Since the introduction of chlorpromazine (Thorazine) in 1952, antipsychotic medications have transformed the treatment of schizophrenia and other psychotic disorders. In most patients, schizophrenia improves with antipsychotic therapy, and in many patients, substantial improvement occurs. [1] However, between 10 and 20 percent of patients derive little or no benefit from conventional antipsychotic therapy. Among those who do respond, the improvement in such symptoms as social withdrawal, flat affect and lack of motivation [2,3] is often less than the improvement in psychotic thought processes. Furthermore, depending on the duration of therapy, 20 to 40 percent of patients treated with conventional antipsychotic agents develop the potentially disabling and chronic involuntary movements of tardive dyskinesia. [4,5]
For these reasons, a great deal of interest is being directed at new classes of antipsychotic agents that may have therapeutic advantages over conventional antipsychotics, including no risk of tardive dyskinesia. Clozapine (Clozaril), which was approved in late 1989, is the first of these new drugs to be released in the United States.
Chemistry
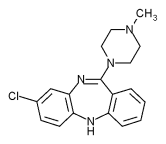
Clozapine is a tricyclic dibenzodiazepine derivative. It is related chemically to the antipsychotic dibenzoxazepine drug loxapine (Loxitane), but its pharmacologic characteristics differ significantly. The serotoninergic ([S.sub.1] subtype), alpha-adrenergic ([alpha.sub.1] and [alpha.sub.2]) and histaminergic ([H.sub.1] subtype) blocking activities of clozapine are greater than its dopamine-blocking effects. In addition, clozapine is a potent muscarinic acetylcholine receptor antagonist. [6] The relative potency of clozapine is estimated to be twice that of chlorpromazine (i.e., 1 mg of clozapine equals 2 mg of chlorpromazine). [2]
Mechanism of Action
Like conventional antipsychotic drugs, clozapine blocks receptors for the [D.sub.2] dopamine subtype. However, compared to similar drugs, it has a lower affinity for [D.sub.2] dopamine receptors and binds more strongly to receptors for the [D.sub.1] dopamine subtype. [6,7] Clozapine's activity at receptors for [D.sub.1] and [D.sub.2] dopamine and at receptors for the [5HT.sub.2] subtype of serotonin may be related to its unique clinical features. [7,8] The drug appears to act selectively at dopamine neuronal systems in the cortical and limbic regions in preference to the nigrostriatal and tuberoinfundibular regions. It may be because of this property that clozapine causes few extrapyramidal effects and only minimal elevation of prolactin levels. [6]
Pharmacokinetics
Clozapine is rapidly absorbed from the gastrointestinal tract, and peak plasma concentrations are achieved in an average of two and one-half hours. [9] The drug is approximately 95 percent bound to serum proteins. Clozapine is almost completely metabolized, and its metabolites are excreted in urine and feces. The biologic activity of clozapine's metabolites is much weaker than that of the parent compound. The elimination half-life of clozapine after multiple does varies considerably, but averages 12 hours. [3]
Efficacy
Double-blind studies [3,5] have shown that clozapine is at least as effective as chlorpromazine or haloperidol (Haldol) in relieving all types of symptoms in acutely ill schizophrenic patients and that it is superior to these two agents in the treatment of refractory patients. However, because of the risk of agranulocytosis (in some cases fatal), clozapine was not marketed in the United States until a carefully designed, well-controlled multicenter trial [5] demonstrated the significant superiority of the drug over conventional antipsychotics in a rigorously defined group of treatment-resistant patients. [2]
This study included 268 severely ill schizophrenic patients who, over the previous five years, had failed to respond to at least three different antipsychotic medications from at least two different chemical classes. The dosage of each antipsychotic had to have been equivalent to at least 1,000 mg of chlorpromazine, and the drug had to have been given continuously for at least six weeks. [2]
To confirm the lack of treatment response, all patients were given high-dose haloperidol for six weeks. At the end of this time, fewer than 2 percent of the patients were classified as haloperidol responders. Those who did not improve with haloperidol therapy were entered into a double-blind trial of clozapine and high-dose chlorpromazine. After six weeks of therapy, 30 percent of the clozapine-treated patients, but only 4 percent of the chlorpromazine-treated patients, were characterized as significantly improved on standardized rating scales. [2]
Subsequent prospective studies have suggested that patients continue to improve after the first six weeks of clozapine therapy. In the first six weeks of an open uncontrolled prospective study of 51 treatment-resistant schizophrenic patients, [10] only 45 percent of the patients who ultimately responded to clozapine could be identified. About 60 percent of the patients demonstrated a response with one year of therapy, although about three-fourths of the responders were identified within the first three months.
In an open uncontrolled prospective study, [11] eight of 14 patients with refractory chronic schizophrenia who were treated for up to two years did substantially better while on clozapine than on adequate doses of several other antipsychotic medications. Only about half of the eventual improvement, as judged by the Brief Psychiatric Rating Scale, was evident within the first 12 weeks of clozapine therapy.
