Abstract
Allergic rhinitis is the most prevalent chronic allergic disease in children. Although it is not life-threatening, it can have a significantly detrimental effect on a child's quality of life, and it may exacerbate a number of common comorbidities, including asthma and sinusitis. The Allergic Rhinitis and its Impact on Asthma guidelines, an evidence-based algorithm for the treatment of allergic rhinitis, advocate the use of antihistamines for the treatment of the broad spectrum of the disease. However, first-generation antihistamines are associated with a number of adverse events, including central nervous system impairment and anticholinergic and cardiovascular effects. Moreover, these agents have not been rigorously tested in the pediatric population. Nevertheless, first-generation antihistamines remain the most frequently prescribed agents in this class of drugs. This is despite the fact that the second-generation antihistamines are largely free of the undesirable side effects associated with their predecessors and the fact that they have been shown to be effective in relieving allergic rhinitis symptoms in children in a number of large-scale clinical trials. Therefore, when selecting an antihistamine for a child, it would be prudent to consider the full range of antihistamines and to base the selection of a particular drug on its efficacy, onset and duration of action, and safety profile.
Introduction
We have recently seen a rapid increase in the incidence of allergic disorders, particularly in the pediatric population. Of these, allergic rhinitis is the most common chronic allergic disease, and recent reports estimate that as many as 40% of children are affected by the condition. (1)
Allergic rhinitis is clinically defined as an allergen-induced inflammation of the nasal membranes and surrounding tissues that results in sneezing, rhinorrhea, conjunctivitis, nasal congestion, and pruritus of the nose, palate, throat, and/or ears. Allergic rhinitis can be classified as either intermittent or persistent; persistent allergic rhinitis is subclassified as either seasonal or perennial, depending on the duration and frequency of symptoms. Allergic rhinitis is most common in children; the mean age of patients at its onset is approximately 10 years and its incidence peaks between the ages of 13 and 19 years. (2,3)
Although allergic rhinitis is not an acute disease, it can have an important negative impact on the quality of life in children, impairing their learning performance, (4,5) reducing their ability to concentrate, (6,7) and causing disturbed sleep patterns. (7) Moreover, allergic rhinitis may also be associated with the development of other allergic diseases--the so-called allergic march. Left untreated, allergic rhinitis may exacerbate asthma, another prevalent childhood chronic disease with a high burden of morbidity. (8) A range of other disorders has also been linked to pediatric allergic rhinitis, including sinusitis, sleep apnea, nasal polyposis, nasal collapse, hearing impairment, abnormal craniofacial development, and impaired cognitive functioning. (9)
Given the high prevalence of allergic rhinitis in children, its negative impact on quality of life, and its potential to exacerbate or lead to other disorders, there is little doubt that the disease warrants effective treatment and management. In this article, the author reviews the efficacy, the onset and duration of action, and the safety of currently available treatments.
Overview of treatment options
As is the case with many other allergic disorders, first-line treatment for allergic rhinitis is allergen avoidance. The ease with which this can be accomplished depends on the type of allergen involved. Indoors, a range of measures can be taken to reduce the allergen load. Aggressive cleaning--particularly of carpets, curtains, and bedding--can be effective. However, the efficacy of nonallergenic bedcovering products is still questionable; whereas some studies have shown that they are associated with a reduction in allergic rhinitis symptoms, (10) others have found them to be of little benefit when used alone. (11) Ubiquitous aeroallergens such as pollen are harder to avoid, and patients who are sensitive to them are therefore more likely to require medication to relieve their symptoms.
The Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines were developed by the World Health Organization to establish an evidence-based protocol for the treatment of allergic rhinitis. (8) These guidelines provide a useful point of reference for physicians who treat both adults and children with allergic rhinitis. They contain a stepwise approach to treatment to maximize its beneficial effects while minimizing its adverse effects. In view of children's developmental vulnerability, the guidelines include a recommendation that physicians pay special attention to the risk/benefit ratio of any therapeutic intervention in this population.
The ARIA guidelines also include a review of the therapeutic agents that are indicated for the treatment of allergic rhinitis, including oral and intranasal antihistamines, intranasal glucocorticosteroids, local chromones, oral and intranasal decongestants, intranasal anticholinergics, and antileukotrienes. (8) The suitability and availability of these agents in children vary. For example, intranasal glucocorticosteroids, with their global effects on the inflammatory response, are indicated only for moderate-to-severe or persistent allergic rhinitis. The guidelines" authors express some concern about the use of intranasal glucocorticosteroids in children, and they stress the need for monitoring these children. Very few intranasal glucocorticosteroid therapies have been approved for children, and none is available for children younger than 3 years of age. In contrast, antihistamines are indicated for the broad spectrum of allergic rhinitis severity, and oral formulations of this drug class remain the mainstay of treatment in children.
