Study objectives: To determine the effect of clarithromycin therapy in patients with asthma.
Design: Randomized, double blind, placebo-controlled trial.
Setting: A tertiary referral center.
Patients or participants: Fifty-five subjects with chronic, stable asthma recruited from the general Denver, CO, community.
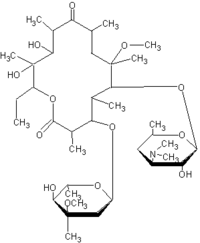
Interventions: Patients underwent airway evaluation for Mycoplasma pneumoniae and Chlamydia pneumoniae by polymerase chain reaction (PCR) and culture, followed by treatment with clarithromycin, 500 bid, or placebo for 6 weeks.
Measurements and results: Outcome variables were lung function, sinusitis as measured by CT, and the inflammatory mediators tumor necrosis factor (TNF)-[alpha], interleukin (IL)-2, IL-4, IL-5, and IL-12 messenger RNA (mRNA) measured via in situ hybridization, in airway biopsies, and BAL. Mycoplasma or chlamydia were detected by PCR in 31 of 55 asthmatics. Treatment resulted in a significant improvement in the FE[V.sub.1], but only in the PCR-positive subjects (2.50 [+ or -] 0.16 to 2.69 [+ or -] 0.19 L, mean [+ or -] SEM; p = 0.05). This was not appreciated in the PCR-negative subjects (2.59 [+ or -] 0.24 to 2.54 [+ or -] 0.18 L, p = 0.85) or the PCR-positive or PCR-negative subjects who received placebo. Sinus CTs revealed no change in sinusitis with clarithromycin treatment. In situ hybridization revealed no significant difference in baseline airway tissue or BAL-mediator expression between the PCR-positive and PCR-negative subjects. However, the PCR-positive subjects who received clarithromycin demonstrated a reduction in TNF-[alpha] (p = 0.006), IL-5 (p = 0.007), and IL-12 (p = 0.004) mRNA in BAL and TNF-[alpha] mRNA in airway tissue (p = 0.0009). The PCR-negative subjects who received clarithromycin only demonstrated a reduction in TNF-[alpha] (p = 0.01) and IL-12 (p = 0.002) mRNA in BAL and TNF-[alpha] mRNA in airway tissue (p = 0.004). There were no significant differences in cytokine expression in those subjects who received placebo.
Conclusions: These observations support the hypothesis that clarithromycin therapy improves lung function, but only in those subjects with positive PCR findings for M pneumoniae or C pneumoniae.
Key words: airway; asthma; bronchoscopy; chlamydia; mycoplasma
Abbreviations: IL = interleukin; IQ = interquartile range; mRNA = messenger RNA; PCR = polymerase chain reaction; TNF = tumor necrosis factor
**********
The role of infectious agents in chronic inflammatory disease processes has become an active area of investigation. There are data to suggest that infectious organisms, particularly the atypical bacteria, Chlamydia pneumoniae and Mycoplasma pneumoniae, may be involved in asthma pathogenesis. (1-14) Certainly there are considerable data implicating these organisms in the exacerbation of asthma. (12,15-22) We have previously reported the presence of M pneumoniae and C pneumoniae in the airways of chronic, stable asthmatics. (3,14) These organisms were present by polymerase chain reaction (PCR) in the upper and lower airways of patients with mild-to-moderate asthma.
