BACKGROUND. Topical antimicrobials have been considered for treatment of secondarily infected wounds because of the potential for reduced risk of adverse effects and greater patient convenience. We compared mupirocin cream with oral cephalexin in the treatment of wounds such as small lacerations, abrasions, or sutured wounds.
METHODS. In 2 identical randomized double-blind studies, 706 patients with secondarily infected wounds (small lacerations, abrasions, or sutured wounds) received either mupirocin cream topically 3 times daily or cephalexin orally 4 times daily for 10 days.
RESULTS. Clinical success at follow-up was equivalent in the two groups: 95.1% and 95.3% in the mupirocin cream and the cephalexin groups, respectively (95% confidence interval [CI], -4.0% to 3.6%; P = .89). The intention-to-treat success rate was 83% in both groups. Bacteriologic success at follow-up was also comparable: 96.9% in the mupirocin cream and 98.9% in the cephalexin groups (95% CI, -6.0% to 2.0%; P = .22). The occurrence of adverse experiences related to study treatment was similar for the 2 groups, with fewer patients in the mupirocin cream group reporting diarrhea (1.1 % vs 2.3% for cephalexin).
CONCLUSIONS. Mupirocin cream applied topically 3 times daily is as effective as oral cephalexin given 4 times daily for the treatment of secondarily infected wounds and was well tolerated.
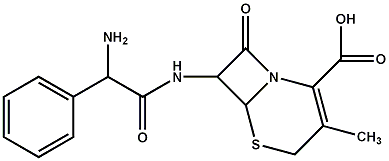
KEY WORDS. Mupirocin; cephalexin; wound infection; abrasion; laceration. (J Fam Pract 1998; 47:429-433)
Most patients with secondarily infected wounds are treated with systemic antimicrobials that pose a risk of adverse reactions, including hypersensitivity reactions and gastrointestinal disturbances. Topical antimicrobials may offer reduced risk of adverse effects and greater patient convenience. Mupirocin calcium cream is a new formulation of mupirocin that contains 20 mg mupirocin calcium in each gram of an emulsion base. It has antibacterial activity against the majority of common wound pathogens, including aerobic gram-positive cocci: Staphylococcus aureus (including methicillin-resistant strains), Staphylococcus epidermidis, Streptococcus pyogenes, and beta-hemolytic streptococci.[1] The cream formulation was developed because it is preferred over the ointment formulation for treatment of conditions when the lesion should be kept "dry." Also, polyethylene glycol in the ointment formulation poses a slight risk of nephrotoxicity if there is absorption through denuded epithelium. The ointment formulation of mupirocin was shown to be superior to ampicillin, erythromycin, and cloxacillin for treatment of primary and secondary skin infections.[2,3,4]
The objective of this study was to compare the efficacy, safety, and tolerability of the mupirocin calcium cream formulation with oral cephalexin in the treatment of patients with secondarily infected wounds (such as small lacerations, abrasions, or sutured wounds). This is the first report of this formulation for infected wounds.
METHODS
STUDY DESIGN
This report includes the combined results from 2 multicenter studies, with a total of 53 participating centers in the United States conducted concurrently under identical protocols between August 1994 and June 1996. Two studies were required for approval by the Food and Drug Administration. Treatment was randomized and administered in a double-blinded, double-dummy manner to 2 parallel groups. The protocol was approved by the investigational review board at each institution, and patients (or parent or legal guardian) provided written informed consent.
PATIENTS
Patients of any age presenting with secondarily infected wounds (such as a small laceration, abrasion, or sutured wound) who could be treated with mupirocin calcium cream or oral cephalexin were enrolled. Most patients were seen in physician offices or clinics. All patients had to have a Skin Infection Rating Scale (SIRS) total score of at least 8.[5] The SIRS score is a severity index based on a 0 (absent) to 6 (severe) scale, with a possible maximum score of 42. The parameters evaluated were: exudate/pus, crusting, erythema/inflammation, tissue warmth, tissue edema, itching, and pain. Investigators were instructed in the use of the scale, and it was applied by a single investigator at each site to assure continuity. Also, patients had to have a positive Wright stain for white blood cells from wound exudate. A laceration or sutured wound could not have exceeded 10 cm in length with surrounding erythema no more than 2 cm from the edge of the lesion. Abrasions could not exceed 100 [cm.sup.2] in total area with surrounding erythema no more than 2 cm from the edge of the abrasion.