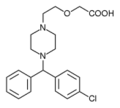
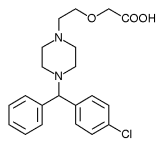
Phenbenzamine, the first available antihistamine, was developed in the 1940s. It was succeeded by a number of similar agents, including chlorpheniramine, brompheniramine, diphenhydramine, promethazine, and hydroxyzine. These older, first-generation antihistamines were associated with a range of adverse effects, including sedation, dry mucous membranes, and tachycardia. The second-generation agents--fexofenadine, loratadine, cetirizine, and azelastine were developed in recent years to reduce these side effects. A number of first- and second-generation oral and inhaled antihistamines have been approved for use in children and are available either as over-the-counter or prescription-only drugs (table).
Antihistamines are antagonists to the [H.sub.1] histamine receptor, and they reduce inflammation by blocking the histamine-driven inflammatory cascade. However, although all antihistamines mediate their therapeutic effects via the same primary mechanism, each agent has different properties, both positive and negative. Therefore, product selection should be tailored to the needs of each patient. A range of criteria should be borne in mind when making this selection, including efficacy, onset and duration of action, and safety profile because there are important differences among the antihistamines in each of these areas.
Efficacy
The best evidence of the benefits of antihistamine use in the pediatric population is provided by well-designed clinical trials. Such data are generally not available for the first-generation agents because they were introduced at a time when study requirements were less rigid than they are today. The most recent data on the first-generation agents derive from their use as active controls in studies of second-generation agents. This means that although diphenhydramine is the most widely used antihistamine in the United States, (12) its exact benefits in terms of symptom reduction are unclear, particularly in the pediatric population. The paucity of data from well-designed studies coupled with concerns over tolerability led a recent consensus group to recommend that the use of first-generation antihistamines should be limited in all patients with allergic rhinitis. (12)
The efficacy and safety of some second-generation antihistamines in children have been assessed in a number of well-designed clinical trials. Four of these agents are currently available for use in children in the U.S.: fexofenadine is indicated for use in children aged 6 years and older, loratadine for children 2 years or older, cetirizine for children 6 months and older, and azelastine for children 5 years and older. (The secondary metabolite of loratadine, desloratadine, is currently approved only for patients aged 12 years and older.) However, there have been no head-to-head trials among the second-generation agents in children, so direct comparisons are not possible.
Fexofenadine. In 2000, fexofenadine was approved in the U.S. for the treatment of seasonal allergic rhinitis in children aged 6 to 11 years. This antihistamine was shown to alleviate symptoms in a placebo-controlled, double-blind study of 935 children aged 6 to 11 years in 15 countries. (13) The primary endpoint of this study was the change from baseline in the mean total symptom score; these symptoms included sneezing; rhinorrhea; itchy nose, mouth, throat, and/or ears; and itchy, watery, and/or red eyes. Nasal congestion was assessed separately. At study's end, children who had taken fexofenadine 30 mg twice daily had a significantly lower mean total symptom score than did those in the placebo control group (p [less than or equal to] 0.0001). The mean change from baseline for the fexofenadine-treated group was 1.94 compared with 1.21 for the placebo group. Moreover, secondary endpoint analyses revealed that fexofenadine was significantly more effective than placebo in reducing individual symptom scores, including those for nasal congestion (p [less than or equal to] 0.05 for each symptom). The data also suggest that fexofenadine is rapidly effective, as improvement in both individual and total symptom scores were observed on the first day of treatment and were maintained throughout the entire 14-day trial.
Loratadine. Loratadine is available over the counter for the treatment of seasonal and perennial allergic rhinitis as a tablet (10 mg) for children aged 6 and older and as a syrup (5 mg/ml) for children aged 2 to 5 years. Trials of loratadine in the pediatric population have included only relatively small numbers of patients. The initial efficacy data on loratadine for seasonal allergic rhinitis were obtained during a 14-day trial of 40 children aged 3 to 6 years. (14) A total of 21 patients received loratadine syrup at 0.11 to 0.24 mg/kg ideal body weight once daily, and 19 children received first-generation dexchlorpheniramine syrup at 0.10 to 0.23 mg/kg every 8 hours. The efficacy data showed that loratadine was just as effective as dexchlorpheniramine in terms of alleviating nasal and ocular symptoms.
