Ms. P is a 72-year-old widowed retired librarian who presents at your office seeking advice. Since her retirement last year, she has been complaining of a depressed mood. Ms. P has no past psychiatric history, but her mother suffered from recurrent bouts of moderately severe depression. An assessment of her symptoms shows that she is experiencing depressed mood, some anhedonia, decreased energy, and poor sleep. She has a history of atrial fibrillation, but otherwise is in good health. She takes coumadin 4 mg po qhs and a multivitamin daily. She tells you that she began taking St. John's Wort (Hypericum perforatum) from a nearby health food store after a friend had recommended it about one week ago. She is taking 300 mg tid and would like to know if it is "safe" for her to use. What should you advise?
Herbals history
Herbs and plants have been used to treat various medical and psychiatric conditions for many centuries, dating back to the early uses of belladonna as an aesthetic agent and lavender as an anesthetic. More recently, they have transmogrified into the realm of 'herbal supplements,' a designation causing many patients not to consider them serious medications. Currently, supplements are taken to treat psychiatric complaints, such as anxiety, dementia, depression, and insomnia. Supplements and herbs, however, do not require the same rigorous approval as do prescription medications. The Food and Drug Administration (FDA) only requires that supplement labels state, "These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease." Perhaps a more rigorous standardized evaluation of these supplements by the FDA is warranted.
Common belief holds that herbs cannot harm you because they are not 'foreign,' like manufactured or chemical medications. This is a misplaced notion, for St. John's Wort is no more natural for one's body than is fluoxetine. Nearly 16% to 18% of adults in the United States regularly use herbal supplements. (1) Sales of herbal products in the United States doubled to $16 billion between 1994 and 20002 and 23% of those >50 years use herbal products. (3) There are about 15 million adults at risk of experiencing adverse interactions from prescription medication, herbs, and/or vitamin supplements, including nearly 3 million adults age 65 or older. (4,5)
Given the misconception that herbal supplements have benign side effects, it is not surprising that one study found that almost two-thirds of patients do not tell their physicians that they are taking supplements. (6,7) Therefore it is imperative to ask each patient to tell his health care provider every medication (prescribed and over-the-counter) as well as every vitamin and supplement that they are taking or have been taking recently. The physician should warn patients that such supplements may interfere with prescribed medications or that they may have side effects. As we shall review, it is important to consider the range of interactions and adverse events that can result from herbal supplements (Table 1). Wong et al (7) provided an excellent review of herbal supplements, usage, and effects.
Herb-drug interactions
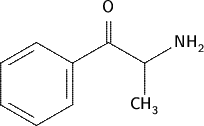
Many herb-drug interactions can be explained through inhibition or inducement of P450 microenzymes. (8) For example, St. John's Wort is a potent inducer of 3A4 and an inhibitor of several others (1A2, 2C9, 2C19, 2D6, and 3A4). (9) St. John's Wort is particularly worrisome given the interactions with anticoagulants, digoxin, antidepressants, and protease inhibitors. (10,11) In one case series, St. John's Wort was reported to cause mania. (12)
Lack of regulation of plant products could mean that patients may not even be consuming the plant listed on the product label. For example, preparations of ginseng may contain substantially more or less ginseng than labeled as well as varying quantities of other, unrelated, but active substances. (13) Thus, if there is a question of a herb/drug interaction, it is important to stress to the patient the necessity of discontinuing all herbal supplements.
Herb and plant misuse is yet another overlooked issue (Table 2). This can be more important in certain cultures than others. Because many commonly abused plants are not regulated by government agencies, they are more freely available even if they are not native to one's country. Some plants, such as betelnut, may leave telltale traces of their use, such as staining of the teeth and gums or oral ulcerations, which may become cancerous. Others offer no such signs.
Conclusion
You advise Ms. P that St. John's Wort may interfere with her levels of coumadin and arrange for her to have her blood drawn for INR and PT levels, which were therapeutic. You advise her to discontinue the St. John's Wort and arrange for Ms. P to undergo weekly group and individual cognitive behavioral therapy. Two months later she reports that she is doing well.
References
(1.) Keller KB, Lemberg L. Herbal or complementary medicine: Fact or fiction? Am J Crit Care 2001; 10(6):438-43.
(2.) Blendon RJ, et al. Americans' views on the use and regulation of dietary supplements. Arch Intern Med 2001; 161(6):805-10.
(3.) Eskin SB. Dietary supplements and older consumers. In AARP Public Policy Institute, Data Digest 2001: Washington, DC:1-8.
(4.) Eisenberg DM, et al. Trends in alternative medicine in the United States, 1990-1997: Results of a follow-up national survey. J Am Med Assoc 1998; 280(18):1569-75.
(5.) Studdert DM, et al. Medical malpractice implications of alternative medicine. J Am Med Assoc 1998; 280(18):1610-5.
(6.) Eisenberg DM. Advising patients who seek alternative medical therapies. Ann Intern Med 1997; 127(1):61-9.
(7.) Wong AH, Smith M, Boon HS. Herbal remedies in psychiatric practice. Arch Gen Psychiatry 1998; 55(11): 1033-44.
(8.) Zhou S, Chan E, Pan SQ, Huang M, Lee EJ. Pharmacokinetic interactions of drugs with St John's wort. J Psychopharmacol 2004; 18(2):262-76.
(9.) Zhou S, Gao Y, Jiang W, Huang M, Xu A, Paxton JW. Interactions of herbs with cytochrome P450. Drug Metab Rev 2003; 35(1):35-98.
(10.) Brazier NC, Levine MA. Drug-herb interaction among commonly used conventional medicines: A compendium for health care professionals. Am J Ther 2003; 10(3):163-9.
(11.) Williamson EM. Drug interactions between herbal and prescription medicines. Drug Saf 2003; 26(15):1075-92.
(12.) Moses EL, Mallinger AG. St. John's Wort: Three cases of possible mania induction. J Clin Psychopharmacol 2000; 20(1):115-7.
(13.) Harkey MR, Henderson GL, Gershwin ME, Stern JS, Hackman RM. Variability in commercial ginseng products: An analysis of 25 preparations. Am J Clin Nutr 2001; 73(6):1101-6.
(14.) Desai AK, Grossberg GT. Herbals and botanicals in geriatric psychiatry. Am J Geriatr Psychiatry 2003; 11(5): 498-506.
Dr. Hoblyn is associate director of inpatient geropsychiatry, Palo Alto Veterans Affairs Health Care System, California, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, California.
Dr. Brooks is director of inpatient psychiatry, Palo Alto Veterans Affairs Health Care System, and assistant professor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine.
Disclosure: The authors have no real or apparent conflicts of interest with the information presented here.
COPYRIGHT 2005 Advanstar Communications, Inc.
COPYRIGHT 2005 Gale Group