Nearly one-third of all women who responded to a Fall 2003 online survey at the NWHRC's Web site, www.healthywomen.org, said they were taking vitamins, over-the-counter medications and/or herbal remedies to manage their menopausal-related symptoms mostly because they felt they would be safer than hormonal therapies. (11) They'-re not alone.
**********
After the Women's Health Initiative results were announced in 2002, thousands of women stopped taking hormones and began looking for other options, many for the most trouble some of their menopausal symptoms: hot flashes. Among the alternatives:
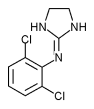
* Prescription medications. Studies on the antidepressants fluoxetine (Prozac), paroxetine (Paxil) and venlafaxine (Effexor); the anti-seizure medication gabapentin (Neurontin); and the anti-hypertensives clonidine (Catapres) and methyldopa (Aldoril), find these medications significantly reduce the frequency and severity of hot flashes in postmenopausal women. However, antidepressants have well-established side effects affecting sexual response, which is often a problem for menopausal women to begin with, notes Philip Sarrel, MD, an emeritus professor at Yale Medical School.
* Oral contraceptives. Women approaching menopause are often prescribed oral contraceptives to help with heavy bleeding and other menstrual irregularities. One three-year study of a triphasic oral contraceptive in 200 perimenopausal women found it significantly reduced women's hot flashes when compared to placebo. It also reduced bone-mass loss, helped with vaginal dryness and sexual responsiveness, and prevented or improved mood, concentration, insomnia and loss of concentration, among other menopause-related symptoms. (14) Oral contraceptives contain higher doses of estrogen and progesterone than most hormone therapies on the market.
* Herbal and alternative remedies. Leading the pack of herbal remedies touted for hot flash relief is black cohosh, with some randomized, controlled studies showing improvement in mild hot flashes. But there are no long-term data on the safety of black cohosh, a plant estrogen, in postmenopausal women, and some researchers worry it could increase the risk of certain reproductive cancers. (19) Furthermore, since it is thought to act similarly to estrogen in some ways in the body, it is usually not recommended for women for whom estrogen is not recommended.
Other herbal remedies, including isoflavones, red clover, evening primrose oil, ginseng, licorice, or dong quai, show little effect on menopausal symptoms. (15) Though a handful of controlled studies conducted on acupuncture for menopausal symptoms also found no effect, one study did. (15,21) There is also some evidence that hypnosis may help reduce the frequency, duration and severity of hot flashes. (16)
If you're considering herbal remedies or other supplements, keep in mind that the U.S. Food and Drug Administration doesn't oversee the production of supplements, nor require manufacturers to prove their products are effective, as they do with prescription or even over-the-counter drugs.
* Vitamins. The first well-controlled trial of vitamin E, conducted in 1953, found it was no more effective than a placebo in relieving menopausal symptoms, but a trial in women with breast cancer conducted in 1998 found it did relieve hot flashes. Plus, vitamin E is believed to have healthful benefits for your heart, and at doses of 800 IU, presents no danger. (17,18)
* Progesterone cream. Whether or not this product works on hot flashes isn't certain. With only two randomized clinical trials conducted on the use of progesterone cream on hot flashes, one showed a small improvement at 20 mg/day, but the other trial, which used 32 mg/day, showed no improvement over placebo. According to a position statement by the North American Menopause Society in the March/April 2003 journal Menopause, progesterone cream or gel preparations available by prescription or over-the-counter may not protect the uterine lining from the effects of unopposed estrogen. These products should not be used for this purpose until more is known from long-term clinical trials about ideal therapeutic doses. (20)
COPYRIGHT 2004 National Women's Health Resource Center
COPYRIGHT 2004 Gale Group