Patients were excluded if they (1) demonstrated a previous hypersensitivity reaction to penicillins, cephalosporins, other beta-lactam antimicrobials, or mupirocin; (2) had a bacterial skin infection that, because of depth or severity, could not be appropriately treated with a topical antibiotic (eg, cellulitis, abscess, ulcer, furunculosis); (3) had a secondarily infected animal, human, or insect bite or a puncture wound; (4) had systemic signs or symptoms of infection; (5) required surgical intervention for treatment of the infection; (6) received a systemic antibacterial or steroid, or had applied any topical therapeutic agent directly to the wound or used soap containing an antibacterial agent within 24 hours before entering the study; (7) had a serious underlying disease as judged by the investigator; (8) were pregnant, breast-feeding, or planning a pregnancy during the study; (9) had used an investigational drug within 30 days before entering the study; or (10) had been previously enrolled in this protocol.
ANTIMICROBIAL TREATMENT
Patients were randomly assigned (1:1 ratio, by computer) to receive either topical mupirocin calcium cream (2% mupirocin, SmithKline Beecham) or oral cephalexin (Keflex, Dista Products Co.) for 10 days. All patients received a placebo of the alternative dosage form. Mupirocin (or placebo cream, the emulsion base alone) was applied to cover the entire wound 3 times daily. Patients weighing more than 40 kg received cephalexin 250-mg capsules (or identical-appearing placebo capsules) 4 times daily. Patients weighing less than or equal to 40 kg received cephalexin suspension (or placebo suspension) 4 times daffy at a dosage adjusted for body weight (25 mg per kg of body weight per day). Patients were instructed to apply and gently rub the cream into the entire area with a sterile gauze sponge 3 times dally. A wound dressing could be used at the discretion of the investigator.
An assessment of compliance was performed, using patient diary cards, to ensure that patients received a minimum of 80% and a maximum of 120% of the prescribed medication doses. Pill and tube counts were also performed but were not the primary compliance measure.
EVALUATIONS
Forty-eight hours before beginning study medication, a Wright stain of wound exudate was performed by the investigator, and the SIRS score was determined. Bacteriologic specimens were obtained by lesion swabs and transported to SmithKline Beecham Clinical Laboratories (Van Nuys, Calif) for culture according to standard aerobic and anaerobic techniques as appropriate.
Patients were evaluated 3 to 5 days after the start of treatment ("on-therapy evaluation"), then 2 to 3 days after completion of therapy ("end-of-therapy evaluation"). Patients returned for follow-up clinical and bacteriologic evaluation 7 to 12 days after the end of treatment.
The primary end point was clinical response ("persistent clinical success," "clinical recurrence," or "unable to determine") which was recorded at the follow-up visit (7 to 12 days post-therapy). Persistent clinical success was defined as complete resolution or sustained improvement of signs and symptoms of infection. No exudate or pus could be present in the patient's wound, and no additional antibiotics were required for the treatment to be considered a persistent clinical success. Clinical recurrence was defined as reappearance or worsening of signs and symptoms of infection that required additional antibiotic therapy. Unable to determine was defined as the inability to make a valid assessment of clinical outcome. Results determined as failures at any point after 3 days of treatment were also considered failures at follow-up.
Bacteriologic response was determined at the follow-up visit and was assessed to be "persistent presumed eradication" if the symptomatic response was a success and a culture was not clinically indicated; "reinfection" if the pretherapy pathogen was eradicated but one or more new pathogens appeared during the follow-up period; "relapse" if the initial pathogen was eliminated during therapy but reemerged during the follow-up period; or "unable to determine" if bacteriologic evaluation could not be made. Patients were evaluated for bacteriologic efficacy if a pretherapy pathogen had been isolated and they were clinically evaluable.
Safety was determined for all randomized patients by interview at each visit. All adverse experiences were judged by the investigator to be not related, possibly related, or related to the study drug.
To assess patient acceptance of the 2 methods of treatment, a survey of all patients was conducted at the end-of-therapy visit. Two of the survey questions were "Do you prefer oral or topical therapy?" and "Was the cream easy to apply?"
DATA ANALYSIS
Each study was designed to enroll at least 150 patients per treatment (300 patients total) to determine with 90% power (beta = .10) that the lower confidence limit of the two-sided 95% CI (alpha = .05) of the difference in the clinical success rates between the 2 treatment groups was not below -10%, assuming that the clinical response rate in the 2 groups was 93%.
Continuous data were analyzed by t test, whereas categorical data were analyzed with the chi-square test. The equivalence of the 2 treatment groups was also assessed by determining the two-tailed 95% CIs of the difference in the proportions of patients with clinical and bacteriologic successes. The treatment groups were considered equally effective if the lower 95% confidence limit was not below -10%. Data were analyzed for the population that completed the study according to protocol, as well as the intention-to-treat population.
RESULTS
The 53 investigational sites were randomly assigned to either of the 2 studies. As a consequence, the 2 studies enrolled very similar populations. The results between the studies were consistent for clinical and bacteriologic efficacy as well as for safety.