A randomized, double-blind, parallel-group study of 96 children aged 3 to 6 years with seasonal allergic rhinitis showed that the therapeutic response at the study's endpoint was rated by physicians as good or excellent in 82% of children who took loratadine syrup at 5 or 10 mg once daily for 14 days, compared with only 60% of those who took terfenadine suspension at 15 mg twice daily for 14 days. (15) According to physicians' ratings, treatment outcomes were similar across groups, except at day 14 when the response was significantly better in the loratadine group (p [less than or equal to] 0.02). Nasal and nonnasal symptom severities were also rated by physicians on a 4-point scale at baseline and on treatment days 3, 7, and 14. Mean nasal and nonnasal scores decreased significantly from baseline in both groups at each test point (p < 0.05), with greater nonnasal symptom improvement found in the loratadine group at day 14 (p = 0.05).
Cetirizine. Cetirizine is approved for the treatment of seasonal allergic rhinitis in children aged 2 years and older and for perennial allergic rhinitis in those aged 6 months and older. Several trials have evaluated cetirizine in children, but they all differed in scale, controls, and primary endpoints. (16-19) Overall, these studies have shown that cetirizine is an effective treatment for allergic rhinitis in children, but there is some variation in outcomes among these trials.
The largest of these trials was a randomized, double-blind, placebo-controlled study of cetirizine syrup at 5 and 10 mg once daily in the treatment of seasonal allergic rhinitis in 209 children aged 6 to 11 years. (16) At 4 weeks, cetirizine 10 mg was significantly better than placebo in lowering total symptom scores (p < 0.05): there was no significant difference between placebo and the 5-mg dose of cetirizine.
Another study showed that cetirizine at 5 and 10 mg was as effective as chlorpheniramine in reducing total symptom scores in 188 children aged 6 to 11 years with allergic rhinitis. (17) Similar studies have shown that cetirizine is effective in children and in infants as young as 6 months of age. (18,19)
Azelastine. Azelastine is approved for the treatment of seasonal allergic rhinitis in children aged 5 years and older. Unlike the other second-generation agents discussed here, azelastine is not an oral preparation: it is delivered as a nasal spray. The efficacy of azelastine in pediatric allergic rhinitis has not been clinically assessed. Instead, the efficacy of a 125-[micro]g dose has been extrapolated from adult studies. This dose was found to be sate and well tolerated in an initial series of controlled safety studies in 176 children aged 5 to 12 years who were treated over 6 weeks. (20) The efficacy of this dose has not yet been established in children.
Onset and duration of action
Given the relatively small variations in efficacy among the second-generation antihistamines, other factors--including the onset and duration of action and the incidence of side effects--are important considerations in the selection of treatment.
Antihistamines are often used intermittently, and as such they should have a rapid onset of action, which can minimize disruption of the patient's daily life. Histamine-induced wheal-and-flare skin reactivity testing is the gold standard for measuring the onset and duration of peripheral [H.sub.1] receptor blockade by an antihistamine. (21-25) This assay has been used widely in adult studies to assess the newer-generation antihistamines. For example, Simons and Simons used this technique to compare loratadine 10 mg and fexofenadine 120 mg. (26) They found that although both medications were effective in suppressing histamine-induced wheal and flare for 24 hours, fexofenadine had a significantly faster onset of action. In a similar comparative study, Day et al found that the onset of action of cetirizine 10 mg occurred at 1 hour, versus 3 hours with loratadine 10 mg. (27)
However, comparable pharmacologic data in children are limited, as studies of this nature in special populations have only recently been conducted. In one of the first of these studies, Simons et al compared the pharmacology of single doses of fexofenadine 30 mg and cetirizine 10 mg in children with allergies. (28) They enrolled 15 children (mean age: 8.8 [+ or -] 0.5 yr) in a randomized, double-blind, crossover, single-dose study. The authors found that while both cetirizine and fexofenadine significantly suppressed the wheal-and-flare reaction over the 24-hour test period, cetirizine demonstrated greater [H.sub.1] activity. However, it should be noted that the single test dose of fexofenadine was 30 mg, which is not the currently recommended daily dosage for children aged 6 to 11 years (the recommended dosage is 30 mg twice daily). Furthermore, cetirizine 10 mg is the larger of two available doses indicated for children and is equivalent to the adult dose. Children aged 6 to 24 months and 2 to 5 years can be prescribed 2.5 to 5 mg of cetirizine; the 2.5-mg dose is administered as one-half a teaspoon of syrup.
