Special programs for nursing students and faculty members of schools of nursing were presented at this year's Congress. Students were allowed to attend Congress free of charge and invited to a networking breakfast and a special one-day program designed to introduce them to the OR. Faculty members were invited to attend the networking breakfast and a three-hour session about the Perioperative Nursing Data Set (PNDS) and using the OR for clinical experience.
STUDENTS LEARN ABOUT PERIOPERATIVE NURSING
More than 200 students attended a special Congress program designed just for them on Wednesday, March 26, 2003. The program consisted of three parts--didactic instruction, which focused on aseptic technique, electrosurgery, and patient safety; an assignment; and hands-on instruction. Joy Don Baker, RN, PhD, CNOR, CNA, welcomed attendees to the program, saying, "You represent the people who are going to take care of us."
A student's view. Tracy Albanese, a student from Shepherd College in Shepherdstown, WV, attended Congress with her professor, Kathleen B. Gaberson, RN, PhD, CNOR. At the member ambassador recognition breakfast held at the 2002 Congress, William J. Duffy, RN, BSN, MJ, CNOR, Treasurer, won complimentary registration, airfare, and lodging for the 2003 Congress. As a Board member and resident of Chicago, Duffy gave his prize to Dr Gaberson so she could bring a student.
"As a student, I really enjoyed the sessions on different surgeries, patient safety, and ethics," said Albanese. She explained that although she learns about general principles and basic techniques in school, Congress allowed her the opportunity to apply this information in a concrete way. When asked whether she plans to practice in the OR, Albanese said, "I still feel wide eyed. Everything's new." She did, however, say that a positive clinical experience in the OR and experiences at Congress have "definitely encouraged me to lean toward the OR."
Aseptic technique. Dr Gaberson discussed definitions related to aseptic technique, related recommended practices, and principles and application of aseptic technique. Protecting patients from infection "is one of the most important things perioperative nurses do," according to Dr Gaberson. She told students, "We have to report all breaks in aseptic technique immediately." She also explained that an item either is contaminated or it is not--there are no gray areas.
Of nursing standards and recommended practices, Dr Gaberson told students, "Organizations make a conscious decision they are going to adhere to them." Standards relate to technical practice and represent what nurses should do in ideal situations. Recommended practices relate to various issues, including traffic patterns. "Did you know the perioperative nurse has to be a traffic manager?" Dr Gaberson asked.
One principle of aseptic technique Dr Gaberson discussed is that the edges of anything that encloses sterile contents are considered unsterile. "This is a very strange principle," she said, explaining that when anything is opened, it becomes a sterile field, and the inside of the wrapper is considered sterile to within 1 inch of the edge. "In reality, this is not the way it goes," Dr Gaberson commented, alluding to the fact that if tested in a laboratory, this would not be a hard and fast rule.
Electrosurgery. Judith Eagan, RN, BS, CNOR, discussed the basic principles and clinical applications of electrosurgery; safety concerns when using electrosurgery, and recommended practices related to electrosurgery. She told attendees that an electro-surgical unit is the most hazardous medical device used on a daily basis, but it is used because "the pros outweigh the cons."
Eagan gave an overview of the basic principles of electricity. She explained its properties, the frequency spectrum, different types of waveforms, and the differences between monopolar and bipolar surgery. Monopolar surgery uses one electrode that delivers electricity to a patient and collects it somewhere on his or her body. Bipolar surgery has both active and return poles in one instrument (eg, forceps). "Inherently, bipolar is safer," Eagan said.
In relating information on electrosurgery to nursing practice, Eagan said, "The hospital staff is responsible for maintaining this equipment." There have been many changes and advances in technology, but not all hospitals have the most recent equipment, so being familiar with these principles is important. Nurses also should be aware of the issue of flammability because "it is possible in the right circumstances to start a fire," said Eagan. Three things are needed to start a fire--heat, fuel, and oxidizers. In the OR, surgeons typically provide the heat, nurses the fuel, and anesthesia care providers the oxidizers. "[Fires] occur frequently in the OR, so it requires the vigilance of the staff," Eagan said.
Possible adverse outcomes resulting from the use of electrosurgery include patient return electrode burns, alternate site burns, ignition incidents, and injuries caused by the effects of stray current. According to Eagan, health care professionals never discuss the potential for electrosurgical burns when having patients sign consent forms. "Imagine how happy you'd be," she said.
Patient safety. Before discussing patient safety, Linda K. Groah, RN, MS, CNOR, CNAA, FAAN, said that as a nursing student she hated the OR because "of the way the OR nurses treated the students." The message perioperative nurses now send to students has changed, she noted.
Groah's discussion on patient safety centered on three issues, including identifying an RN's role in patient safety, identifying major risk factors, and defining human factors and their effect on caring for surgical patients. She identified types of errors, including slips, lapses, mistakes, and violations. Slips happen when "your mind is somewhere else," according to Groah.
There are many types of medical errors. Some specific to the OR include medication errors, wrong site surgery, transfusion mistakes, nosocomial infections, burns, falls, and pressure ulcers. Reasons for medical errors include psychological precursors; unsafe acts; and organization, team, individual, and technical errors. Referring to how errors occur in terms of the now-popular Swiss cheese model, Groah said, "If enough of those things are lined up, an error will occur."
