Abstract
Telithromycin (HMR 3647) is a new ketolide antimicrobial that was developed for the treatment of community-acquired respiratory truer infections. We conducted a randomized, double-blind, multicenter study to compare the clinical efficacy and safety of oral telithromycin, at 800 mg once daily for 5 or 10 days, with that of amoxicillin/ clavulanic acid, at 500/125 mg three times daily for 10 days, in adults with acute maxillary sinusitis (AMS). A total of 754 patients with AMS of less than 28 days' duration were randomized to receive either telithromycin for 5 days followed by placebo for 5 days, telithromycin for 10 days, or amoxicillin/clavulanic acid for 10 days. Clinical outcome was assessed at a test-of-cure (TOC) visit between days 17 and 24 and at a late post-therapy visit between days 31 and 45. Analysis of clinical outcome on a per-protocol basis (n = 434) demonstrated therapeutic equivalence among the three regimens at the TOC visit; in each treatment group, the clinical cure rate was approximately 75%. Only a few patients (3 to 5 in each group) had relapsed by the late post-therapy follow-up visit. Telithromycin was generally safe and well tolerated. The most common adverse events were mild or moderate gastrointestinal effects, which occurred with similar frequency in all three groups. We conclude that 5 or 10 days of telithromycin at 800 mg once daily is as effective clinically and as well tolerated as 10 days of treatment with amoxicillin/clavulanic acid. Telithromycin, therefore, appears to be a valuable option for the treatment of AMS.
Introduction
Sinusitis is one of the most prevalent diseases encountered in general practice. (1) Estimated to affect more than 30 million people annually in the United States, (2) sinusitis is responsible for approximately 16 million physician office visits per year. (3) Its actual prevalence is probably higher because its major symptoms--facial pain, purulent nasal discharge, headache, and fever--are difficult to distinguish from those of the common cold or allergies, for which patients often do not consult a physician.
In patients with bacterial sinusitis, Streptococcus pneumoniae and Hemophilus influenzae account for approximately 70% of bacterial isolates. (4) Less frequently implicated pathogens include Moraxella catarrhalis, Streptococcus pyogenes, and staphylococci, which are often found in cases of chronic or recurrent sinusitis. (4,5) Early treatment with an antimicrobial is warranted to reduce the duration and severity of symptoms, eradicate causative pathogens, and prevent the development of permanent mucosal damage, chronic sinusitis, and rarer complications, such as optic neuritis, subdural abscess, and meningitis. (6)
Antral sinus puncture with culture remains the gold standard for the diagnosis of acute bacterial sinusitis, but this procedure is rarely performed in general practice. Instead, antibacterial therapy is usually initiated empirically with an agent that is active against likely pathogens. However, a major concern with empiric treatment is an increase in antibacterial resistance among key pathogens. For example, penicillin resistance occurs in more than 40% of S pneumoniae strains in many regions; many of these strains are also resistant to macrolide antibiotics. (7) Therefore, selecting an agent that retains activity against resistant strains is important in treating sinusitis.
The usual duration of oral antibacterial therapy is 10 days, and efforts have been made to develop shorterduration antibacterial regimens that have the potential to improve patient compliance, thus minimizing the risk of treatment failure and possibly decreasing resistance. (8) The effectiveness of a shorter treatment regimen depends on the intrinsic properties of the antibacterial--primarily its potency, elimination half-life, and tissue diffusion.
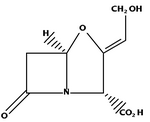
Telithromycin (HMR 3647), a ketolide, has a targeted spectrum of activity that covers the common pathogens seen in acute bacterial sinusitis--specifically, beta-lactamase-producing H influenzae and M catarrhalis and penicillin G- and erythromycin A-resistant S pneumoniae. (9-13) The pharmacokinetic profile of oral telithromycin supports a convenient 800-mg once-daily regimen. At this dosage, telithromycin is rapidly absorbed and has a long terminal-phase elimination half-life (~10 hr). When used against common respiratory pathogens, it has a high "area under the plasma concentration--time curve" to minimum inhibitory concentration ratio (AUC:MIC ratio). (14) Moreover, telithromycin concentrates in white blood cells, which suggests that it has longlasting antibacterial activity in tissues and penetrates into otorhinolaryngologic tissue. (15) All these characteristics make telithromycin an attractive option for the short-term treatment of acute maxillary sinusitis (AMS).
