain, their real therapeutic purpose is to minimize inflammation (swelling, redness) in the joints and tissues, which can affect movement in some cases. Examples of common NSAIDs are aspirin and ibuprofen.
Which specific ingredients are used?
Compounding pharmacists have far more options than commercial medicines provide, since commercial medicines are available only in fixed doses and in certain forms. (Many pain medications are available commercially only in oral form.) Transdermal pain formulations can include a number of drugs, including but not limited to those listed here. Some of these can be taken in oral form, but transdermal preparations usually cause fewer, if any, unwanted side effects.
* Amitriptyline
* Cyclobenzaprine
* Dexamethasone
* Gabapentin
* Ketamine
* Ketoprofen
* Lidocaine
* Piroxicam
What conditions are transdermal medications used for?
While there are many specific diagnoses for which transdermal pain medication may be ideal, the following are some of the most common:
* Arthritis
* Localized or acute injury
* Muscle and joint pain
* Nerve pain
Am I a candidate for transdermal pain medication?
Transdermal [trans = through; dermal = the skin] preparations are suitable for most people, and may be particularly useful in those who have an unusually sensitive digestive tract or difficulty swallowing. Transdermal pain medications may not be suitable for broken or raw skin or on very large surface areas. Patients who have allergies or sensitivities to any of the prescription components should not use these medications, and those who are allergic to soy may not be able to use preparations containing certain ingredients such as Pluronic lecithin organogel (PLO). As with any prescription, you should tell your Healthcare provider and pharmacist about all other prescription and overthe-counter medications and supplements you use so that they can screen for possible drug interactions. Talk to your doctor if you are pregnant or nursing a baby. Your pharmacist will advise you about possible side effects.
How are transdermal pain medications usually applied?
Your Healthcare provider will advise you how to apply the medication and for how long. This type of treatment typically is applied in the amount prescribed to the affected area(s) up to three times daily and rubbed in well. Some patients may gradually taper the amount they use as pain lessens. Application of a thin film onto clean, diy skin is generally all that is required to produce the needed effect.
How are transdermal medications dispensed?
Dispensing and packaging vaiy from pharmacy to pharmacy. The medication may come in a tube, a jar, or a syringe. In some cases, a jar with a special adapter is used, and a syringe will be dispensed along with it for easy application. Be sure to ask your pharmacist for a demonstration of how to measure your dose.
Copyright International Journal of Pharmaceutical Compounding Sep/Oct 2005
Provided by ProQuest Information and Learning Company. All rights Reserved