Gaspoz JM, Coxson PG, Goldman PA, et al. Cost effectiveness of aspirin, clopidogrel, or both for secondary prevention of coronary heart disease. N Engl J Med 2002; 346:1800-6.
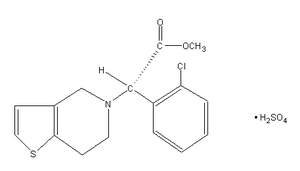
* BACKGROUND Clopidogrel is a platelet aggregation inhibitor that is slightly more effective than aspirin in reducing the risk of cardiovascular events in individuals with preexisting cardiovascular disease (0.51% annual absolute risk reduction; Lancet 1996; 348:1329-39). However, clopidogrel is currently 80 times more expensive than aspirin. The authors looked at the risks, benefits, and costs of long-term use of various therapeutic strategies involving these 2 medications.
* POPULATION STUDIED A computer simulation, known as the Coronary Heart Disease Policy Model, was used to predict the number of patients in the United States (35-84 years) who would develop coronary disease before or during the next 25 years, as well as the number of subsequent cardiovascular events and deaths these individuals would experience. Only patients predicted to survive their first month after a cardiac event were included in the therapeutic intervention analysis. Parameters lot the model were based on cohort studies and clinical trials found in the medical literature.
* STUDY DESIGN AND VALIDITY Beginning with their estimated number of Americans with coronary disease and cardiovascular events, the authors predicted the reduction in events using aspirin, clopidogrel, or both. The 4 possible treatment strategies were (1) aspirin 325 mg/day for all eligible patients; (2) aspirin for all eligible patients or clopidogrel 75 mg/day for the remaining 5.7% ineligible for aspirin; (3) clopidogrel 75 mg/day for all patients; or (4) a combination of clopidogrel for all patients plus aspirin for all eligible patients. They also considered costs of various interventions, including hospitalizations, rehabilitation services, outpatient and home services, and treatment for adverse drug effects such as gastrointestinal bleeding. To carry out the cost effectiveness analysis over such a long time period, the authors discounted costs at a rate of 3% per year (a typical amount) and converted all values to year-2000 US dollars. Sensitivity analysis used upper and lower bounds of reductions from past trial data to give a reasonable range of values. As with all hypothetical cost-effectiveness studies, this study only represents the authors' best estimates of costs and benefits, not actual results from a therapeutic trial or cohort. Issues such as the safety of combination therapy over this prolonged time period have not been well established.
* OUTCOMES MEASURED The main outcome was the cost per quality-adjusted life year (QALY) gained, that is, the cost of an additional year of optimal health.
* RESULTS Aspirin alone in all eligible patients (strategy #1) resulted in an estimated $11,000 per QALY gained. Giving clopidogrel to the 5.7% of patients ineligible for aspirin (strategy #2) would prevent some subsequent events at an increased cost, resulting in a total estimate of $31,000 per QALY gained compared with the first strategy. Using clopidogrel alone for everyone (strategy #3) led to a very high estimated cost of $250,000 per QALY gained compared with strategy #2. Combination therapy of clopidogrel for everyone plus aspirin for the 96.3% of eligible patients (strategy #4) resulted in an estimated cost of $130,000 per QALY gained compared with strategy #2. However, in patients with annual risks 3 times as high as that of the average patient with coronary disease, this ratio fell below $64,000 per QALY gained.
A cost of $50,000 per QALY gained is generally considered acceptable in Western society, and as such strategy #2 appears to balance cost and benefits most reasonably. Because the cost of clopidogrel will probably decrease over the coming years, the authors also took this price change into account for various strategies. If the cost of clopidogrel fell 70% (to approximately $1.00 per dose), then strategy #4 (combination therapy) would drop below the $50,000 threshold.
RECOMMENDATIONS FOR CLINICAL PRACTICE Considered from a societal standpoint, clopidogrel at its current price has acceptable cost effectiveness when used by patients with cardiovascular disease who cannot take aspirin. If the cost of clopidogrel falls substantially in the future combination therapy with both clopidogrel and aspirin in these patients may also be a reasonable public health policy.
COPYRIGHT 2002 Dowden Health Media, Inc.
COPYRIGHT 2002 Gale Group