In this article, we describe our comparison of the efficacy and safety of 5- and 10-day courses of telithromycin with that of a standard 10-day regimen of amoxicillin/clavulanic acid in the treatment of AMS.
Patients and methods
This randomized, double-blind, three-arm, parallel-group, multicenter trial was conducted between July 17, 1998, and June 16, 1999, at 69 centers in the United States (51 centers), Canada (11), South Africa (3), Argentina (2), and Chile (2). The study was conducted in accordance with good clinical practice and ethical principles as set forth in the latest revisions to the Declaration of Helsinki; the clinical protocol was approved by an independent ethics committee or institutional review board in each country. All patients provided written informed consent prior to the initiation of study-related procedures.
Inclusion and exclusion criteria. Patients aged 18 years or older with presumed AMS (i.e., purulent nasal discharge visualized in the middle meatus or postnasal discharge; maxillary tenderness; toothache or pain on percussion; facial pain, pressure, or tightness; or nasal congestion that responded poorly to nasal decongestants) were screened for enrollment. To be eligible for the study, patients had to have exhibited clinical symptoms of AMS (that did not require immediate surgery) for fewer than 28 days and evidence of infection on maxillary sinus x-ray (presence of an air-fluid level and/or total sinus opacity and/or [greater than or equal to] 6 mm of mucosal thickening) within 48 hours of study inclusion.
Exclusion criteria included a history of chronic or recurrent sinusitis or the presence of sphenoid sinusitis, nosocomially acquired sinusitis, obstructive anatomic lesions in the nasopharynx, suspected nonbacterial infection, documented resistant pathogens, immotile cilia syndrome, cystic fibrosis, or odontogenic infection. Patients were excluded if they had taken an antibacterial within the previous 7 days. Also excluded were immunocompromised patients, patients who had a known hypersensitivity to a macrolide or beta-lactam antibiotic, and patients who were taking a corticosteroid or any drug that could interfere with the efficacy and safety assessments of the study medications. Further exclusion criteria included progressively fatal illness, long Q-T syndrome, severe hypokalemia, a history of drug or alcohol abuse, renal or hepatic impairment, and lactation or pregnancy.
Study procedures and medications. Patients attended their respective study clinics on five separate occasions. On the first visit (day 1), patients underwent evaluation of AMS-related signs and symptoms, sinus x-rays from three separate views, a physical examination (including vital signs), 12-lead electrocardiography (ECG), and collection of blood and urine for routine laboratory safety testing. At selected study sites, sinus puncture and aspiration of sinus fluid were undertaken in some patients who had a confirmed diagnosis of AMS; subsequent in vitro culture and antibacterial susceptibility testing were performed at a local accredited laboratory. All isolates were submitted to a central laboratory (Clinical Microbiology Institute; Wilsonville, Ore.) for confirmatory susceptibility testing by disk diffusion and MIC determinations.
Patients were randomized (1:1:1) to one of three oral treatment groups: 800 mg of telithromyein once in the morning for 5 days, 800 mg of telithromycin once in the morning for 10 days, or 500/125 mg of amoxicillin/ clavulanic acid three times daily for 10 days. The identity of all study drugs was concealed by placing them in identical opaque capsules. Each dose of amoxicillin/ clavulanic acid was administered as two capsules; one contained 250 mg of amoxicillin and 125 mg of clavulanic acid and the other contained 250 mg of amoxicillin. To further ensure the maintenance of the double-blind conditions, patients in both telithromycin groups also received matching placebo capsules at midday and in the evening, and those who had been randomized to the 5-day group received matching placebo capsules (morning, midday, and evening) for 5 days after the completion of their active treatment.
Patients were re-evaluated for infection-related signs and symptoms during an on-therapy visit between days 3 and 5 and during three post-therapy visits between days 11 and 13 (end-of-therapy visit), between days 17 and 24 (test-of-cure [TOC] visit), and between days 31 and d (]ate post-therapy visit). All patients underwent repeat sinus x-rays at the TOC visit as part of the assessment clinical outcome; additional x-rays were performed during other clinical visits for patients whose symptoms had worsened or who had required additional antibacterial therapy. When indicated by clinical failure, additional sinus punctures were performed to determine bacteriologic outcome. At the end-of-therapy and/or the TOC visits, patients underwent further blood and urine sampling, physical examination, measurement of vital signs, and 12-lead ECG. Compliance was assessed by counting unused capsules at the on-therapy and end-of-therapy visits.
