Q & A Infection Protection is a monthly column dedicated to education about infection control issues. Every fourth issue includes a Q&A column to answer your questions about recent articles. We are pleased to publish your questions and hope you find the responses useful. If you have a question, please submit it to jakridge@hpnonline.com or call (941)927-9345 ext. 202.
Cynthia T. Crosby
Vice President, Clinical Affairs, Medi-Flex, Inc.
Question: We read your article about surgical fires with interest. Our OR staff and hospital administrators want to be proactive and improve our procedures to reduce surgical fire risk. But we are concerned that there is a push toward eliminating alcohol based preoperative antimicrobial skin preparations, which might increase the risk of infection among our patients. Do you have examples of what other hospitals or policy organizations are recommending to reduce fire risk without exposing the patient to more infection risk?
Answer: Balancing the risk of surgical fire with infection control is a significant issue, as you point out. The 2005 AORN Guidance Statement: Fire Prevention in the Operating Room reiterates the need to use flammable prep solutions with caution, which includes avoiding pooling, allowing fumes to evaporate and ensuring that ignition sources are kept away from prep solutions. Drapes that remain in contact with the patient should not be allowed to absorb flammable prep solutions. (1)
In September 2004, the Texas Department of State Health Services published its Position Statement Regarding the Use of Alcohol-Based Surgical Skin Preparations. This document was published in response to questions from hospitals and ambulatory surgical center providers regarding licensing rules prohibiting the use of flammable germicides for preoperative preparation of the surgical field. (2) The statement acknowledged that literal interpretation of the rule would prohibit the use of any alcohol-based surgical skin preparation. However, the statement differentiated between literal interpretation and the intention of the role, providing clarification that effective products could be used as long as there is evidence to support their safety for patients. Alcohol-based products with demonstrated efficacy can be used by qualified staff under certain circumstances. (The full statement can be found at the URL listed in the references.) Some additional precautions were listed in the Texas guidelines that may be useful in your effort to develop detailed policies regarding surgical fire prevention. These include the use of self-contained single-used, pre-measured applicators to apply alcohol-based surgical skin preparations and the need to follow product safety warnings and institute detailed policies and procedures outlining precautions in the use of products. The position paper includes requirements for documenting details about the prepping procedure, along with training and reporting guidelines. These recommendations are one example of how policy regarding surgical fires is being addressed and clarified in one state.
Question: In your article about chlorhexidine dressings, you didn't mention anything about their effectiveness in the presence of antibiotic-resistant bacteria. Do you have any information about that?
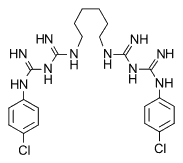
Answer: Yes, an in vitro study was published that evaluated hydrophilic polyurethane foam dressing with chlorhexidine gluconate to determine its effects against several antibiotic-resistant isolates. Sterile foam with chlorhexidine was compared to untreated control dressing materials. The polyurethane foam with chlorhexidine was effective in killing all organisms, including antibiotic-resistant strains of Staphylococcus, Enterococcus and Candida species. (3)
Question: I work in Illinois, one of the states that requires reporting of health-associated infections. I know several other states have legislation pending to require state reporting, but do you know whether there will eventually be national reporting standards?
Answer: According to the Centers for Disease Control (CDC), healthcare-associated infections account for 90,000 deaths and $4.5 billion dollars in excess costs of care each year. (4) Four states--Florida, Illinois, Missouri and Pennsylvania-now have mandatory reporting rules, and 30 other states have legislation pending. The CDC has recently released recommendations for policymakers who are developing mandatory reporting systems. Currently, there is no national reporting system planned, but the CDC is encouraging mandatory reporting at the state level to protect patients. The CDC's Healthcare Infection Control Practices Advisory Committee (HICPAC) has released guidelines, which are available on the CDC website. (See the URL listed in the references.) Key recommendations in the guidelines include:
* using established public health surveillance methods
* involving people with infection control expertise in the reporting process
* tracking practices that prevent infections, in addition to measuring infection rates
* providing regular and confidential feedback to healthcare professionals
It is interesting to note that the CDC recommends tracking infection control practices, as well as infection rate outcomes. Practices often are predictors of outcomes, and tracking infection control activities will allow institutions to share knowledge that can help reduce infection rates. Specific outcome measures suggested by the CDC for tracking healthcare-acquired infections include:
* central-line insertion practices
* surgical antimicrobial prophylaxis
* influenza vaccination coverage for patients and healthcare staff
* central line-associated bloodstream infections
* surgical site infections following selected operations
These new guidelines will continue to be updated as new information is collected. More detailed information about the guidelines and the effort to expand reporting will appear in a future issue of "Infection Protection".
References
(1.) AORN Guidance Statement Fire Prevention in the Operating Room, 2005 Standards, Recommended Practices, and Guide lines. AORN. Available at: http://www.aorn.org/about/positions/pdf/SECTI-2e-firesafety.pdf. Accessed on March 1, 2005.
(2) Position Statement Regarding the Use of Alcohol Based Surgical Skin Preparations Texas Department of State Health Ser vices Available at: http://www.penonline.org/documents/ TexasDept of StateHealthServicesPositionStatementonAlcoholBasedSurg.Preps.pdf. Accessed on March 1, 2005.
(3) Bhende S, Spangler D. In vitro assessment of clorhexidine gluconate-impregnated polyurethane foam antimicrobial dressing using zone of inhibition assays. Infect Control Hosp Epidemiol. 2004;25(8):664-667.
(4) Centers for Disease Control CDC Advisory Committee Offers Guidance to States on Developing Systems for Public Reporting of Healthcare-Associated Infections. Available at: http:// www cdc.gov/od/oc/media/pressrel/r050228.htm.
COPYRIGHT 2005 Healthcare Purchasing News
COPYRIGHT 2005 Gale Group