Seven hundred six patients were randomized to receive study medication: 357 to receive mupirocin cream and 349 to receive cephalexin (Table 1). A total of 630 patients (89%) completed all 3 visits, and 478 (68%) were considered evaluable for clinical efficacy at the follow-up visit. Individual centers completed from 1 to 57 patients. Seventy-six patients were withdrawn because of adverse experiences, lack of efficacy, deviation from the protocol, or being lost to follow-up (Table 1).
TABLE 1
Patient Data for Those Randomized to Mupirocin Cream Topically or Cephalexin Orally (N = 760)
SD denotes standard deviation.
Of the evaluable patients, 155 had a small laceration (32%), 90 had a sutured wound infection (19%), 153 had an abrasion (32%), and 80 (17%) had other types of infected wounds (such as infected scratches, infected pierced body parts, and infected biopsy sites). Compliance with the antibiotic regimen ([is greater than] 80% and [is less than] 120% of doses taken) was similar for the 2 groups (92% and 93%, for mupirocin cream and cephalexin, respectively). Compliance for each route of administration was similar irrespective of the route of administration for the active treatment. There was no difference between the 2 treatment groups with respect to the SIRS score at the preliminary visit (P = .34), at the on-therapy visit (P = .35) and at the follow-up visit (P = .45).
CLINICAL RESPONSE
Analysis of the 2 studies combined, as well as each study independently, demonstrated statistical equivalence between the treatment groups. The clinical response at the follow-up visit was similar for the 2 treatment groups with success rates of 95% in both the mupirocin cream group and the cephalexin group (95% CI, -4.04% to 3.64%, P = .89) (Table 2). Twelve patients in the mupirocin group and 11 in the cephalexin group had treatment failures. Clinical failures occurred in patients with a variety of wound types (small lacerations, abrasions, and sutured wounds) and sites (hands, arms, legs, feet, face, neck, and trunk). Clinical response at the end-of-therapy visit (a secondary outcome measure) was similar between groups, 95.6% for the mupirocin cream group and 95.7% for the cephalexin group (95% CI, -3.59 to 3.39, P = .85).
TABLE 2
Summary of Clinical and Bacteriologic Responses for Evaluate and Intention-to-treat Populations (N = 478)
The 2 regimens were similar when assessed by intention-to-treat analysis of 706 patients. Clinical success at the end-of-therapy visit was achieved in 296 of 357 patients (83%) who received the mupirocin cream regimen and in 289 of 349 (83%) who received oral cephalexin (95% CI, -5.5 to 5.7, P = .77).
There was no significant effect of SIRS score on clinical response at follow-up (P = .13).
BACTERIOLOGIC RESPONSE
The pattern of organisms isolated was similar for the 2 treatment groups (Table 3). The most common isolate was Staphylococcus aureus (41% of isolates) followed by group A Streptococcus (7% of isolates).
TABLE 3
Pretherapy Pathogens isolated from >1% of Mupirocin-Treated Patients (Bacteriologic per Protocol Population at Follow-Up)
(*) Total pathogens = 136; total patients with at least 1 pretherapy pathogen = 98.
([dagger]) Total pathogens = 148; total patients with at least 1 pretherapy pathogen = 92.
([double dagger]) Total pathogens = 284: total patients with at least 1 pretherapy pathogen = 190.
Bacteriologic success was achieved in 97% of the patients who received mupirocin cream and 99% of patients who received cephalexin (95%, CI, -6.0% - 2.0%, P = .22) (Table 2). Superinfecting pathogens appeared in 3 patients (4 pathogens) in the mupirocin cream group and 1 patient (3 pathogens) in the cephalexin group. In the mupirocin cream group one isolate each of Aeromonas caviae, Ochrobium anthoropi, Pseudomonas aeruginosa, and Serratia liquifaciens and in the cephalexin group one isolate each of Enterobacter cloacae, S aureus, and group B Streptococcus appeared as superinfecting pathogens.
ADVERSE EXPERIENCES
Sixty of 706 patients (8.5%) reported 70 adverse experiences related or possibly related to the study medication (27 of 357 patients in the mupirocin group [7.6%] and 33 of 349 patients in the cephalexin group, [9.5%]; P = .42 between groups). The most frequently reported related or possibly related adverse experiences in both treatment groups were headache, diarrhea, and nausea, reported by 2.0%, 1.1%, and 1.1%, respectively, of patients in the mupirocin calcium cream group and by 1.1%, 2.3%, and 1.1%, respectively, of patients in the cephalexin group. No adverse experiences related or possibly related to study medication were severe in intensity. Ten patients in the mupirocin group (2.8%) and 7 in the cephalexin group (2.0%) were withdrawn because of adverse experiences. Adverse experiences believed related or possibly related to study medication that led to patient withdrawal were abdominal pain, nausea, earache, secondary wound infection, dermatitis, and rash in the mupirocin group and anorexia, diarrhea (3 patients), and urticaria in the cephalexin group.