Evaluation of clinical and bacteriologic efficacy. The primary efficacy variable was clinical outcome at the TOC visit in the clinical per-protocol patient population (i.e., patients who met diagnostic criteria, who received least one dose of study medication, and who were not major protocol violators). Determinations of clinical outcome were based on investigator assessments of signs and symptoms of AMS and the degree of radiologic changes on repeat x-ray. Cure was defined as (1) disappearance of infection, clinical improvement, or a return to the preinfection state with regard to all AMS-related signs and symptoms without a need for subsequent antibacterial therapy and (2) sinus x-ray findings that were normal, improved, or at least not worse. Patients whose signs and symptoms were unchanged or worse (with or without worsening on sinus x-ray) and who needed subsequent antibacterial therapy were classified as treatment failures.
Secondary efficacy variables included clinical outcome at the late post-therapy visit and bacteriologic outcome at the TOC and late post-therapy visits. Clinical cure at the late post-therapy visit was declared for those patients who had been clinically cured at the TOC visit and who did not subsequently develop signs and symptoms of new infection and who did not need further antibacterial therapy for AMS or related complication: Patients who were designated clinical failures at the TOC visit were carried forward to the late post-therapy assessment. Other clinical failures included patients who had relapsed between the TOC and late post-therapy visits an thus required additional antibacterial treatment.
For patients in whom a causative bacterial pathogen had been isolated at screening, bacteriologic outcome was rate as either satisfactory, unsatisfactory, or indeterminate.
* A satisfactory outcome was declared when (1) the causative pathogen was documented to be eradicated on repeat sinus sampling or (2) eradication was presumed in patients whose degree of clinical recovery obviated tit need for follow-up sampling. Those patients in whom bacterial strain other than the primary causative pathogen was isolated (colonization) were also considered to have achieved a satisfactory outcome in the absence of signs and symptoms of active infection.
* Bacteriologic outcome was considered to be unsatisfactory when the causative pathogen persisted on repeat sinus sampling or was presumed to be persistent because of a need to initiate treatment with another antibacterial in the wake of clinical failure or worsening radiologic findings. Bacteriologic failure was also declared in patients who experienced superinfection or reinfection in 3 days or less after the completion of treatment in conjunction with the emergence of clinical and laboratory evidence of infection and a recurrence of the causative pathogen after it had been confirmed or presumed to be eradicated during earlier assessments.
* An indeterminate outcome was declared when circumstances did not allow for a clear classification of cure or failure. Factors that had an influence on this designation included a missed appointment, discontinuation of at the study medication for reasons not related to the medication itself; or the administration of another antimicrobial for an infection other than sinusitis.
Evaluation of safety and tolerability. Safety was evaluated by analyzing adverse events, laboratory data, ECG recordings, and physical examination findings, including vital signs. All adverse events that emerged or worsened during the study were recorded and evaluated in terms of intensity and causality.
Statistical analysis. The primary objective of this study was to obtain evidence of the clinical equivalence, on a at per-protocol basis at the TOC visit, of 5 and 10 days of telithromycin therapy with 10 days of amoxicillin/ clavulanic acid. In order to demonstrate equivalence, between-group comparisons were made in terms of the two-sided 95% confidence interval (CI) for the difference in cure rates; treatments were considered equivalent if the lower limit of the CI was--15% or greater and the upper it limit crossed 0. The limits of the two-sided 95% CI for between-group differences were based on an expected cure rate of 85%.
In order to achieve 90% power, our study required a minimum of 120 patients per group. Based on an assumption that 70% of all patients would be evaluable for clinical efficacy, we calculated that our population would have to include no fewer than 516 patients.
Once the study was under way, routine stability testing of the amoxicillin/clavulanic acid supply detected evidence that some of the samples in one batch had degraded. Therefore, the efficacy data on all patients who had received amoxicillin/clavulanic acid from this batch were declared invalid. As a result, 100 patients were unblinded and excluded from the study. A new population of patients was recruited and randomized to take their place, and the study resumed as planned.
