Patients treated with some antipsychotic medications have been shown to be at increased risk for ventricular arrhythmias, cardiac arrest, and sudden death. This includes patients with schizophrenia who are treated with thioridazine (Mellaril), haloperidol (Haldol), and other conventional antipsychotics (see accompanying table). This increased risk has been attributed to the QT-prolonging properties of conventional antipsychotics. The newer atypical antipsychotics may be more effective in the treatment of negative symptoms in schizophrenia, and they may have a lower risk of extrapyramidal side effects and tardive dyskinesia compared with conventional antipsychotics. Because of this improved side effect profile, the use of atypical antipsychotics has increased. The effects of atypical antipsychotics on cardiac events and sudden death has not been established. Liperoti and associates performed a case-control study to compare the effects of conventional and atypical antipsychotics on the risk of hospitalization for ventricular arrhythmias or cardiac arrest among older patients.
The authors collected data from the Systematic Assessment of Geriatric Drug Use via Epidemiology database for patients at Medicaid- and Medicare-certified nursing homes in six states. This information is linked to the Medicare inpatient claim files. Patients were included in the study if they had a primary diagnosis of cardiac arrest or ventricular arrhythmia. A control group consisting of residents in the same facilities was selected from the database.
A total of 649 patients had used antipsychotic medication within seven days of admission, and 2,962 patients were included in the control group. The use of conventional antipsychotics was associated with an increased risk of hospitalizations for cardiac arrest or ventricular arrhythmias (odds ratio [OR], 1.86; 95% confidence interval [CI], 1.27 to 2.74). The use of atypical antipsychotics was not associated with an increased risk for hospitalization. Patients with cardiac disease who took conventional antipsychotics were at increased risk of hospitalizations for ventricular arrhythmias compared with the control group (OR, 3.27; 95% CI, 1.95 to 5.47). The synergy index for this data was 1.19, indicating that there was no interaction between conventional antipsychotic use and preexisting cardiac disease.
The authors conclude that the use of conventional antipsychotic medications is associated with an increased risk of hospitalizations for cardiac arrest and ventricular arrhythmias, and that atypical antipsychotics are not associated with increased risk. They add that the use of conventional antipsychotics should be avoided, if possible, in patients with cardiac disease.
KARL E. MILLER, M.D. Liperoti R, et al. Conventional and atypical antipsychotics and the risk of hospitalization for ventricular arrhythmias or cardiac arrest. Arch Intern Med March 28, 2005;165:696-701.
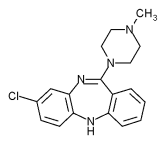
Antipsychotic Medications
Atypical
Clozapine (Clozaril) Olanzapine (Zyprexa) Quetiapine (Seroquel) Risperidone (Risperdal)
Conventional
Chlorpromazine (Thorazine) Chlorprothixene (Taractan) Fluphenazine (Prolixin) Haloperidol (Haldol) Loxapine (Loxitane) Molindone (Moban) Perphenazine (Trilafon) Promazine * Thioridazine (Mellaril) Thiothixene (Navane) Trifluoperazine (Stelazine)
*--Not available in the United States.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2006 Gale Group