The significance of these organisms is as yet unclear. It is not known whether these organisms were allowed to persist after an infection, or were present prior to the development of asthma. There is evidence to support both possibilities, as mycoplasma organisms have been shown to persist in the airways of guinea pigs for up to 160 days. (23) However, there was no clinical evidence of acute M pneumoniae or C pneumoniae infection for at least 3 months prior to study. (3,14) The observation that these organisms were present first and lead to the development of asthma is intriguing. There have been reports of patients presenting with acute infection by M pneumoniae or C pneumoniae, followed either by the development of asthma (2) or a significant improvement in lung function and asthma symptoms with antimicrobial therapy directed against these organisms. (6,12,13) In addition, the effects of infection with this organism can persist for months, resulting in decreased expiratory flow rates, and increased airway hyperresponsiveness in normal individuals. (24,25)
If M pneumoniae and C pneumoniae are causal factors in chronic asthma in certain individuals, then treatment with clarithromycin, a macrolide with known activity against mycoplasma and chlamydia species as well as anti-inflammatory effects, (26-28) would be expected to improve asthma. Given the presence of M pneumoniae and C pneumoniae in the lower airways as we have previously reported, we hypothesized that pulmonary function and airway inflammation would be improved in asthmatic patients after treatment with clarithromycin as compared to placebo. This report is an extension of our previous work. (3,14)
MATERIALS AND METHODS
Subjects
Fifty-five subjects were recruited via newspaper and radio advertisements from the general Denver, CO, community. The asthmatics fulfilled criteria for asthma, (29) exhibiting a provocative concentration of methacholine causing a 20% decline in FE[V.sub.1] of < 8 mg/mL, and reversibility of lung function by at least 12% with bronchodilator. Exclusion criteria included inpatient status; upper or lower respiratory tract infection within 3 months of study; use of macrolides, tetracyclines, or quinolones within 3 months of the study; smoking history > 5 pack-years or any cigarettes within the previous 2 years; and significant nonasthma pulmonary disease or other medical problems. No subject was a hospital worker to ensure that contact with potential patients with M pneumoniae infection was minimized. Subject characteristics are shown in Table 1, where subjects were considered of moderate severity by American Thoracic Society criteria. (29)
Study Protocol
Physiologic and Radiographic Evaluation: After informed consent was obtained for this institutional review board-approved protocol, all subjects underwent methacholine challenge and pulmonary function tests, including spirometry, lung volumes, and bronchodilator response. A chest radiograph was performed to rule out infiltrates consistent with acute mycoplasma pneumonia.
The extent of sinusitis was determined by quantitative evaluation of one CT image to determine the area of sinus tissue before and after therapy. Each image, which was a 3-mm-thick coronal cut at the level of the osteomeatal unit, was visually optimized before measurements were made by standard window and leveling techniques to maximize the contrast between the aerated sinuses and the surrounding mucosa. Initially, the entire sinus tissue and airway area was measured by utilizing a computerized image analysis software package (Osiris Medical Imaging Software, Version 3.6; University Hospital of Geneva; Geneva, Switzerland) to hand draw a region of interest around the entire sinus tissue and airway region on the CT image. This measurement yielded the sinus tissue plus airway area in millimeters squared. The osteomeatal complex was not included in this measurement. Secondly, the area within the sinus cavities (maxillary, ethmoid, and frontal), where density was equivalent to air, was measured by using a region-growing tool in the same computerized image analysis software package. This region-growing tool automatically measured the airway area by finding the boundary between the air and sinus tissue and calculating the area of the air-filled spaces. The air density area was subtracted from the total area to obtain the desired sinus tissue area in millimeters squared. One image was chosen, and the image at the same level was evaluated before and after treatment. The individual who performed the analysis was blinded to subjects' mycoplasma/chlamydia status.
Specimen Collection: Upper-airway and lower-airway specimens were collected and analyzed for M pneumoniae and C pneumoniae as previously described, (3,14) Nasal epithelial cells were obtained by placing a probe (Rhinoprobe; ASI; Arlington, TX) into the anterior nares. Oropharyngeal specimens were obtained from the posterior oropharynx with a wire-shafted Dacron swab (Dacroswab; Spectrum Laboratories; Houston, TX). Specimens from each site were placed and agitated in tubes of SP4 mycoplasma media for mycoplasma culture and PCR.
Subjects underwent bronchoscopy with endobronchial biopsy, endobronchial protected brushing, and BAL to obtain specimens for lower-airway evaluation as previously described. (3,14) The location of the biopsies was randomized to the right or left lower lobe, followed in the opposite lung by brushing of the lower lobe and BAL in the right middle lobe or lingula to ensure that biopsy, brushing, and lavage were done equally in the group as a whole. Prior to the bronchoscopy, spirometry was performed and asthmatics received 0.18 mg of inhaled albuterol. All subjects received 0.4 mg of atropine IV. Lidocaine (4%) was used to anesthetize the upper airway, and lidocaine (1%) was applied to the laryngeal area, trachea, and orifice of the right lower or left lower lobe bronchi via the bronchoscope. Four endobronchial biopsies were performed under direct visualization from the fourth-generation or fifth-generation airways. The brushing of the proximal airways was performed under direct visualization using a separate protected cytologic brush for each pass, with a total of nine passes performed. BAL was performed using five 60-mL aliquots of sterile nonbacteriostatic normal saline solution at 37[degrees]C and returned by gentle hand suction. The specimens were placed in SP4 transport media. Supplemental oxygen was administered throughout the procedure, along with monitoring of heart rate, BP, and oxygen saturation.