Appropriate parametric and nonparametric tests were used to analyze between-group differences for continuous and categorical variables, respectively.
Results
Of the 754 patients who were randomized in the study, 753 received at least one dose of study medication. A total of 146 patients were excluded from the clinical efficacy analysis because their x-ray findings were not consistent with a diagnosis of AMS and/or they had received degraded medication. The modified intent-to-treat population, then, was made up of 607 patients, aged 16 to 84 years (median: 39), who had a confirmed diagnosis of AMS and who received at least one dose of study medication.
Overall, baseline demographics and disease characteristics were comparable in the three treatment groups, and no significant between-group differences were apparent (table 1). Analysis of infection characteristics showed that 222 patients (36.6%) had experienced at least one episode of AMS within the previous 12 months, with most having undergone one to three courses of antibacterial therapy during that time. Their current episode of AMS was generally of moderate intensity, and in most patients the infection had been present for 7 days or longer prior to enrollment. Only 10 patients (1.6%) were feverish. As a reflection of the relatively young age of the study population, only 28 patients (4.6%) had one or more general risk factors for morbidity; the most common were diabetes mellitus and unspecified liver disease (14 and 7 patients, respectively). The use of concomitant medication such as analgesics, anti-inflammatory agents, and cough and cold preparations was similar and well balanced in the three groups.
At study's end, 423 patients were clinically evaluable on a per-protocol basis (5-day telithromycin: n = 146; 10 day telithromycin: n = 140; amoxicillin/clavulanic acid: n = 137); 184 patients were excluded from analysis because of major protocol violations (primarily an insufficient duration of treatment, an incorrect diagnosis, or missing post-treatment information). The baseline characteristics of the clinical per-protocol population, their mean active treatment durations, and the number of active doses per patient were similar among the three groups and comparable with those of the modified intent-to-treat population (data not shown). Counts of returned study medication showed that more than 90% of patients in each group took at least 70% of their doses during the study.
Clinical outcome. Analysis of clinical outcome on a per-protocol basis (primary efficacy analysis) showed therapeutic equivalence between the two telithromycin regimens and the amoxicillin/clavulanic acid regimen at the TOC visit; each treatment achieved clinical cure in approximately 75% of patients (table 2). The classification of patients with an indeterminate outcome as clinical failures in this analysis (5-day telithromyein: n = 14; 10-day telithromycin: n = 14; amoxicillin/clavulanic acid: n = 20) meant that cure rates were slightly lower relative to the per-protocol analysis, from which such patients were excluded.
As was the case at the TOC visit, per-protocol clinical cure rates at the late post-therapy visit were similar in the three groups--approximately 70% in each (table 2). By the time of this visit, only a small number of patients had experienced a relapse. Analysis of the 95% CIs for between-group differences demonstrated the therapeutic equivalence of the two telithromycin regimens relative to amoxicillin/clavulanic acid therapy.
Clinical outcome according to demographic and infection characteristics. Subgroup analyses of clinical outcome at the TOC visit according to demographic and infection characteristics yielded comparable findings in the three groups, although the number of evaluable patients in some subgroups was small. Gender, age, and smoking status had no clinically relevant relationship to outcome in any group. Similar findings were observed when clinical outcome was analyzed according to current infection characteristics, including baseline x-ray findings (table 3).
Causative pathogens and susceptibility. Because sinus punctures were performed in only a small subset of patients, the number who were evaluable for bacteriologic outcome was likewise small. In all, 33 causative pathogens were isolated in 29 patients. The most common were S pneumoniae and H influenzae, which together accounted for 54.5% of the total number of pathogens. Other isolated pathogens included Hemophilus parainfluenzae and M catarrhalis. No patient had either S pyogenes or Staphylococcus aureus. Among those who did undergo sinus puncture, clinical cure rates were 85.7%, 85.7%, and 80.0% for the 5-day telithromycin, 10-day telithromycin, and amoxicillin/clavulanic acid groups, respectively (per-protocol data).
Susceptibility testing by disk diffusion methodology showed that no major respiratory pathogen (i.e., S pneumoniae and H influenzae) was resistant to study medication prior to treatment. Distribution of causative pathogens was comparable across the treatment groups, and similar findings (in terms of the profile and distribution of causative pathogens) were observed for the bacteriologically evaluable per-protocol population.
