Vogel T, Verreault R, Gourdeau M, et al. Optimal duration of antibiotic therapy for uncomplicated urinary tract infection in older women: a double-blind randomized controlled trial. CMAJ 2004:170:469-4 73.
* CLINICAL QUESTION
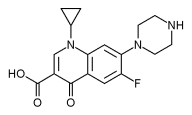
Is 3 days of ciprofloxacin as effective as 7 to 10 days of the same drug for older women with urinary tract infection?
* BOTTOM LINE
This reasonably large study found that 3 days of ciprofloxacin (Cipro) twice daily is as effective and better tolerated than 7 days of treatment for healthy older women with urinary tract infection (UTI). Although a much larger study might find a small difference in outcomes, it is unlikely to be clinically meaningful; this study was powered to detect a modest 10% difference in outcomes. (LOE=1b)
* STUDY DESIGN
Randomized controlled trial (double-blinded)
* SETTING
Outpatient (any)
* SYNOPSIS
We know that 3 days of antibiotics is effective for uncomplicated lower UTI in young healthy women. However, most physicians still use a longer course of 7 to 10 days for older women.
In this study, women aged >65 years with a positive urine culture and at least 1 symptom of UTI were randomized to receive either oral ciprofloxacin 250 mg twice daily for 3 days plus placebo for 4 days (n=93) or ciprofloxacin 250 mg twice daily for 7 days (n=89). Women with diabetes, an indwelling catheter, abnormal renal function, sepsis, recent use of antibiotics, or signs of pyelonephritis (not specified what they are) were excluded. Groups were similar at baseline, allocation was appropriately concealed, and analysis was by intention to treat. Patients were followed up for a total of 6 weeks.
Four patients withdrew from the 7-day group because of adverse events, compared with 1 in the 3-day group. There were 2 deaths in each group (the study included some hospitalized patients, since it was organized via a central laboratory). Most had Escherichia coli (71%), and 15.8% had Klebsiella pneumoniae. There was no difference between groups at 2 days after completion of antibiotic therapy regarding bacterial eradication (98% for the 3-day group vs 93% for the 7-day group) or symptom improvement (98% for the 3-day group vs 92% for the 7-day group). The same was true at 6 weeks, with similar rates of reinfection (14% vs 18%) and relapse (15% vs 13%). Adverse effects--drowsiness, loss of appetite, and nausea or vomiting, in particular--were more common in the 7-day group.
COPYRIGHT 2004 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group