Investigation of errors often focuses on the sharp end (ie, the people) instead of the blunt end (ie, the environment). "We have this habit of always wanting to place blame," Groah said. "If all we're going to do is point fingers, we're never going to get to the causation."
Groah described human factors as the interaction between humans and devices, saying it is time for organizations to use this approach to make services safer. Human factors skills include communication, briefings, cross checking and verifying, situational awareness, assertion, and decision making. She called assertion "an important part of human factors training." Groah told students that they need to be assertive if they observe behavior that could lead to an error.
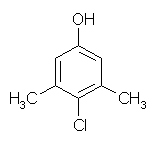
Assignment. Students were given an assignment that, according to Dr Gaberson, was not bad because "it doesn't have to be typed in APA style." The assignment entailed going to the exhibit floor, finding the answers to four questions, and having exhibitors initial the assignment to show that students found the answers. The questions involved identifying the characteristics of latex, nonlatex, and powder-free gloves; identifying different types (ie, povidone-iodine, chlorhexidine gluconate, hexachlorophene, chloroxylenol) of antimicrobial agents for hand scrubs or patient skin prep; identifying the equipment used to achieve sterilization by steam, peracetic acid, and hydrogen peroxide; and identifying specific technologies (ie, electrosurgical units, overhead OR lights, endoscopes, robotics) used in surgical patient care.
Hands-on instruction. Students ended their specialized program with hands-on instruction in the areas of prepping and cautery. More than 50 expert volunteers showed students the appropriate way to prep patients' upper torsos using povidone-iodine and how to use an electrosurgical unit, which was demonstrated on an orange. Students found this part of the session informative and fun.
FACULTY MEMBERS ENCOURAGED TO CONSIDER THE OR
Faculty members from a variety of colleges of nursing and health care education programs also gathered on Wednesday. They attended a program titled "Integrating the Perioperative Experience." Susan V. M. Kleinbeck, RN, PhD, CNOR, focused on how faculty members can incorporate the PNDS in their curriculum.
Dr Kleinbeck explained the basics of the PNDS, including assessments, nursing interventions, and outcomes. "The PNDS makes [perioperative] practice more visible," she said, adding that it helps perioperative nurses explain what they do to their colleagues. "Nurses have a hard time articulating what they do. The PNDS can help because it describes the activities of perioperative nursing," said Dr Kleinbeck. The PNDS is a coded vocabulary with standardized definitions, which makes it a perioperative dictionary. The language is detailed enough so even nurses from outside the perioperative arena can use it for teaching, said Dr Kleinbeck.
The PNDS adapts well to the classroom setting because it focuses on patient outcomes rather than tasks, and faculty members with limited perioperative experiences easily can identify what nurses should do and patient outcomes, said Dr Kleinbeck. She emphasized that the PNDS is not a standard of care. "The PNDS tries to address all areas of perioperative practice, but you don't have to do it all."
The PNDS activities are not coded, so they can be adjusted to meet the criteria of individual facilities to achieve common interventions or outcomes. Dr Kleinbeck noted that education on the PNDS can be divided into six modules, including
* course introduction,
* safety domain,
* physiologic responses domain,
* behavioral responses domain,
* health system domain, and
* final evaluation.
She emphasized that the most useful way to disseminate the PNDS nomenclature is for faculty members to use it in their classes. "The PNDS clearly reflects actual practice of perioperative nurses," said Dr Kleinbeck. Attendees were encouraged to access AORN's electronic mailing list on the PNDS at http://www.aorn.org/pnds/list.
Linda M. Sigsby, RN, MS, then told attendees about a study she conducted on student perioperative clinical rotations that compared students who took a perioperative clinical rotation to students who took other clinical rotations. The hypothesis was that perioperative students would demonstrate knowledge equal to or better than students who took other clinical rotations.
Sigsby said that most nursing students have limited exposure to surgical patients, in part because of the competition for clinical sites, surgical procedures moving to ambulatory settings, and shorter hospital stays. She also said many nursing faculty members do not accept OR rotations.
Students in the study experienced a typical clinical rotation that consisted of two days per week in a clinical setting for five to eight weeks. In fall 1998, of 138 students, 46 were placed in the perioperative group, and in fall 1999, of 142 students, 51 were placed in the perioperative group. Data were collected from students in the perioperative rotation and students in other types of clinical rotations. Both groups of students were tested in a number of different categories, including aseptic technique, skin integrity, medication administration, patient safety, infection control, patient positioning, informed consent, thermal regulation, and general health care.
Sigsby said the evaluation revealed that, statistically, perioperative students had more knowledge about health care issues. Data were not available to show whether these students actually went into perioperative nursing upon graduation, but Sigsby said she knew of several who had done so.
NIKKI PARKER
ASSOCIATE EDITOR
NANCY K. KUEHL
SENIOR EDITOR
COPYRIGHT 2003 Association of Operating Room Nurses, Inc.
COPYRIGHT 2003 Gale Group