Bacteriologic outcome. A satisfactory bacteriologic outcome was obtained in six of seven patients in each telithromycin group and in eight of 10 patients in the amoxicillin/clavulanic acid group at the TOC evaluation. At the late post-therapy evaluation, the bacteriologic outcome was satisfactory in five of seven patients in all three groups (per-protocol population). There were no cases of recurrence, reinfection, or superinfection.
Bacteriologic outcome by pathogen and resistance profile. Analysis of bacteriologic outcome by pathogen at TOC in the per-protocol population revealed that all isolates of S pneumoniae and H influenzae were eradicated (or presumed to be eradicated) following both 5-and 10-day therapy with telithromycin (table 4). This included two Spneumoniae isolates with reduced susceptibility to penicillin G (MIC [greater than or equal to] 0.12 rag/L), one of which also had erythromycin A resistance, and three betalactamase-positive H influenzae isolates. All patients infected with these pathogens achieved clinical cure during telithromycin therapy, but amoxicillin/clavulanic acid failed to eradicate two of four isolates of S pneumoniae, despite the fact that all isolates were susceptible to penicillin G in vitro. Both patients with presumed persistence of S pneumoniae were clinical failures. Presumed persistence was recorded for one isolate of Pseudomonas aeruginosa (a pathogen outside the spectrum of telithromycin) in the telithromycin 5-day group and one isolate of Streptococcus bovis in the telithromycin 10-day group (susceptible to telithromycin); both patients failed to achieve clinical cure.
Safety and tolerability. All patients who received at least one dose of study medication, except those who did not undergo a pretherapy entry assessment (n = 10), were included in the safety analysis (5-day telithromycin: n = 244; 10-day telithromycin: n = 254; amoxicillin/ clavulanic acid: n = 245). Overall, 327 patients (44.0%) experienced one or more treatment-emergent adverse events that were considered to be possibly related to a study medication during the study (5-day telithromyein: n = 103 [42.2%]; 10-day telithromycin: n = 119 [46.9%]; amoxicillin/clavulanic acid: n = 105 [42.9%]). Diarrhea and nausea were the most common adverse events in each treatment group (table 5). With the exception of vaginal candidiasis, which occurred less frequently in the 5-day telithromycin group than in the amoxicillin/clavulanic acid group, there were no significant differences among the three treatment groups in terms of the frequency of adverse events.
A total of 41 patients (5.5%) withdrew from the study because of adverse events that were considered to be possibly drug related (5-day telithromycin: n = 16 [6.6%]; 10-day telithromycin: n = 14 [5.5%]; amoxicillin/ clavulanic acid: n = 11 [4.5%]). Seven patients (1.0%) experienced at least one serious treatment-emergent adverse event during the study; adverse events in four of these patients were considered to be possibly related to the study medication by an investigator--three in the 10-day telithromycin group (allergy, gastroenteritis, and pseudomembranous colitis [one patient each]) and one in the amoxicillin/clavulanic acid group (pseudomembranous colitis; the patient recovered without sequelae following treatment with metronidazole). No deaths occurred during the study.
Analysis of ECG recordings showed that mean changes in the Q-Tc interval were small and within the limits of normal variability in each group, and no patient met the clinically noteworthy criterion of a Q-Tc interval of 500 or more msec. No clinically relevant between-group differences were apparent for changes in vital signs or laboratory safety data, including transaminase levels.
Discussion
Over the past 3 decades, the susceptibility to antibiotics of many bacterial species implicated in acute bacterial sinusitis has declined dramatically. (16) This development has complicated the selection of suitable empiric antibiotic therapy for this condition. Indeed, in the United States, almost all M catarrhalis and at least 33% of H influenzae isolates produce beta-lactamase, which undermines the empiric use of beta-lactamase-susceptible drugs such as amoxicillin. (17) As a result, amoxicillin/clavulanic acid and newer macrolides have gained wider acceptance in recent years as potential first-line agents for acute sinusitis. However, penicillin G resistance in the other major bacterial sinusitis pathogen, S pneumoniae, has also reached alarming levels; because this resistance mechanism involves the alteration of penicillin-binding proteins, these isolates also show decreased susceptibility to amoxicillin/clavulanic acid. (17) Furthermore, more than 50% of penicillin G-resistant isolates are also reported to be resistant to macrolides, and the overall levels of macrolide resistance among S pneumoniae isolates are now thought to exceed those of penicillin resistance in many regions. (7,13) These findings highlight the need for effective new antibacterials that have activity against the spectrum of sinusitis bacterial pathogens, including resistant strains, and that have a low potential for further selection of resistant isolates.