Microbiological Analysis: Culture for mycoplasma was performed as previously described. (3,14) Growth was monitored daily for approximately 8 weeks. For PCR analyses, we used multiple primer sets directed against organism-specific target sequences of either the P1 adhesion gene or the 16S ribosomal RNA gene of M pneumoniae, which can detect approximately 100 genomes. (30,31) A complete description of our technique can be found in the initial publication. (3) Under these conditions, although we found Mycoplasma genitalium and Mycoplasma fermentans, none of the primers reacted with any other mycoplasmas of human origin. Chlamydia cultures and PCR were performed as previously described. (32)
In Situ Hybridization: Airway tissue was placed in 4% ribonuclease-free paraformaldehyde, and then embedded in paraffin for in situ hybridization using [sup.35]S-labeled riboprobes as previously described. (33-35) BAL cytospins were prepared by removing 10 mL of whole BAL prior to the adherence step and resuspending BAL cells in phosphate-buffered saline solution at a concentration of 7.5 x [10.sup.5]/mL. Seventy-five microliters were placed in a Shandon cytocentrifuge tube and centrifuged at 1,000 revolutions per minute for 1 min. This technique resulted in a concentration approximately of 56,250 cells per slide. The slides were then fixed in methanol. [sup.35]S-uridine triphosphate-labeled RNA probes (antisense and sense) were prepared from complementary DNA for tumor necrosis factor (TNF)-[alpha], interleukin (IL)-2, IL-4, IL-5, and IL-12. To avoid nonspecific binding of [sup.35]S-labeled RNA probes, incubation with N-ethyl maleimide, iodoacetamide, and triethanolamine was included in prehybridization steps, and dithiothreitol (150 mM) was included in the hybridization mixture (Sigma Chemical; St. Louis, MO). As a negative control, preparations were hybridized with a sense TNF-[alpha], IL-2, IL-4, IL-5, IL-10, and IL-12 probes (having identical sequence to TNF-[alpha], IL-2, IL-4, IL-5, IL-10, and IL-12 messenger RNA [mRNA]). To further ensure the specificity of the signal, separate sets of preparations were pretreated with ribonuclease solution (Promega; Southampton, UK) prior to hybridization with antisense probe.
Counting was performed in a blinded fashion without knowledge of treatment status. Hybridization between cytokine mRNA and complementary RNA probes was identified as dense collections of silver grains overlying cells. Hybridization signals were assessed by counting mRNA-positive cells/1,000 total BAL cells on at least two slides for each cytokine probe, and counts were performed in duplicate. In tissue, biopsies were cut into 4-[micro]m sections. Two sections were evaluated for each cytokine probe. Hybridization signals were assessed by counting mRNA-positive cells per section, and the counts were performed in duplicate. The cytokines IL-2, IL-4, IL-5, and TNF-[alpha] were evaluated in tissue per the method described above. IL-10 and IL-12 were not evaluated due to reduced availability of tissue. For both tissue and BAL, the hybridization signal was considered to be specific when a positive signal was obtained with antisense probe, but not with the sense probe, and when the positive signal was abolished with the pretreatment with ribonuclease.
Randomization: Once the initial radiographic, physiologic, and bronchoscopic evaluations were completed, the asthmatic subjects were randomized to clarithromycin, 500 mg po bid, or placebo for 6 weeks in a double-blind fashion. Clarithromycin levels were measured in serum by high-pressure liquid chromatography at week 3, with therapeutic levels of 2 to 7 [micro]g/mL. The investigators remained blinded to these results until the end of the study. At the end of the treatment period (6 weeks), all subjects returned for repeat physiologic and bronchoscopic assessment as described above.
Statistical Analysis: The asthmatic subjects were compared for the presence or absence of mycoplasma or chlamydia infection (dichotomous variable) using Fisher exact test (36) as previously described. (3) Outcome variables in the treatment arm of the protocol (clarithromycin vs placebo) included the FE[V.sub.1], the change in FE[V.sub.1], FVC, and change in sinus area. Tissue variables included the number of positive cells per 1,000 for TNF-[alpha], IL-2, IL-4, IL-5, and IL-12 mRNA. The variables were compared using unpaired t test or Wilcoxon sign rank, depending on distribution of the data. Within-group comparisons were performed using the paired t test or Wilcoxon rank sum. Data are expressed as mean [+ or -] SEM or median (25th to 75th interquartile range [IQ]). For all analyses, all tests were two sided, and the level of significance was p [less than or equal to] 0.05.