Although it is clear that this subject merits further research, it is important to recognize that wheal-and-flare testing is not a direct substitute for clinical efficacy trials. Further clinical pharmacologic trials should be conducted in this population.
Safety profile
First-generation antihistamines have long been associated with a range of adverse events, including impairment of the central nervous system (CNS) and anticholinergic and cardiovascular effects. Many of these adverse effects arise as a result of the first-generation agents' lower degree of specificity for the [H.sub.1] receptor and their propensity to cross the blood-brain barrier. Consequences are particularly serious in cases of overcompliance or overdose. More than 14,000 accidental exposures to first-generation antihistamines in children younger than 6 years of age occur every year in the U.S., and these exposures have resulted in several fatalities and severe toxic reactions.> For example, accidental ingestion of diphenhydramine caused multiple seizures and the eventual death of a 15-month-old boy. (30)
Second-generation antihistamines with [H.sub.1] receptor specificity are generally not associated with such adverse effects. Few cases of overdose have been reported, but when they have occurred, outcomes have been generally satisfactory. For example, an 18-month-old boy who ingested 180 mg of cetirizine remained asymptomatic and exhibited no electrocardiographic (ECG) abnormalities. (31)
Learning impairment. Studies have shown that poorly controlled allergic rhinitis can have a significant impact on a child's development and social integration, particularly with respect to learning performance. (4,7) It has been estimated that more than 1.5 million school days are lost each year in the U.S. as a direct result of allergic rhinitis. (4)
Unfortunately, treatment of allergic rhinitis with first-generation antihistamines appears to have exacerbated learning impairment. Vuurman et al compared the effects of antihistamines on children's learning ability and found that diphenhydramine caused significantly more impairment than did loratadine. (4) In a subsequent study, these same researchers found that diphenhydramine compounded the learning disability associated with allergic rhinitis. (32)
In contrast, second-generation antihistamines that cause significantly fewer adverse CNS effects may be less likely to have a negative impact on academic performance, particularly in children who require medication for prolonged periods of time. For example, in a large, double-blind study of 574 children, Reilly et al found that fexofenadine therapy was associated with reduced absenteeism and improved classroom performance. (33)
However, Bender et al reported that the intermittent use of antihistamines by patients with mild symptoms is unlikely to have any lasting negative effect on learning performance. (34)
Sedation. Sedation is the most common adverse effect associated with the first-generation antihistamines. It occurs secondary to the drugs' penetration of the blood-brain barrier. Indeed, a number of first-generation antihistamines--diphenhydramine, promethazine, and hydroxyzine--have been used to sedate children prior to electroencephalography (EEG), and they are still recommended by some physicians for sedation, pain relief; and as an antinausea medication for infants prior to surgery. (7) The authors of the ARIA guidelines recommend avoiding the "global impairment of psychomotor performance" observed with the older-generation antihistamines. (8)
Data from clinical trials in adults have established that some second-generation antihistamines are nonsedating. (35,36) Similar observations have been made in the pediatric population. (13,37) For example, during a safety study of fexofenadine in 875 children, the incidence of somnolence was comparable in those children who received the drag and in those who received placebo. (38) Similarly, Meltzer et al recently conducted a pooled analysis of three 2-week placebo-controlled trials of fexofenadine (at 15, 30, and 60 mg twice daily) in children aged 6 to 11 years with seasonal allergic rhinitis and found that the drug was not associated with any sedating effects. (37)
As is the case with their predecessors, however, second-generation antihistamines vary in their ability to cause adverse CNS effects. Some of these agents have been consistently found to be free of sedative effects, whereas others have been reported to be mildly sedating in children according to objective measurements. (39) For example, there is evidence that cetirizine causes sedation in some children at therapeutic doses, whereas recent meta-analyses have found that fexofenadine is the only second-generation antihistamine that is consistently not associated with adverse CNS effects. (40,41)
The need for objective rather than subjective assessments of sedation in this population was highlighted by a recent report from Ng et al. (39) They found that cetirizine 10 mg and chlorpheniramine 4 mg were associated with significantly (p < 0.03) greater degrees of P300 latency (an objective EEG-based measure of somnolence) than was placebo; however, when these patients self-rated their sedation on a visual analog scale, they reported no significant increase in sedation. Despite the difficulties of assessing the clinical relevance of the adverse effects of antihistamines on the CNS in children, further studies are clearly required in this area.