In yet another study, [12] clozapine was associated with significant improvement in quality of life over six-month period and was independently associated with an 80 percent decrease in rehospitalization over the first year of therapy.
Several studies have demonstrated that in addition to apparently not causing tardive dyskinesia, clozapine actually has therapeutic effects against tardive dyskinesia, especially tardive dystonic movements. In a study of 37 patients who were maintained on clozapine, [4] 40 percent showed remission of tardive dyskinesia, most within the first six months of therapy.
Adverse Reactions
Rarely, clozapine causes extrapyramidal symptoms such as pseudoparkinsonism or akathisia. To date, no confirmed cases of tardive dyskinesia have been attributed to the drug. [5,6]
The most serious adverse effect of clozapine is agranulocytosis, which occurs in 1 to 2 percent of patients. [3] The mortality rate from this condition can be significantly decreased by regularly monitoring the white blood cell count and by immediately discontinuing clozapine when agranulocytosis develops. [5] Once agranulocytosis appears, clozapine should never be restarted.
Sandoz Pharmaceuticals (East Hanover, N.J.), the manufacturer of clozapine, recently notified psychiatrists that sudden respiratory depression, sometimes with orthostatic hypotension and syncope, occurs in about one of 2,000 to 6,000 patients treated with clozapine. [13] This complication, which may result in respiratory arrest, may occur with the first dose or during dosage escalation. The risk of respiratory depression may be increased by concomitant use of benzodiazepines while clozapine therapy is initiated.
Clozapine has been found to lower the seizure threshold. The drug has been associated with a dose-related increase in the incidence of seizures, which appears to be higher than with other antipsychotic agents. Dosages of up to 300 mg per day are associated with a 1 to 2 percent risk of seizures, dosages of 300 to 600 mg per day with a 3 to 4 percent risk, and dosages of 600 to 900 mg per day with a 5 percent risk. [5]
Sedation and orthostatic hypotension are common when clozapine therapy is first initiated. [6] These side effects may be minimized by starting with a low dosage, which is then gradually increased. Tolerance to clozapine often develops over time.
Benign hyperthermia, usually with temperature elevations of 0.5[degrees] C to 1.0[degrees] C (1[degrees] F to 2[degrees] F), may occur during the first three weeks of clozapine therapy. [5] However, greater temperature elevations may occur in some patients, necessitating discontinuance of the drug and close hematologic monitoring. [5] The neuroleptic malignant syndrome, consisting of fever, rigidity, altered state of consciousness and autonomic instability, has also been reported in patients treated with clozapine. [14]
Despite the anticholinergic potency of clozapine, hypersalivation is common, especially at night. [5] Tachycardia is also common and is not related to postural hypotension. [6] Other frequent side effects of clozapine include nausea, constipation, abnormal ejaculation and urinary symptoms such as incontinence, urgency or retention. [5] Hepatic dysfunction occurs in approximately 1 percent of patients. [6]
Drug Interactions
Because clozapine has potent sedative, hypotensive and anticholinergic properties, caution should be used in combining this agent with other drugs, particularly during the initiation of therapy. The possibility exists that clozapine may interact with other protein-bound drugs such as digoxin (Lanoxin) or warfarin (Coumadin, Panwarfin).
While a patient is receiving clozapine other drugs associated with significant rates of agranulocytosis, such as carbamazepine (Tegretol), should be avoided. [6] Based on the recent Sandoz announcement, it would be prudent to limit the use of benzodiazepines during the initiation of clozapine therapy. [13] Because of the alpha-adrenergic blocking activity of clozapine, epinephrine should not be administered in the event of drug-induced hypotension.
Indications
The U.S. Food and Drug Administration has approved the use of clozapine to treat severely ill schizophrenic patients who have failed to respond adequately to standard antipsychotic therapy, either because of insufficient effectiveness or because an effective dose cannot be achieved due to intolerable drug side effects. It may be best to limit the use of clozapine to patients who have not responded to well-documented trials of adequate doses of antipsychotic medications from at least two classes or who have manifested overwhelming side effects, such as severe tardive dyskinesia. [5,6]
Treatment
Before Clozapine therapy is initiated, a thorough medical history should be obtained and a complete physical examination should be performed. An electrocardiogram also should be obtained. Laboratory tests should include a baseline complete blood count and hepatic and renal function tests. [6]
Clozapine therapy is initiated in a dosage of 25 mg once or twice daily. The daily dosage is increased in increments of 25 to 50 mg until a target dosage of 300 to 450 mg per day is achieved at the end of two weeks. Most patients respond to 300 to 600 mg per day, given in divided doses. Before initiating clozapine therapy, physicians should consult the manufacturer's package insert and should become thoroughly familiar with the proper use of this drug.