RESULTS
Of fifty-five subjects recruited, 52 subjects were randomized to receive clarithromycin or placebo. Three subjects underwent analysis for mycoplasma and chlamydia, but were excluded from the treatment analysis due to scheduling difficulties (n = 1) and noncompliance (n = 2). On entry into the study, no chest radiographs revealed infiltrates. The mean clarithromycin level in the treatment group was 2.78 [+ or -] 0.31 [micro]g/mL.
PCR Results
As described (3,14) M pneumoniae or C pneumoniae were detected in 31 of 55 asthmatics by PCR. M pneumoniae was detected in 23 of 55 asthmatics, and M genitalium and M fermentans were detected in an additional two subjects, respectively. C pneumoniae was detected by PCR in 7 of 55 subjects. One subject had positive findings for both M pneumoniae and C pneumoniae All culture findings were negative for both organisms.
Treatment Arm Results, Physiology
Of the 52 asthmatics whose data were analyzed in the treatment arm of the protocol, 26 subjects were randomized to clarithromycin therapy and 26 subjects were randomized to placebo. In the placebo group, 13 subjects had positive PCR findings for either M pneumoniae or C pneumoniae and 13 subjects had negative PCR findings, Of the 26 subjects who received clarithromycin, 9 subjects had positive PCR findings at baseline and negative PCR findings after treatment, 5 subjects had positive PCR findings before and after treatment with clarithromycin, 9 subjects had negative PCR findings before and after treatment, and 2 subjects had positive PCR findings after treatment only.
When airway physiology was evaluated, there were no baseline differences in FE[V.sub.1] between PCR-positive and PCR-negative groups (percent predicted FE[V.sub.1], 68.1 [+ or -] 2.8% vs 69.0 [+ or -] 3.5%, respectively; p = 0.85). The baseline mean FE[V.sub.1] values in the placebo and clarithromycin groups were also not significantly different (2.72 [+ or -] 0.17 L vs 2.52 [+ or -] 0.13 L, respectively, p = 0.37). After treatment, lung function in the clarithromycin group was not significantly different from placebo (2.64 [+ or -] 0.14 vs 2.69 [+ or -] 0.16, respectively; p = 0.75). When subjects who received clarithromycin were compared by PCR status, the PCR-positive subjects exhibited a significant increase in FE[V.sub.1], where the mean FE[V.sub.1] increased from 2.50 [+ or -] 0.16 to 2.69 [+ or -] 0.19 L (p = 0.05; Fig 1). This significant increase was not appreciated in the PCR-negative subjects who received clarithromycin (FE[V.sub.1], 2.59 [+ or -] 0.24 to 2.54 [+ or -] 0.18 L, p = 0.85) or the PCR-positive or PCR-negative subjects who received placebo (p > 0.05). There were no significant changes in either treatment group in the FVC or lung volumes, regardless of PCR status.
[FIGURE 1 OMITTED]
Treatment Arm Results, In Situ Hybridization
In regard to cytokine expression, there was no difference in baseline expression of TNF-[alpha], IL-2, IL-4, IL-5 IL-10, and IL-12 mRNA between the PCR-positive and PCR-negative subjects. However, the PCR-positive subjects who received clarithromycin demonstrated a reduction in TNF-[alpha], IL-5, and IL-12 mRNA in BAL and TNF-[alpha] mRNA in airway tissue (Fig 2, 3). The PCR-positive subjects who received placebo demonstrated a reduction on BAL TNF-[alpha] mRNA, where expression decreased from 166 [+ or -] 9 to 122 [+ or -] 6 cells per 1,000 (p < 0.05). The PCR-negative subjects who received clarithromycin only demonstrated a reduction in TNF-[alpha] mRNA and IL-12 mRNA in BAL and TNF-[alpha] mRNA in airway tissue (Fig 4, 5). However, there was no significant change in cytokine expression in the PCR-negative subjects after placebo (data not shown). There was no difference in BAL IL-2, IL-4, and IL-10 mRNA expression or tissue IL-2, IL-4, IL-5, IL-10, and IL-12 mRNA expression in the PCR-positive and PCR-negative subjects after clarithromycin therapy (Figs 2-5). Thus, subjects who had positive PCR findings for mycoplasma or chlamydia exhibited reduced expression of IL-5 mRNA after clarithromycin therapy that was not observed in the PCR-negative subjects.
