Source: Zamrini E, McGwin G, Roseman JM. The association between statin use and Alzheimer's disease. Neuroepidemiology 2004; 23(1-2):94-8.
Statin use for up to 12 months has been shown to reduce the risk of Alzheimer's disease (AD) by 39% in patients age >50 who have cardiovascular disease or risk factors, according to a study by researchers at the University of Alabama.
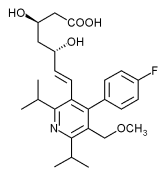
In the nested case-control study, investigators evaluated patients from the Veterans Affairs Medical Center in Birmingham, Alabama, to determine whether statin drugs (eg, atorvastatin, cerivastatin) normally used for patients with hyperlipemic disorders, have any effect on patients with AD; adjustments were made for comorbid medical conditions.
To date, current treatment for AD patients relied on cholinesterase inhibitors, vitamin E, and symptomatic treatment.
Researchers examined 308 new cases of AD, diagnosed between 1997 and 2001, along with age-matched non-AD controls (n=3,088). Because females represented what study authors deemed a small proportion of the patient population (10.8%), they were excluded from the study.
The raw proportion of patients who filled their statin prescription prior to their AD diagnosis was 12.6% among cases; 15.1% among controls (OR 0.81, 95% CI 0.57-1.15). Compared to non-users, those with less than one year of statin use experienced reduced risk of AD (OR 0.56, 95% CI 0.34-0.92). Reductions were present among patients with hypertension, ischemic heart disease and cerebrovascular disease. Conversely, for patients with no cardiovascular risk factors, no association between statin use and lowered risk of AD was found.
Researchers identified 5 potential hypotheses for how statins may work to reduce dementia risk:
* Statins are designed to reduce an elevated cholesterol level, which is linked to an increased AD risk;
* Statins have a positive effect on cardiovascular risk, which is also a risk factor for AD;
* Statins affect production of [beta]-amyloid;
* Statins affect vascular dilation through nitric oxide;
* Statins affect inflammatory and oxidative stress markers tied to hyperlipidemia.
The authors acknowledge that the current study does not favor any one of their five hypotheses and recommend that more AD-statin association trials be conducted. Additionally, the authors recommend a closer examination of medication dosage, target cholesterol levels, and the role of different statins in future trials.
One limit of the study is that it cannot be generalized to cover AD patients who do not have the CVDs assessed in the study. Secondly, authors did not find a notable effect of duration of statin use and reduced risk of AD, suggesting that statin use pertaining to AD may have short-term effect only. Third, the study was limited to males only.
In conclusion, this study's results contribute to mounting evidence of an inverse association between AD diagnosis and statin use.
COPYRIGHT 2004 Advanstar Communications, Inc.
COPYRIGHT 2004 Gale Group