Anticholinergic effects. The poorer [H.sub.1] receptor specificity of the older antihistamines has resulted in a range of anticholinergic effects caused by blockade of muscarinic receptors. Dry mouth, urinary retention, tachycardia, and constipation have all been linked to a number of first-generation agents. In comparison, the newer [H.sub.1] antagonists have much lower affinities for muscarinic cholinergic receptors. (42) In studies of the safety of fexofenadine, (43) loratadine, (44) and cetirizine, (45) the incidence of anticholinergic adverse effects was equivalent to that seen with placebo.
Cardiovascular effects. Concerns over cardiotoxicity with first-generation and some second-generation antihistamines have largely centered on poor receptor selectivity and the blockade of cardiac potassium ion channels. A number of cases of QT prolongation as a consequence of this effect were reported in patients who took astemizole and terfenadine. However, these agents have subsequently been withdrawn from the market in most countries. (46) In addition, diphenhydramine has been shown to cause a moderate but significant increase in [QT.sub.c] intervals
The potential for fexofenadine, loratadine, and cetirizine to affect cardiovascular function has been examined, and none has been shown to have any effect on QT interval and other ECG parameters in children. In a safety study of fexofenadine, 14 children with allergic rhinitis received single doses of fexofenadine 30 or 60 mg. (43) Two-lead ECG measurements were taken before and 2.5 hours after dosing, and no abnormalities were found in any ECG rhythm strip. Similar ECG findings have been observed for loratadine (44) and cetirizine. (45) These findings were supported by in vitro measurements showing that fexofenadine, loratadine, and cetirizine have very low affinities for cardiac potassium ion channels. (48)
Conclusion
Despite the efficacy and popularity of first-generation antihistamines for the treatment of allergic rhinitis, these agents are associated with adverse effects in children. These effects can be avoided by using the currently available second-generation antihistamines, which have been shown to be not only safer, but just as effective. Given the number of second-generation preparations that are available and the differences in their specific pharmacologic attributes, care must be taken to match the particular drug to the needs of the individual child.
References
(1.) Management of Allergic and Nonallergic Rhinitis. Summary, Evidence Report/Technology Assessment: Number 54, May, 2002. Rockville, Md.: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality. www.ahrq.gov/clinic/ epesums/rhinsum.htm (accessed Feb. 2, 2005).
(2.) Druce HM, Kaliner MA. Allergic rhinitis. JAMA 1988;259:260-3.
(3.) Fagin J, Friedman R, Fireman P. Allergic rhinitis. Pediatr Clin North Am 1981;28:797-806.
(4.) Vurrman EF, van Veggel LM, Uiterwijk MM, et al. Seasonal allergic rhinitis and antihistamine effects on children's learning. Ann Allergy 1993;71:121-6.
(5.) Marshall PS, Colon EA. Effects of allergy season on mood and cognitive function. Ann Allergy 1993;71:251-8.
(6.) Juniper EF, Guyatt GH, Dolovich J. Assessment of quality of life in adolescents with allergic rhinoconjunctivitis: Development and testing of a questionnaire for clinical trials. J Allergy Clin Immunol 1994;93:413-23.
(7.) Meltzer EO. Quality of life in adults and children with allergic rhinitis. J Allergy Clin Immunol 2001;108(1 suppl):S45-53.
(8.) Bousquet J, Van Cauwenberge P, Khaltaev N. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 2001; 108 (5 suppl): S147-334.
(9.) Settipane RA. Complications of allergic rhinitis. Allergy Asthma Proc 1999:20:209-13.
(10.) Frederick J M, Warner JO, Jessop WJ, et al. Effect of a bed covering system in children with asthma and house dust mite hypersensitivity. Eur Respir J 1997;10:361-6.
(11.) Terreehorst I, Hak E, Oosting AJ, et al. Evaluation of impermeable covers for bedding in patients with allergic rhinitis. N Engl J Med 2003;349:237-46.
(12.) Casale TB, Blaiss MS, Geffand E, et al. First do no harm: Managing antihistamine impairment in patients with allergic rhinitis. J Allergy Clin Immunol 2003;111:S835-42.