[FIGURES 2-5 OMITTED]
Treatment Arm Results, Sinus CT Evaluation
There was no significant difference in sinus disease at baseline between those subjects who received clarithromycin and those who received placebo (clarithromycin group median value, 1,571 [mm.sup.2] [IQ, 172 to 1,482 [mm.sup.2]], vs placebo median value, 1,701 [mm.sup.2] [IQ, 1496 to 1814 [mm.sup.2]]; p = 0.16). Clarithromycin treatment did not significantly alter the degree of sinus disease as illustrated by the change in sinus area with treatment (before/after treatment median value of 40 [mm.sup.2] [IQ, 128 to 513 [mm.sup.2]], vs placebo median value of 144 [mm.sup.2] [IQ, 37 to 400 [mm.sup.2]]; p = 0.64). In addition, clarithromycin treatment did not alter the degree of sinus disease, regardless of PCR status (before/after treatment PCR-positive median value of 111 [IQ, - 183 to 305], vs PCR-negative median value of 235 [IQ, 235 to 250]; p = 0.31).
DISCUSSION
This study illustrates that M pneumoniae or C pneumoniae are present in the airways by PCR in > 55% of the patients with chronic, stable asthma studied. In addition, treatment with clarithromycin improved the FE[V.sub.1] and reduced airway tissue expression of IL-5, but only in the PCR-positive subjects. There was no change in degree of sinus disease with clarithromycin.
The role of infectious agents in asthma has been shown in exacerbations, and there are now data suggesting a role in pathogenesis. (1-5,12,15-22) Yano et al (2) reported the development of asthma in an adult male subject following an episode of pneumonia secondary to M pneumoniae. This patient presented again to the health-care providers 1 month after pneumonia with reversible airway obstruction and bronchial hyperresponsiveness. He was treated with erythromycin, 1,200 mg/d, for 1 week, with improvement.
Mok and colleagues (37) also demonstrated an impairment in pulmonary function in 50 children with a previous history of M pneumoniae respiratory tract infection. These investigators measured large airway function via the FE[V.sub.1], vital capacity, and peak expiratory flow rate. Small airway function was determined by evaluating the change in maximum flow at 50% of vital capacity. When the patients with previous M pneumoniae infection were compared to healthy normal control subjects, the FE[V.sub.1], FVC, and peak expiratory flow rate were not significantly different, and all patients were asymptomatic. The maximum expiratory flow at 50% of vital capacity was significantly reduced in the group who had had the previous M pneumoniae infection and did not change with inhalation of a helium-oxygen mixture, suggesting small airway obstruction (p < 0.001). These tests were performed from 1.5 to 9.5 years after the infection, suggesting that M pneumoniae infection may impair pulmonary function despite lack of symptoms and underlying lung disease.
To further elucidate the mechanisms driving the association between mycoplasma and asthma, studies in a murine model have been undertaken. (38) In BALB/c mice, infection with M pneumoniae resulted in increased airway hyperresponsiveness as compared to saline solution control. (38) The increase in hyperresponsiveness was most pronounced on days 3, 7, and 14 after infection, and the associated lung pathology was primarily a neutrophilic infiltrate at day 3, followed by a reduction of neutrophils and an increase in macrophages by day 21. Interferon-[gamma], a T-helper type 1 cytokine, was suppressed at day 3 and day 7 compared with the saline solution-treated control, suggesting a T-helper type 2 response that was associated with hyperresponsiveness. Therefore, M pneumoniae infection may result in a T-helper type 2 predominant airway disease with hyperresponsiveness that mimics asthma in a murine model. Further studies are in progress to assess the interaction between M pneumoniae and allergen.
In regard to treatment, Hahn and Golubjatnikov (8) tested the hypothesis that treatment with an antibiotic with activity against C pneumoniae would significantly affect the natural history of the disease. (8) They treated 46 asthmatic patients with either doxycycline, 100 mg bid; azithromycin, 1,000 mg once weekly; or erythromycin, 1,000 mg/d, for a median period of 4 weeks. Pulmonary function and asthma symptoms were determined before and after treatment. Testing for a polyvalent antibody against C pneumoniae, which was a mixture of IgG, IgM, and IgA, was determined by microimmunofluorescence prior to treatment. Patients were considered eligible if they were seroreactive to C pneumoniae by exhibiting a titer against this polyvalent antibody of at least 1:16, were willing to accept prolonged empiric treatment with an antibiotic, and had no contraindication to prolonged antimicrobial administration. No restrictions were placed on medication use; 41% of subjects received inhaled corticosteroids, but the doses were not specified, and 41% used theophylline preparations. The mean pretreatment FE[V.sub.1] was 67.8% predicted, and increased by 12.5% after treatment (p = 0.003 compared to baseline). This study had no placebo group, and subjects received a wide variety of medications at varying doses. Thus, the validity of these results is uncertain.
In our study, mycoplasma and chlamydia organisms were still present in the airways of seven asthmatic subjects after treatment with clarithromycin, and two subjects had positive PCR findings after treatment only. A possible mechanism is that the organism is difficult to eradicate, as macrolides are bacteriostatic, which may result in a chronic state of infection/colonization. (39) Clarithromycin may have decreased the organism burden, which could not be evaluated by the PCR methods currently available to detect M pneumoniae and C pneumoniae. Additionally, M pneumoniae infection is known to be nonuniform in the airway, which may explain why two subjects had positive findings after therapy only despite extensive sampling of the lower airway. (23) However, clarithromycin may also act as an anti-inflammatory agent, as macrolides have been shown to exhibit anti-inflammatory actions on neutrophils and lymphocytes. (26,27) Amasayu and colleagues (40) showed in patients with mild-to-moderate asthma that 8 weeks of clarithromycin, 200 mg bid, improved asthma symptoms, and decreased sputum eosinophils and serum eosinophil cationic protein. There were also modest improvements in bronchial hyperresponsiveness. Additionally, Konno et al (41) showed that macrolides decreased pulmonary expression of TNF-[alpha], IL-3, IL-4, and IL-5 in a murine model. Macrolides have also been shown to decrease mucus production and bronchial hyperresponsiveness in vitro. (42,43) In our study, clarithromycin did not affect sinus disease significantly; thus, it may affect the airways directly. As a therapeutic agent, clarithromycin has been shown to exert a glucocorticoid sparing effect, as shown by Garey et al (44) in patients with severe, steroid-dependent asthma. In their report of three patients, two of three patients were able to discontinue prednisone after 12 months of clarithromycin, 500 mg bid The third patient was able to taper prednisone to 5 mg/d. There is controversy about whether clarithromycin alters the metabolism of glucocorticoids, as suggested by Black (45) but not supported by Fost et al. (46) Further studies are needed to conclusively evaluate the mechanism of clarithromycin in the treatment of asthma.
We have demonstrated that asthmatic subjects exhibit evidence of M pneumoniae and C pneumoniae colonization/infection exhibit an improvement in their FE[V.sub.1] with the antimicrobial and anti-inflammatory therapy, clarithromycin. This improvement was not mediated via improvement in sinus disease. Nor was this improvement seen in patients who received clarithromycin, but had negative findings for mycoplasma or chlamydia. Further study is needed to assess if the presence of M pneumoniae or C pneumoniae is an epiphenomenon or, as we expect, a pathogenic mechanism in asthma. If the latter is correct, the therapeutic armamentarium in asthma may include antibiotic therapy in selected patients.
ACKNOWLEDGMENT: We gratefully acknowledge the technical assistance of L. Duffy, G. Gambil, J. Glass, and E. Keyser at the University of Alabama at Birmingham; C. Gaydos at Johns Hopkins University; B. Marmion at the Institute of Medical and Veterinary Science, University of Adelaide, Australia; J. Pak and J. Henson at the National Jewish Medical and Research Center, Denver, CO; and the General Clinical Research Center at National Jewish Medical and Research Center and the University of Colorado Health Sciences Center.
REFERENCES
(1) Tipirneni P, Moore BS, Hyde JS, et al. IgE antibodies to Mycoplasma pneumoniae in asthma and other atopic diseases. Ann Allergy 1980; 45:1-7
(2) Yano T, Ichikawa Y, Komatu S, et al. Association of Mycoplasma pneumoniae antigen with initial onset of bronchial asthma. Am J Respir Crit Care Med 1994; 149:1348-1353
(3) Kraft M, Cassell GH, Henson JE, et al. Detection of Mycoplasma pneumoniae in the airways of adults with chronic asthma. Am J Respir Crit Care Med 1998; 158:998-1001
(4) Melbye H, Kongerud J, Vorland L. Reversible airflow limitation in adults with respiratory infection. Eur Respir J 1994; 7:1239-1245
(5) Hahn DL, Dodge RW, Golubjatnikov R. Association of Chlamydia pneumoniae (strain TWAR) infection with wheezing, asthmatic bronchitis, and adult-onset asthma. JAMA 1991; 266:225-230
(6) Hahn DL, McDonald R. Can acute Chlamydia pneumoniae respiratory tract infection initiate chronic asthma? Ann Allergy Asthma Immunol 1998; 81:339-344
(7) Hahn DL, Bukstein D, Luskin A, et al. Evidence for Chlamydia pneumoniae infection in steroid-dependent asthma. Ann Allergy Asthma Immunol 1998; 80:45-49
(8) Hahn DL, Golubjatnikov R. Asthma and chlamydial infection: a case series. J Fam Pract 1994; 38:589-595
(9) Hahn DL. Treatment of Chlamydia pneumoniae infection in adult asthma: a before-after trial. J Fam Pract 1995; 41:345-351
(10) Cook PJ, Davies P, Tunnicliffe W, et al. Chlamydia pneumoniae and asthma. Thorax 1998; 53:254-259
(11) Von Hertzen L, Toyryla M, Gimishanov A, et al. Asthma, atopy and Chlamydia pneumoniae antibodies in adults. Clin Exp Allergy 1998; 29:522-528
(12) Emre U, Roblin PM, Gelling M, et al. The association of Chlamydia pneumoniae infection and reactive airway disease in children. Arch Pediatr Adolesc Med 1994; 148:727-732
(13) Emre U, Sokolovskaya N, Roblin PM, et al. Detection of anti-chlamydia pneumoniae IgE in children with reactive airway disease. J Infect Dis 1995; 172:265-267
(14) Martin R, Kraft M, Chu H, et al. A link between infection and asthma. J All Clin Immunol 2001; 107:595-601
(15) Seggev JS, Lis I, Siman-Tov S, et al. Mycoplasma pneumoniae is a frequent cause of exacerbation of bronchial asthma in adults. Ann Allergy 1986; 57:262-265
(16) Berkovich S, Millian SJ, Snyder RD. The association of viral and mycoplasma infections with recurrence of wheezing in the asthmatic child. Ann Allergy 1970; 28:43-49
(17) Kondo S, Ito M, Saito M, et al. Progressive bronchial obstruction during the acute state of respiratory tract infection in asthmatic children. Chest 1994; 106:100-104
(18) Gil JS, Cedillo RL, Mayagoitia BG, et al. Isolation of Mycoplasma pneumoniae from asthmatic patients. Ann Allergy 1993; 70:23-25
(19) Huhti E, Terttu M, Nikosekelainen J, et al. Association of viral and mycoplasma infections with exacerbations of asthma. Ann Allergy 1974; 33:145-149
(20) Cunningham AF, Johnston SL, Julious SA, et al. Chronic Chlamydia pneumoniae infection and asthma exacerbations in children. Eur Respir J 1998; 11:345-349
(21) Allegra L, Blasi F, Centanni S, et al. Acute exacerbations of asthma in adults: role of Chlamydia pneumoniae infection. Eur Respir J 1994; 7:2165-2168
(22) Hahn DL, Anttila T, Saikku P. Association of Chlamydia pneumoniae IgA antibodies with recently symptomatic asthma. Epidemiol Infect 1996; 117:513-517
(23) Marmion BP, Williamson J, Worswick PA, et al. Experience with newer techniques for the laboratory detection of Mycoplasma pneumoniae infection: Adelaide, 1978-1991. Clin Infect Dis 1993; 17:S90-S99
(24) Sabato AR, Martin AJ, Marmion BP, et al. Mycoplasma pneumoniae: acute illness, antibiotics, and subsequent pulmonary function. Arch Dis Child 1984; 59:1034-1037
(25) Shimuzu T, Mochizuki H, Kato M, et al. Immunoglobulin levels, number of eosinophils in the peripheral blood and bronchial hypersensitivity in children with Mycoplasma pneumoniae pneumonia. Jpn J Allergol 1991; 40:21-27
(26) Greos LS, Surs W, Szefler SJ, et al. Macrolide antibiotics inhibit neutrophil chemotaxis [abstract]. J Allergy Clin Immunol 1990; 85:195
(27) Alvarez J, Szefler SJ, Gelfand EW. Troleandomycin (TAO) therapy modies the T-lymphocyte response to glucocorticoids in asthmatics [abstract]. J Allergy Clin Immunol 1990; 85:195
(28) Schlossberg D. Azithromycin and clarithromycin. Med Clin North Am 1995; 79:803-815
(29) American Thoracic Society Board of Directors. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD). Am Rev Respir Dis 1987; 136:225-244
(30) Williamson J, Marmion B, Worswick D, et al. Laboratory diagnosis of Mycoplasma pneumoniae infection: 4. Comparison of antigen detection of M Pneumoniae in respiratory isolates. Epidemiol Infect 1992; 109:519-537
(31) Williamson J, Marmion BP, Kok T, et al. Confirmation of fatal Mycoplasma pneumoniae infection by polymerase chain reaction detection of adhesin gene in fixed lung tissue [letter]. J Infect Dis 1994; 170:1052-1053
(32) Gaydos CA, Roablin PM, Hammerschlag MR, et al. Diagnostic utility of PCR-enzyme immunoassay, culture and serology for detection of Chlamydia pneumoniae in symptomatic and asymptomatic patients. J Clin Microbiol 1994; 32:903-905
(33) Robinson DS, Harold Q, Ying S, et al. Predominant TH2-type bronchoalveolar lavage T-lymphocyte activation in atopic asthma. N Engl J Med 1992; 326:298-304
(34) Hamid Q, Wharton J, Terenghi G, et al. Localization of natriuretic peptic mRNA and immunoreactivity in rat heart and human arterial appendage. Proc Natl Acad Sci U S A 1987; 84:6760-6764
(35) Hamid Q, Azzawi M, Ying S, et al. Expression of mRNA for interleukin-5 in mucosal bronchial biopsies from asthma. J Clin Invest 1991; 87:1541-1546
(36) Sokal RR, Rohlf FJ. Biometry. 2nd ed. New York, NY: W.H. Freeman and Company; 1981; 704-721
(37) Mok JYQ, Waugh PR, Simpson H. Mycoplasma pneumoniae infection: a follow up study of 50 children with respiratory illness. Arch Dis Child 1979; 54:506-511
(38) Martin RJ, Chu HW, Honour JM, et al. Airway inflammation and bronchial hyperresponsiveness after Mycoplasma pneumoniae infection in a murine model. Am J Respir Cell Mol Biol 2001 24:577-582
(39) Luby JP. Pneumonia caused by Mycoplasma pneumoniae. J Infect Dis 1991; 135:673-677
(40) Amayasu H, Yoshida S, Ebana S, et al. Clarithromycin suppresses bronchial hyperresponsiveness associated with eosinophilic inflammation in patients with asthma. Ann Allergy Asthma Immunol 2000; 84:594-598
(41) Konno S, Asano K, Kurokawa M, et al. Antiasthmatic activity of a macrolide antibiotic, roxithromycin: analysis of possible mechanism in vitro and in vivo. Int Arch Allergy Immunol 1994; 105:308-316
(42) Goswami SK, Kivity S, Marom Z. Erythromycin inhibits respiratory glycoconjugate secretion from human airways in vitro. Am Rev Respir Dis 1990; 141:72-78
(43) Miyatake H, Taki F, Taniguchi H, et al. Erythromycin reduces the severity of bronchial hyperresponsiveness in asthma. Chest 1991; 99:670-673
(44) Garey K, Rubinstein I, Gotfried M, et al. Long term clarithromycin decreases prednisone requirements in elderly patients with prednisone dependent asthma. Chest 2000; 118:1826-1827
(45) Black P. The use of macrolides in the treatment of asthma. Eur Respir Rev 1996; 38:240-243
(46) Fost D, Leung D, Martin R, et al. Inhibition of methylprednisolone elimination in the presence of clarithromycin therapy. J Allergy Clin Immunol 1999; 103:1031-1035
* From the Department of Medicine (Drs. Kraft and Martin, and Mr. Pak), National Jewish Medical and Research Center and the University of Colorado Health Sciences Center, Denver, CO; and Department of Microbiology (Dr. Cassell), University of Alabama at Birmingham, Birmingham, AL.
Supported by the American Lung Association Asthma Research Center Grant and Abbott Laboratories.
Manuscript received July 10, 2001; revision accepted December 12, 2001.
Correspondence to: Richard J. Martin, MD, FCCP, National Jewish Medical and Research Center, 1400 Jackson St, Room J115, Denver, CO 80206; e-mail: martinr@njc.org
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group