Our study shows that treatment with telithromycin at 800 mg once daily for 5 or 10 days is as clinically effective as a 10-day course of amoxicillin/clavulanic acid for the treatment of adults with AMS. Resolution of both clinical symptoms and radiologic abnormalities (clinical cure) was achieved in approximately 75 % of clinically evaluable (per-protocol) patients in each of the treatment groups at the post-therapy TOC assessment 17 to 24 days after treatment initiation. For the most part, treatment response was maintained at the late post-therapy evaluation 31 to 45 days after treatment initiation, as only a very small number of patients (3 to 5 in each group) had relapsed by the time of this assessment. The 5-day regimen of telithromycin was not associated with a higher relapse rate than was the 10-day regimen, despite a follow-up period that was longer by 5 days.
All patients included in this study had clinical signs and symptoms and radiologic signs of AMS, and most patients (80.2%) rated their AMS as moderate in intensity. Subgroup analyses of clinical cure rates showed that a 5-day course of telithromycin was equally effective in patients with severe AMS and in those who had received antibiotics for the treatment of sinusitis during the previous year.
Roos et al recently reported clinical cure rates of 91% following a 5- or 10-day course of telithromycin at 800 mg once daily. (18) The somewhat lower clinical cure rates observed in our study might reflect the fact that fewer than 10% of our patients underwent sinus puncture, a procedure that can help relieve symptoms through aspiration of fluid. Among our patients who did undergo sinus puncture, the clinical outcome was cure in 85.7%, 85.7%, and 80.0% of patients in the 5-day telithromycin, 10-day telithromycin, and amoxicillin/clavulanic acid groups, respectively (per-protocol data).
We chose amoxicillin/clavulanic acid as the comparator drug in this study because of its proven efficacy in the empiric treatment of AMS and its activity against common causative bacterial pathogens. However, the perprotocol clinical cure rate for amoxicillin/clavulanic acid in our study (74.5% at TOC) was lower than rates reported for this agent in other studies (82 to 96%). (19-22) This can be explained to some extent by differences in study designs, analyses, and methodologies. For example, in many of the aforementioned studies, sinus puncture was performed at study entry. Moreover, the definition of clinical cure in other studies was based solely on clinical symptoms and not on radiographic resolution, which tends to lag behind clinical findings, as we saw in our study. Finally, in our study, clinical cure was evaluated 7 to 14 days alter the end of the 10-day treatment course, which allowed us to identify early cases of relapse and provided a more rigorous measure of efficacy than that seen in many of the other amoxicillin/clavulanic acid trials, in which TOC was performed closer to the end of therapy.
Of all the published studies of amoxicillin/clavulanic acid in AMS, the findings of Camacho et al are probably closest to ours in terms of the definitions used for clinical cure and failure and the types of analyses that were performed. (19) The major difference between these two studies is that Camacho et al classified patients who failed treatment after receiving less than 5 days of therapy as clinically unevaluable. If data from our study are reanalyzed to exclude such patients from our evaluable population, clinical cure rates across all treatment groups would range from 77 to 79% (instead of 73 to 75%), rates that are comparable to the rate reported by Camacho et al (82%).
Bacteriologic outcome was not a primary endpoint of our study, so the number of patients in whom sinus puncture was performed and the number of causative pathogens isolated (principally S pneumoniae and H influenzae) were small. All strains of Spneumoniae (4/4) and H influenzae (5/5) were eradicated following treatment with telithromycin, including two isolates of S pneumoniae that exhibited reduced susceptibility to penicillin G (one of which was also resistant to erythromycin A) and three isolates of beta-lactamase-positive H influenzae. Telithromycin's antibacterial activity against such strains is well documented in vitro. Bacteriologic efficacy was the primary endpoint in the study (n = 336) of telithromycin in adult AMS by Roos et ai. (18) They found that 91% of causative pathogens were eradicated by a 5-day regimen of telithromycin, a value comparable to those reported for standard durations of therapy with amoxicillin/ clavulanic acid, cefdinir, and cefuroxime axetil. (21,23,24)
Patient compliance with oral antibacterial therapy is notoriously poor, particularly during the treatment of acute infections such as AMS. (8,16) Because symptoms frequently subside before the pathogen is eradicated, patients often prematurely stop taking their medication. The duration of treatment and the frequency of daily dosing have been shown to be two of the most important factors that influence compliance with an antibiotic treatment regimen. Logically, patients are more likely to be compliant with a short-duration, once-daily treatment regimen, such as the 5-day telithromycin regimen used in this study, than with a prolonged regimen that requires multiple daily doses. In addition to being associated with disease recurrence and significant healthcare expenditure, poor compliance may have broader ramifications, such as encouraging selection of resistant isolates. (8) Compliance with medication was generally good in our study. Unfortunately, one of the drawbacks of randomized, double-dummy studies is that they do not reflect real-world conditions, and therefore reliable evaluations of the effects that factors such as dosing frequency and duration have on compliance are not possible.
Another rationale for shortening treatment regimens is the potential for improved tolerability. In our study, both of the telithromycin regimens were generally well tolerated. Adverse events were mostly mild or moderate in intensity and were generally similar in nature and frequency to those that occurred with amoxicillin/clavulanic acid. The most frequently reported adverse events in each of the three groups were diarrhea and nausea. Notably, a significantly lower incidence of vaginal candidiasis occurred among women who received telithromycin for 5 days than in those who received amoxicillin/clavulanic acid, which is of clinical relevance in view of the frequency with which this adverse effect occurs with broadspectrum antibiotics. Differences in abnormal laboratory values rated as clinically noteworthy were not statistically significant among the treatment groups, and there were no treatment-related changes in vital signs or clinically relevant changes in Q-Tc intervals.
In conclusion, the results of our study demonstrate that a 5- or 10-day course of telithromycin at 800 mg once daily is as effective clinically and was equally well tolerated as a 10-day treatment with amoxicillin/clavulanic acid. Thus, short-course treatment with telithromyein for 5 days, with the convenience of once-dally administration, appears to be a valuable option for the treatment of acute bacterial sinusitis in adults.
References
(1.) Gwaltney JM, Jr. Acute community acquired bacterial sinusitis: To treat or not to treat. Can Respir J 1999;6(Suppl A):46A-50A.
(2.) Youngs R. Sinusitis in adults. Curt Opin Pulm Med 2000;6: 217-20.
(3.) Schappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. Vital Health Stat 13 1999;(143):i-iv, 1-39.
(4.) Parsons DS, Wald ER. Otitis media and sinusitis: Similar diseases. Otolaryngol Clin North Am 1996;29:11-25.
(5.) Ahuja GS, Thompson J. What role for antibiotics in otitis media and sinusitis? Postgrad Med 1998;104(3):93-9, 103-4.
(6.) Bartlett JG. IDCP guidelines: Management of upper respiratory tract infections. Infect Dis Clin Pract 1997;6:212-20.
(7.) Felmingham D, Gruneberg RN. The Alexander Project 1996-1997: Latest susceptibility data from this international study of bacterial pathogens from community-acquired lower respiratory tract infections. I Antimicrob Chemother 2000:45:191-203.
(8.) Sclar DA, Tartaglione TA, Fine MJ. Overview of issues related to medical compliance with implications for the outpatient management of infectious diseases. Infect Agents Dis 1994;3:266-73.
(9.) Pankuch GA, Visalli MA, Jacobs MR, Appelbaarn PC. Susceptibilities of penicillin- and erythromycin-susceptible and -resistant pneumoeocci to HMR 3647 (RU 66647), a new ketolidc, compared with susceptibilities to 17 other agents. Antimicrnb Agents Chemother 1998;42:624-30.
(10.) Dubois J, St. Pierre C. In vitro study of the minimal inhibitory concentrations (MIC) of telithromycin (HMR 3647), macrolides and quinolones against Haemophilus, Streptococcus, Staphylococcus and Moraxella strains obtained from upper and lower respiratory tract infections and from maxillary sinus aspiration. Presented at the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; Sept. 17-20, 2000; Toronto.