Clozapine may help improve the behavior and affect of many patients, but some elements of psychosis and thought disorder commonly remain. Because of the potential for serious adverse effects with clozapine therapy, careful informed consent must be obtained from patients and their families. [6,15] Adjunctive psychosocial therapy and patient education should always be available for patients treated with clozapine. [15]
White blood cell count should be obtained weekly for the duration of clozapine therapy, and hepatic functions should be monitored early in treatment. [15] Vital signs also should be monitored. Sandoz recommends that therapy be discontinued if the total white blood cell count drops to below 3,000 per [mm.sup.3] ([3.0 X 10.sup.9] per L) or if the granulocyte count drops to below 1,500 per [mm.sup.3]. [9] Patients with white blood cell counts below 2,000 per [mm.sup.3] (2.0 X [10.sup.9] per L) or granulocyte counts below 1,000 per [mm.sup.3] may require additional hematologic evaluation and protective isolation. [9] Whenever a patient's temperature increases to 38.3 [degrees] C (101 [degrees] F) or greater, clozapine should be withheld, blood counts performed and medical evaluation initiated. [6]
Uncertainty remains as to what constitutes an adequate trial of clozapine. Current recommendations generally range from at least three to six months. [5,6] When clozapine is stopped for reasons other than neutropenia, the drug should be discontinued gradually to avoid withdrawal symptoms. [6]
Final Comment
Originally, clozapine was available in the United States only as part of an expensive and controversial mandatory system for distributing the drug and monitoring side effects/ [16] Sandoz has since agreed to make clozapine available through physicians, pharmacies, and appropriate medical and psychiatric health care facilities registered with Sandoz and agreeing to follow guidelines for monitoring white blood cell counts and protecting at-risk patients from rechallenge with clozapine.
Under the mandatory system, clozapine therapy costs approximately $9,000 per year. [15] Without the mandatory system, the total cost of the drug and weekly white blood cell counts may be nearly as high, depending on the daily dosage.
REFERENCES
[1] Kane JM. The current status of neuroleptic therapy. J Clin Psychiatry 1989;50:322-8.
[2] Kane JM, Honigfeld G, Singer J, Meltzer H. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 1988; 45:789-96.
[3] Stephens P. A review of clozapine: an antipsychotic for treatment-resistant schizophrenia. Compr Psychiatry 1990;31:315-26.
[4] Lieberman JA, Saltz BL, Johns CA, Pollack S, Kane JM. Clozapine effects on the tardive dyskinesia. Psychopharmacol Bull 1989;25:57-62.
[5] Safferman A, Lieberman JA, Kane JM, Szymanski S, Kinon B. Update on the clinical efficacy and side effects of clozapine. Schiz Bull 1991;17:247-61.
[6] Lieberman JA, Kane JM, Johns CA. Clozapine: guidelines for clinical management. J Clin Psychiatry 1989;50:329-38.
[7] Meltzer HY. The mechanism of action of novel antipsychotic drugs. Schiz Bull 1991;17: 263-87.
[8] Gerlach J. New antipsychotics: classification, efficacy, and adverse effects. Schiz Bull 1991; 17:289-309.
[9] Clozapine. In: Facts and comparisons. St. Louis: Facts and Comparisons Div., J.B. Lippincott Co., 1991:267m-r.
[10] Meltzer HY, Bastani B, Kwon KY, Ramirez LF, Burnett S, Sharpe J. A prospective study of clozapine in treatment-resistant schizophrenic patients. I. Preliminary report. Psychopharmacology 1989;99(Suppl:S68-72.
[11] Mattes JA. Clozapine for refractory schizophrenia: an open study of 14 patients treated up to 2 years. J Clin Psychiatry 1989;50: 389-91.
[12] Meltzer HY, Burnett S, Bastani B, Ramirez LF. Effects of six months of clozapine treatment on the quality of life of chronic schizophrenic patients. Hosp Comm Psychiatry 1990;41: 892-7.
[13] Mailgram: Clozaril. East Hanover, N.J.: Sandoz Pharmaceuticals, June 20, 1991.
[14] DasGupta K, Young A. Clozapine-induced neuroleptic malignant syndrome. J Chin Psychiatry 1991;52:105-7.
[15] Green Al, Salzman C. Clozapine: benefits and risks. Hosp Comm Psychiatry 1990;41: 379-80.
[16] Salzman C. Mandatory monitoring for side effects. The "bundling" of clozapine. N Engl J Med 1990;323:827-9.
DAVID L. BUCH, M.D. is assistant professor and director of inpatient psychiatric services at Hahnemann University School of Medicine, Philadelphia. Dr. Buch graduated from Vanderbilt University School of Medicine, Nashville, and trained for one year in internal medicine at the University of California, San Diego. After three years in the U.S. Public Health Service, he completed his psychiatric training at East Carolina University, Greenville, N.C.
COPYRIGHT 1992 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group