(13.) Wahn U, Meltzer EO, Finn AF, Jr., et al. Fexofenadine is efficacious and safe in children (aged 6-11 years) with seasonal allergic rhinitis. J Allergy Clin lmmunol 2003;111:763-9.
(14.) Boner AL, Miglioranzi P, Richelli C, et al. Efficacy and safety of loratadine suspension in the treatment of children with allergic rhinitis. Allergy 1989;44:437-41.
(15.) Lutsky BN, Klose P, Melon J, et al. A comparative study of the efficacy and safety of loratadine syrup and terfenadine suspension in the treatment of 3- to 6-year-old children with seasonal allergic rhinitis. Clin Ther 1993;15:855-65.
(16.) Pearlman DS, Lumry WR, Winder JA, Noonan MJ. Once-daily cetirizine effective in the treatment of seasonal allergic rhinitis in children aged 6 to 11 years: A randomized, double-blind, placebo-controlled study. Clin Pediatr (Phila) 1997;36:209-15.
(17.) Tinkelman D, Kemp J, Mitchell D, et al. Treatment of seasonal allergic rhinitis in children with cetirizine or chlorpheniramine: A multicenter study. Pediatr Asthma Allergy Immunol 1996; 10: 9-17.
(18.) Allegra L, Paupe J, Wieseman HG, Baelde Y. Cctirizine for seasonal allergic rhinitis in children aged 2-6 years. A double-blind comparison with placebo. Pediatr Allergy Immunol 1993:4:157-61.
(19.) Simons FE, Silas P, Portnoy JM, et al. Safety of cetirizine in infants 6 to 11 months of age: A randomized, double-blind, placebo-controlled study. J Allergy Clin Immunol 2003:111:1244-8.
(20.) Astelin (Azelastine product information package insert). Somerset, N.J.: MedPointe Pharmaceuticals, 2003. www.astelin.com/ AstelinPI.pdf (accessed Feb. 2, 2005).
(21.) Simons FE, McMillan JL, Simons KJ. A double-blind, single-dose, crossover comparison of cetirizine, terfenadine, loratadine, astemizole, and chlorpheniramine versus placebo: Suppressive effects on histamine-induced wheals and flares during 24 hours in normal subjects. J Allergy Clin Immunol 1990:8614 Pt 1):5407.
(22.) Rivest J, Despontin K, Ghys L, et al. Pharmacological modulation by cetirizine and ebastine of the cutaneous reactivity to histamine. Dermatologica 1991;183:208-11.
(23.) Grant JA, Riethuisen JM, Moulaert B, DeVos C. A double-blind, randomized, single-dose, crossover comparison of levocetirizine with ebastine, fexofenadine, loratadine, mizolastine, and placebo: Suppression of histamine-induced wheal-and-flare response during 24 hours in healthy male subjects. Ann Allergy Asthma Immunol 2002;88:190-7.
(24.) Frossard N, Purohit A, Kovacs S, et al. Fexofenadine is superior to loratadine and desloratadine in onset of action of histamine-induced wheal and flare inhibition. Ann Allergy Asthma Immunol 2003;90:124.
(25.) Purohit A, N'Gom AS, Deslandes B, et al. Similar rapid onset of action and magnitude of effect of fexofenadine and cetirizine as assessed by inhibition of histamine-induced wheal-and-flare reaction. Ann Allergy Asthma Immunol 2004:93:562-67.
(26.) Simons FE, Simons KJ. Peripheral HI-blockade effect of fexofenadine. Ann Allergy Asthma Immunol 1997:79:530-2.
(27.) Day JH, Briscoe M, Rafeiro E, et al. Comparative onset of action and symptom relief with cetirizine, loratadine, or placebo in an environmental exposure unit in subjects with seasonal allergic rhinitis: Confirmation of a test system. Ann Allergy Asthma Immunol 2001;87:474-81.
(28.) Simons FE, Serous M, Goritz SS, Simons KJ. H1-antihistaminic activity of cetirizine and fexofenadine in allergic children. Pediatr Allergy Immunol 2003;14:207-11.
(29.) Litovitz T, Holm K, Bailey K, Schmitz B. Demographic profile of exposure cases by generic category of substances and products: Nonpharmaceuticals. Annual Report of the American Association of Poison Control Centers National Data Collection System. 1991: 477-89.
(30.) Goetz CM, Lopez G, Dean BS, Krenzelok EP. Accidental childhood death from diphenhydramine overdosage. Am J Emerg Med 1990;8:321-2.
(31.) Ridout SM, Tariq SM. Cetirizine overdose in a young child. J Allergy Clin Immunol 1997;99(6 Pt 1):860-1.
(32.) Vuurman EF, van Veggel LM, Sanders RL, et al. Effects of semprex-D and diphenhydramine on learning in young adults with seasonal allergic rhinitis. Ann Allergy Asthma Immunol 1996;76: 247-52.
(33.) Reilly MC, Tanner A, Meltzer EO. Work, classroom and activity impairment instruments: Validation studies in allergic rhinitis. Clin Drug Invest 1996;11:278-88.
(34.) Bender BG, McCormick DR, Milgrom H. Children's school performance is not impaired by short-term administration of diphenhydramine or loratadine. J Pediatr 2001;138:656-60.
(35.) Weiler JM, Bloomfield JR, Woodworth GG, et al. Effects of fexofenadine, diphenhydramine, and alcohol on driving performance. A randomized, placebo-controlled trial in the Iowa driving simulator. Ann Intern Med 2000;132:354-63.
(36.) Nicholson AN, Handford AD, Turner C, Stone BM. Studies on performance and sleepiness with the H1-antihistamine, desloratadine. Aviat Space Environ Med 2003;74:809-15.
(37.) Meltzer EO, Scheinmann P, Rosado Pinto JE, et al. Safety and efficacy of oral fexofenadine in children with seasonal allergic rhinitis--A pooled analysis of three studies. Pediatr Allergy Immunol 2004;15:253-60.
(38.) Graft DF, Bernstein DI, Goldsobel A, et al. Safety of fexofenadine in children treated for seasonal allergic rhinitis. Ann Allergy Asthma Immunol 2001;87:22-6.
(39.) Ng KH, Chong D, Wong CK, et al. Central nervous system side effects of first- and second-generation antihistamines in school children with perennial allergic rhinitis: A randomized, double-blind, placebo-controlled comparative study. Pediatrics 2004; 113: el 16-21.
(40.) Hindmarch I, Shamsi Z. Antihistamines: Models to assess sedative properties, assessment of sedation, safety and other side-effects. Clin Exp Allergy 1999;29(suppl 3): 133-42.
(41.) Shamsi Z, Hindmarch I. Sedation and antihistamines: A review of inter-drug differences using proportional impairment ratios. Hum Psychopharmacol 2000; 15(S1):S3-S30.
(42.) Snyder SH, Snowman AM. Receptor effects of cetirizine. Ann Allergy 1987;59(6 Pt 2):4-8.
(43.) Simons FE, Bergman JN, Watson WT, Simons KJ. The clinical pharmacology of fexofenadine in children. J Allergy Clin Immunol 1996;98(6 Pt 1):1062-4.
(44.) Salmun LM, Herron JM, Banfield C, et al. The pharmacokinetics, electrocardiographic effects, and tolerability of loratadine syrup in children aged 2 to 5 years. Clin Ther 2000;22:613-21.
(45.) Diepgen TL. Long-term treatment with cetirizine of infants with atopic dermatitis: A multi-country, double-blind, randomized, placebo-controlled trial (the ETAC trial) over 18 months. Pediatr Allergy Immunol 2002;13:278-86.
(46.) Yap YG, Camm AJ. Potential cardiac toxicity of H1-antihistamines. Clin Allergy Immunol 2002;17:389-419.
(47.) Zareba W, Moss A J, Rosero SZ, et al. Electrocardiographic findings in patients with diphenhydramine overdose. Am J Cardiol 1997;80:1168-73.
(48.) Pratt C, Brown AM, Rampe D, et al. Cardiovascular safety of fexofenadine HC1. Clin Exp Allergy 1999;29(suppl 3):212-16.
From the Division of Cell Biology, Department of Pediatrics, National Jewish Medical and Research Center, Denver.
Reprint requests: Erwin W. Gelfand, MD, Department of Pediatrics, National Jewish Medical and Research Center, 1400 Jackson St., Denver, CO 80206. Phone: (303) 398-1196; fax: (303) 270-2105; e-mail: gelfande@njc.org
The preparation of this article was supported by an educational grant from Aventis Pharmaceuticals of Bridgewater, N.J.
COPYRIGHT 2005 Medquest Communications, LLC
COPYRIGHT 2005 Gale Group