(11.) Agouridas C, Bonnefoy A, Chantot IF. In vitro antibacterial activity of HMR 3647, a novel ketolide highly active against respiratory pathogens. Presented at the 4th International Conference on Macrolides, Azalides, Streptogramins and Ketulides; Jan. 21-23, 1998; Barcelona.
(12.) Biedenbach DJ, Barrett MS, Jones RN. Comparative antimicrobiul activity and kill-curve investigations of novel ketolide antimicrobial agents (HMR 3004 and HMR 3647) tested against Haemophilus influenzae and Moraxella catarrhalis strains. Diagn Microbiol Infect Dis 1998;31:349 53.
(13.) Jacobs MR, Bajaksouzian S, Zilles A, et al. Susceptibilities of Streptococcus pneumoniae and Haemophilus influenzae to 10 oral antimicrobial agents based on pharmacodynamic parameters: 1997 U.S. Surveillance study. Antimicrob Agents Chemother 1999;43:1901-8.
(14.) Lenfant B, Saltan E, Wable C, er al. Pharmacokinetics of 800 mg once-daily oral dosing of the ketolide, HMR 3647, in healthy young volunteers. Presented at the 38th Interscience Conference on Antimierobial Agents and Chemotherapy; Sept. 24-27, 1998; San Diego.
(15.) Miyamoto N, Murakami S, Yajin K, et al. Pharmacokiuetie study of a new ketolide antinficrobial telithromycin (HMR 3647) in otorhinolaryngology. Presented at the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; Sept. 17-20, 2000; Toronto.
(16.) Brook I, Gooch WM III, Jenkins SG, et al. Medical management of acute bacterial sinusitis: Recommendations of a clinical advisory committee on pediatric and adult sinusitis. Ann Otol Rhinol Laryngol 2000;109:2-20.
(17.) Thornsberry C, Ogilvie P, Kahn J, Mauriz Y. Surveillance of antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in the United States in 1996-1997 respiratory season. The Laboratory Investigator Group. Diagn Microbiol Infect Dis 1997;29:249-57.
(18.) Roos K, Brunswig-Pitschner C, Kostrica R, et al. Efficacy and tolerability of once-daily therapy with telithromycin for 5 or 10 days for the treatment of acute maxillary sinusitis. Chemotherapy 2002;48:100-8.
(19.) Camacho AE, Cobo R, Otte J, et al. Clinical comparison of cefuroxime axetil and amoxicillin/clavulanate in the treatment of patients with acute bacterial maxillary sinusitis. Am J Med 1992;93:271-6.
(20.) Calhoun KH, Hokanson JA. Multicenter comparison of clarithromycin and amoxicillin in the treatment of acute maxillary sinusitis. Arch Fam Med 1993;2:837-40.
(21.) Gwaltney JM, Jr., Savolainen S, Rivas P, et al. Comparative effectiveness and safety of cefdinir and amoxicillin-clavulanate in treatment of acute community-acquired bacterial sinusitis. Cefdinir Sinusitis Study Group. Antimicrob Agents Chemother 1997;41:1517-20.
(22.) Von Sydow C, Savolainen S, Soderqvist A. Treatment of acute maxillary sinusitis--comparing cefpodoxime proxetil with amoxicillia. Scand J Infect Dis 1995;27:229-34.
(23.) Sydnor A, Jr., Gwalmey JM, Jr., Cocchetto DM, Scheld WM. Comparative evaluation of cefuroxime axetii mid cefaclor for treatment of acute bacterial maxillary sinusitis. Arch Otolaryngol Head Neck Surg 1989;115:1430-3.
(24.) Sydnor TA, Kopp EJ, Anthony KE, et al. Open label assessment of levofloxacin for the treatment of acute bacterial sinusitis in adults. Ann Allergy Asthma Immunol 1998;80:357-62.
From Sound Medical Research. Orchard Park, N.Y.
Reprint requests: Maynard Luterman, MD, 35 Hemlock Hill Rd., Orchard Park, N Y 14127. Phone: (716) 662 7921 ; fax: (716) 662-7922; e-mail: mlutcrman@aol.com
This study was funded by an unrestricted grant from Aventis Pharmaceuticals of Bridgewater, N.J., and was originally presented during the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy, Sept. 17-20, 2000: Toronto.
COPYRIGHT 2003 Medquest Communications, LLC
COPYRIGHT 2003 Gale Group