More than five million cases of otitis media are diagnosed every year in the U.S. A commonly treated health problem, this inflammation of the middle ear is often treated with antibiotics. Dr. J. Owen Hendley, from the University of Virginia, reviewed 100 studies and discovered that antibiotics help only one out of eight children with ear infections.
The New England Journal of Medicine published a study regarding the use of antibiotics versus the use of a placebo. It revealed that during a one-week period, 94 percent of the recipients using antibiotics for ear infections resolved, while 84 percent of the placebo-controlled recipients resolved during the same time period.
Little, Gould, et al.,1 presented the downside of the use of antibiotics by stating: "The bacteria, which cause ear infections, learn quickly to be resistant to antibiotics. At some point we're going to run out of drugs to treat the problem. Antibiotics resistance is a huge problem in this country. The practice of treating eight children to help one who needs antibiotics just makes it worse."
"Wait and watch" is sage advice.
A previous study by Little, Gould, et al., compared immediate versus delayed usage of antibiotics, showing that for most children, the benefit with immediate antibiotics was only marginal, with no significant difference in pain or distress. It should be noted, however, that the medical conclusion was that immediate antibiotic prescriptions provided symptomatic benefit mainly after 24 hours, when symptoms were already resolving. For children who are not very ill systemically, the "wait-and-watch" approach seems clinically feasible.
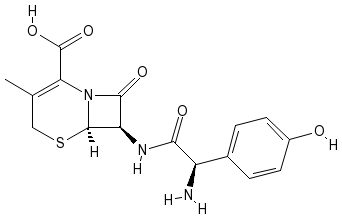
Parents, beware of the side-effects and contraindications to the usage of antibiotics! Side-effects to drugs such as amoxicillin, Augmentin or ampicillin include diarrhea, hives and yeast infections. Children with a previous allergy to these drugs should not take them. Also, the cephalosporin antibiotics cefadroxil and cephalexin may present numerous side-effects, such as upset stomach; nausea; vomiting; depressed white blood cell (WBC) counts; anemia; rashes; and inhibited blood clotting. Contraindications to these may include an allergy to the drug; a blood clotting disorder or history of bleeding problems; phenylketonuria; and stomach or intestinal diseases, especially colitis.
Ciprofloxacin side-effects are upset stomach; nausea; vomiting; loss of appetite; diarrhea; headache; sleep disturbance; increased risk of tendonitis; dizziness; mood changes; a depressed WBC count; anemia; rashes; and sun sensitivity. Its contraindications include children susceptible to seizures or with central nervous system disorders. Erythromycin side-effects are upset stomach and rash, and it is contraindicated if the child is vomiting or has nausea.
The growing problem of childhood asthma brings a new host of drug exposure to the young child.
Did you know that childhood asthma causes more school absences than any other single pediatric disorder?
Between 1982 and 1992, there was a 56-percent increase in newly diagnosed asthma cases in the United States, and in the past decade the numbers have continued to be staggering.
Common drugs for treatment of asthma:
* Bronchodilator side-effects include dizziness; flushed face; headache; increased heart rate; and nervousness. Contraindication includes allergy to the medicine, or a child with heart or blood vessel diseases.
* Leukoriene modifiers (Singulair, Accolate): Side-effects include headache; nasal congestion; nausea; diarrhea; abdominal pain; weakness; dizziness; muscle aches; and fever.
* Inhaled steroids (AeroBid, Flovent, etc.) can cause oral yeast infections and may be risky in cases of serious infection, such as pneumonia.
* Oral steroids (prednisone, etc) may suppress the immune system and cause fluid retention, insomnia and increased appetite. Contraindications are the same as those of inhaled steroids.
* Theophylline (Aerolate, Brokodyl, etc.): Side-effects include nervousness; headache; irritability; increased heart rate; nausea; and diarrhea. Possible long-term use may be linked to learning disabilities.
The doctor of chiropractic often is viewed as a family doctor to many families in his or her practice. Our role is not to take a child off of medication, but rather to inform parents that other possible alternative options (even outside of chiropractic) exist in the less severe cases and that possibly, for the more severely symptomatic child, co-management care is a viable option.
A vast majority of parents unknowingly give their child medications without properly being warned of the potential side-effects and contraindications to these chemicals.
One step you can take is to review these drugs with parents from the PDR or another resource. Parents should have all the information at hand to make an educated decision to the health-care choices and risks when it comes to their children.
Reference
1. Anrig C. The antibiotic dilemma. Dynamic Chiropractic Oct. 2002;20 (21):18,32-33.
Claudia Anrig, DC. Dr. Anrig's articles, a "Talk Back" forum and a brief biography of the author are available online at www.chiroweb.com/columnist/anrig.
Claudia Anrig, DC
Clovis, California
Editor's note: Part one of this article appeared in the June 16, 2003 issue. A printable version of Dr. Anrig's article is available online at www.chiroweb.com/columnist/anrig. You may also leave a comment or ask a question at her "Talk Back" forum at the same location.
Copyright Dynamic Chiropractic Sep 1, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved