Background & objectives: Haemophilus influenzae causes a variety of life threatening infections in humans. Early detection of antimicrobial resistance is of importance in the treatment and management of infection. The modified Slack's method, a simple assay, has been evaluated in this study for the early detection of chloramphenicol resistance.
Methods: Fifty isolates of H. influenzae from invasive and non-invasive sites were included. Antimicrobial susceptibility testing was done by disc diffusion method and minimum inhibitory concentration (MIC) determination was performed for chloramphenicol only. Modified Slack's method was used to test for the production of chloramphenicol acetyl transferase (CAT).
Results: Invasive isolates showed,higher degree of resistance to chloramphenicol (72%) compared to non-invasive ones (28%). One hundred per cent association was found between results of disc diffusion, MIC and CAT production amongst strains resistant to chloramphenicol.
Interpretation & conclusion: The findings suggested that chloramphenicol still remains the drug of choice for treatment for non-invasive infection caused by H. influenzae. Modified Slack's method is a simple, rapid, inexpensive and reliable method for the detection of chloramphenicol resistance amongst H. influenzae.
Key words Acetyl transferase - chloramphenicol - Haemophilas influenza - invasive & non-invasive - modified Slack's method -- resistance
Haemophilus influenzae is a well recognized cause of a variety of serious life threatening infections in humans. Meningitis due to H. influenzae is the most serious acute manifestation of systemic infections and occurs primarily in children under 5 yr of age with 80-90 per cent in the age group 1 month to 3 yr1. With prompt appropriate antibiotic therapy as well as proper clinical management the overall mortality rate in H. influenzae meningitis can be reduced to
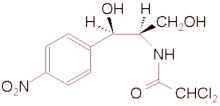
Two mechanisms of resistance to chloramphenicol by H. influenzae have been described. The first is through the plasmid mediated production of chloramphenicol acetyl transferase (CAT) seen in 98-99 per cent of the strains and the second is by chromosomally mediated permeability barrier to chloramphenicol by the loss of a porin proteins.11 Little work has been done so far to correlate the resistance of chloramphenicol to the production of CAT in H. influenzae. There is a lacunae in literature on this aspect especially from India. The objective of the present study was to determine the in vitro susceptibility pattern of invasive and non-invasive strains of H. influenzae to chloramphenicol and to correlate the findings to the production of CAT as determined by a rapid and reliable method12.
Material & Methods
Bacterial isolates: H. influenzae isolates from invasive and non-invasive sites were examined. A total of 50 strains of H. influenzae were inlcuded in the study. Twenty five strains were collected from children in the age group of 3 months to 5 yr clinically diagnosed to have meningitis during January 1998 to June 1999. The other 25 isolates were from sputum (21), throat (3) and eye (1) and were collected during a 3 month period between April 1999 and June 1999. The non-invasive strains were collected from patients in the age group of 19-70 yr. Twenty of the sputum samples were from patients with lower respiratory tract infections, one sample was from a patient with pulmonary tuberculosis. All the three throat swabs were from patients with upper respiratory tract infections while the eye specimen was from a patient with conjunctivitis.
The bacterial isolates were identified by their colony characterisitcs on chocolate agar and their requirement for X and V factors3. A single colony of the bacterial isolate on chocolate agar was used for antimicrobial susceptibility testing and for production of chloramphenicol acetyl transferase. Antimicrobial susceptibility testing: This was carried out by both disc diffusion method (chloramphenicol 30 (mu)g, Becton Dickinson, USA) as well as by determination of minimum inhibitory concentration (MIC)13 to chloramphenicol (Sigma Chemicals, USA). The interpretation was by standard criteria laid -down by the National Committee for Clinical Laboratory Standards (NCCLS)14.
Rapid detection of chloramphenicol acetyl transferase production: The original rapid Slack's method with certain modifications was used for this purpose12. Hence this method is referred to as the modified Slack's method. The following modifications were done: Mueller Hinton agar was used for testing instead of Columbia agar as suggested by Slack et al12;ATCC 25922 strain of Escherichia coli was used by us against Esch. coli NCTC strain 10418 used in the original method, and 30 tg chloramphenicol disc was used instead of 10yg disc used in the original method12. Our modifications were based on the fact that NCCLS guidelines were followed for interpretation of the test readings, hence the media, ATCC Esch. coli strain and chloramphenicol disc used in this modified method were in accordance with NCCLS recommendations14.
A plate of Mueller Hinton agar was flooded with a barely turbid broth culture (MacFarland opacity of 0.5) of chloramphenicol susceptible Esch. coli ATCC 25922. The plate was dried to remove the surface fluid and discs of Whatmann no. 1 filter paper 8.5 mm were placed on the inoculated plate. With the help of an inoculating wire loop, growth was scraped from the surface of the H. influenzae culture to be tested. This heavy inoculum of the organism was applied evenly over the surface of the 8.5 mm filter paper disc. After 5 Tin Whatmann no. 1 filter paper (6 mm size) discs wetted with chloramphenicol, were carefully placed centrally on the larger Whatmann filter disc, which has been inoculated with the test organism. CAT produced by test strain diffuses through the larger outer disc and inactivates the chloramphenicol and hence Esch. coli growth is not inhibited.
If chloramphenicol has diffused into the external medium in the active form (implying that it has passed through the 8.5 mm disc seeded with a chloramphenicol susceptible strain of H. influenzae) it inhibits Esch. coli, thereby producing a zone of inhibition of Esch. coli and this is associated with the production of CAT viz., 18 mm - CAT produced (chloramphenicol resistant strain); > 18 mm - CAT not produced (chloramphenicol susceptible strain). Results are interpreted with 4 h.
Results & Discussion
A total of 50 isolates of H. influenzae during the period January 1998 through June 1999 were included in the study. These included 25 isolates from children with meningitis and an equal number of non-invasive isolates. In the invasive category resistance to chloramphenicol was 72 per cent while among the non-invasive it was 28 per cent.
One hundred per cent association was observed between the results of the disc diffusion, MIC and modified Slack's method (Table). All the resistant strains were positive for the production of CAT, this is an observation of interest.
Among the invasive isolates of H. influenzae resistance to chloramphenicol has shown a steady increase. In a previous study at our center conducted between 1987-1991 resistance to chloramphenicol was 42.5 per cent10. Preliminary results of a previously conducted multicentric invasive bacterial infection surveillance study revealed a resistance level of 55 per cent15. In another study done at Nagpur chloramphenicol resistance was 66.7 per cent16. In this study among the 25 invasive strains tested resistance to chloramphenicol was 72 per cent. These results are in variance with those obtained in the previous studies. This increasing trend in resistance of invasive H. influenzae to chloramphenicol is a cause for concern. However, it should also be noted that in this study all the invasive isolates were from CSF and these represent a subset of the invasive isolates. In terms of therapy our results further reinforce the fact that chloramphenicol is not the drug of choice for treatment of meningitis due to H. influenzae.
Among the non-invasive isolates which were mostly isolated from sputum and throat swabs the resistance to chloramphenicol was 28 per cent; this is in variance with the results of a recent study's where no resistance was seen among nasopharyngeal isolates of H. influenzae. It is to be noted that there are very few studies in India that have looked at the susceptibility pattern of H. influenzae from noninvasive sites. From the results of our study it could be concluded that chloramphenicol still remains relevant in the treatment of conditions caused by non-invasive H. influenzae. The difference in the resistance patterns between invasive and noninvasive strains to the commonly used antimicrobials suggests that there could exist different mechanisms of drug metabolism between these two groups mirrored by difference in their pathogenicity or this difference may be due to the level of antibiotic usage in these two groups.
The modified Slack's method is a simple, rapid and inexpensive technique to determine the production of CAT. Results of the test are available within 4 h. This method has been found to be very accurate and showed agreement with the disc diffusion and MIC findings. All the chloramphenicol resistant strains among both invasive and noninvasive categories were CAT positive by this method and this is a significant finding. A spectrophotometric assay18 is also described to detect CAT, however this assay takes about 2 days. Another rapid assay can also be used, however this method requires the use of expensive chemicals. The modified Slack's method overcomes all these difficulties, but in this method care should be taken in performing the test accurately and in taking readings.
References
1. Smith DH. Haemophilus influenzae. In: Mandell GL, Douglas RG Jr, Bennett JE, editors. Principles and practices of infectious diseases, Vol. II, 4th ed. New York : John Wiley and Sons; 1979 p. 1759-72.
2. Bolan G. Barza M. Acute bacterial meningitus in children and adults. A perstective. Med Clin North Am 1985; 69: 231-41.
3. Campos JM. Haemophilus. In : Murray PR, Baron EJ, Pfaller MA, Tenover FC, Yolken RH, editors. Manual of clinical microbiology, 6th ed. Washington Dc : American Society for Microbiology; 1995 p. 556-63.
4. Khan W, Ross S, Rodriguez W, Controni G, Saz AK. Haemophilus influenzae type B resistant to ampicillin. A report of two cases. JAMA 1974; 229 : 298-301.
5. Tomeh MO, Starr SE, McGowan JE Jr, Terry PM, Nahmias AJ, Ampicillin - resistant Haemophilus influenzae type B infection. JAMA 1974; 229 : 295-7.
6. Manten A, van Klingeren B, Dessens-Kroon M. Chloramphenicol resistance in Haemophilus influenzae. Lancet 1976; i : 702.
7. Azemun P, Stull T, Roberts M, Smith AL. Rapid detection of chloramphenicol resistance in Haemophilus influenzae. Antimicrob Agents Chemother 1981; 20 : 168-70.
8. van Klingeren B, van Embden JDA, Dessens-Kroon M. Plasmid-mediated chloramphenicol resistance in Haemophilus influenzae. Antimicrob Agents Chemother 1977; 11 : 383-7.
9. Ayyagari A, Kaur P, Sachdeva S, Kumar L. Meningitis due to beta lactamase producing type 'b' Haemophilus influenzae resistant to chloramphenicol in India - a case report. Indian J Pediatr 1984; 51: 615-7.
10. Singh R, Thomas S, Kirubakaran C, Lalitha MK, Raghupathy P. Occurrence of multiple antimicrobial resistance among Haemophilus influenzae type b causing meningitis. Indian J Med Res 1992; 95 : 230-3.
11. Burns JL, Mendelman PM, Levy J, Stull TL, Smith AL. A permeability barrier as a mechanism of chloramphenicol resistance in Haemophilus influenzae. Antimicrob Agents Chemother 1985; 27: 46-54.
12. Slack MPE, Wheldon DB, Turk DC. Rapid detection of chloramphenicol resistance in Haemophilus influenzae. Lancet 1977; ii : 1366.
13. World Health Organization. Manual for the national surveillance of antimicrobial resistance of S pneumoniae and H. influenzae: Epidemiological and microbiological methods. Geneva World Health Organization, Atlanta Center for Disease Control 1991: p. 11-25.
14. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibilitytesting, 8th Informational supplement. NCCLS document M 100-S8, Villanova, PA: National Committee for Clinical Laboratory Standards; 1998.
15. Steinhoff MC. Invasive Haemophilus influenzae disease in India : a preliminary report of prospective multihospital surveillance. IBIS (Invasive Bacterial Infections Surveillance) Group. Pediatr Infect Dis J 1998: 17 : S172-5.
16. Agarwal V, Jain D, Pathak AA, Saoji AM. Characterization of invasive Haemophilus influenzae isolated in Nagpur, cantral India. Indian J Med Res 1996: 103: 296-8.
17. Puri J, Talwar V, Juneja M, Agarwal KN, Gupta HC, Prevalence of antimicrobial resistance among respiatory isolates of Haemophilus influenzae. Indian J Pediatr 1999: 36 : 1029-32.
18. Roberts MC, Swenson CD, Owens LM, Smith AL. Characterization of chloramphenicol-resistance Haemophilus influenzae. Antimicrob Agents Chemother 1980; 18 : 610-5.
N. Satish, Anand Manoharan, R, Pai & M.K. Lalitha
Department of Microbiology, Christian Medical College & Hospital, Vellore, India
Received March 9, 2001
Copyright Indian Council of Medical Research Aug 2001
Provided by ProQuest Information and Learning Company. All rights Reserved