PATIENT ACCEPTANCE
Of the patients completing the end of treatment survey, 484 (72%) preferred topical therapy and 181 (27%) preferred oral therapy. Six hundred sixty-four patients (99%) answered that the cream was easy to apply. Reponses were similar for patients in each of the treatment groups separately.
DISCUSSION
These large, multicenter studies demonstrated that topical antibiotic treatment with mupirocin cream is as effective as systemic treatment with oral cephalexin for secondarily infected wounds. Both agents resulted in a greater than 90% success rate for evaluable patients (83% for intention-to-treat patients). Therefore, the choice of regimen can be based on the potential for adverse effects and patient convenience. In these studies almost all patients felt that the topical treatment was easy to apply. Two thirds of patients indicated that they preferred topical treatment over oral treatment.
Mupirocin has demonstrated activity against many multidrug-resistant staphylococci, including methicillin. resistant strains.[1,6] In these studies, resistance to the antimicrobial regimens was not detected from pretherapy isolates, and did not develop during therapy. Resistance of staphylococci to mupirocin has been reported in clinical isolates, usually with long-term (more than 10 days) use.[7] In one multicenter survey of 8220 isolates of staphylococci in the United Kingdom, .3% of S aureus and 3% of coagulase negative staphylococci were mupirocin resistant.[8] A study of 1309 S aureus isolates from hospital personnel in the United States demonstrated a 1% resistance rate.[9] Intermittent or short-term use of mupirocin is unlikely to present a high risk of development of resistance.
One difficulty in conducting trials of secondarily infected wounds is determination of whether a wound is infected. In this trial we relied on the subjective assessment of the investigator; however, objective criteria were also considered. To be enrolled, the patient had to have a minimum SIRS score and the presence of white blood cells in the wound by Wright's stain. We believe these criteria have improved the validity of the data generated.
Cost of treatment is also an important issue when selecting antimicrobial regimens. Because cephalexin is available in generic form, its acquisition cost may be lower than mupirocin cream; however, this must be weighed against the cost of resistance with the systemic agent.
CONCLUSIONS
Mupirocin cream is as effective as oral cephalexin for treatment of secondarily infected wounds (such as small lacerations, abrasions, and sutured wounds). Patients tolerated both regimens well, preferring the topical regimen; this is important when considering patient compliance. The results of these studies are most appropriately applied to patients with similar types of infected wounds who are likely to respond to treatment with a topical agent.
ACKNOWLEDGMENTS
These studies were funded by a grant to each center from SmithKline Beecham Pharmaceuticals.
REFERENCES
[1.] Ward A, Campoli-Richards DM. Mupirocin: a review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs 1986; 32:425-44.
[2.] Welsh O, Saenz C. Topical mupirocin compared with oral ampicillin in the treatment of primary and secondary skin infections. Curr Ther Res 1987; 41:114-20.
[3.] Dux PH, Fields L, Pollock D. 2% topical mupirocin versus systemic erythromycin and cloxacillin in primary and secondary skin infections. Curt Ther Res 1986; 40:933-40.
[4.] Gratton D. Topical mupirocin versus oral erythromycin in the treatment of primary and secondary skin infections. Int J Dermatol 1987; 26:472-3.
[5.] Brenneman DL. Use of mupirocin ointment in the treatment of secondarily infected dermatoses. J Am Acad Dermatol 1990; 22:886-92.
[6.] Layton MC, Patterson JE. Mupirocin resistance among consecutive isolates of oxacillin-resistant and borderline oxacillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 1994; 38:1664-7.
[7.] Chatfield CA, O'Neill WA, Cooke RPD, et al. Mupirocin-resistant staphylococcus aureus in a specialist school population. J Hosp Infect 1994; 26:273-8.
[8.] Cookson BD, Lacey RW, Noble WC, et al. Mupirocin-resistant staphylococcus aureus. Lancet 1990; 335:1095-6.
[9.] Gu JW, Briones F, Fang W, et al. Susceptibility of 1,309 nasal isolates of staphylococcus aureus from hospital personnel in the United States to 21 antibiotics. 91st General Meeting of the American Society for Microbiology, Dallas, Tex. 1991:A-97. (Abstract.)
Submitted, revised, August 25, 1998.
From Dermatology Associates (S.J.K.), Kanuai Medical Clinic (L.J.E.), R/D Clinical Research Inc. (G.W.B.), Centre for Health Care (M.A.D.), and SmithKline Beecham Pharmaceuticals (W.D.B., M.A.C.). Requests for reprints should be addressed to Michael A. Cupo, SmithKline Beecham Pharmaceuticals, 1250 S Collegeville Rd, PO Boa: 5089, Collegeville, PA 19426-0989.
COPYRIGHT 1998 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group