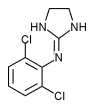
Hot flushes, a set of vasomotor symptoms including a feeling of warmth, redness of the face and upper body, sweating and dizziness, are frequent postmenopausal symptoms. These symptoms are also the most common side effects associated with use of the antiestrogen agent tamoxifen. The symptoms can be severe and may interfere with daily activities and sleep, and may cause discontinuation of tamoxifen therapy. Now that tamoxifen is being used for longer periods in the treatment of early-stage breast cancer, hot flushes are becoming more pronounced. Clonidine hydrochloride is a centrally acting alpha-adrenergic agonist that reduces vascular reactivity and is currently used for treatment of hypertension. It has been shown to control hot flushes thought to be caused by nonadrenergic hyperactivity.
Pandya and associates performed a randomized, controlled trial to study the effect of clonidine on hot flushes in women taking tamoxifen for breast cancer. Postmenopausal women who had been receiving adjuvant tamoxifen therapy for breast cancer for at least one month and reported at least one hot flush per day were included. Patients with coronary artery insufficiency or symptomatic cardiac disease, syncope or symptomatic hypotension were excluded. Patients were randomized to receive oral clonidine, in a dosage of 0.1 mg daily, or placebo at bedtime for eight weeks. Self-report diaries were kept by participants of hot flush symptoms. A side effect checklist was also made available to all participants.
Both groups reported milder hot flush symptoms during treatment, but the reduction was greater in the clonidine group. A significant difference was seen in the mean changes in quality-of-life score at week 8. Difficulty sleeping was the only potential side effect reported significantly more often by the clonidine group.
The authors conclude that oral clonidine can reduce the frequency of tamoxifen-induced hot flushes in postmenopausal women with breast cancer for at least eight weeks. Baseline frequency of hot flushes did not influence patient response to clonidine treatment. The toxicity of oral clonidine was low at the dosage of 0.1 mg daily. Continued use of clonidine for longer periods would probably provide similar benefit, but this step requires further research.
COPYRIGHT 2000 American Academy of Family Physicians
COPYRIGHT 2000 Gale Group