Patients with congestive heart failure (CHF) are at high risk of fatal ventricular arrhythmias; however, there are limited data on the effectiveness of preventive interventions. Bardy and colleagues conducted a randomized placebo-controlled trial comparing the effects of conventional therapy plus amiodarone (Cordarone), an implantable cardioverter-defibrillator (ICD), or placebo on all-cause mortality in patients with CHF.
Investigators enrolled 2,521 patients who were New York Heart Association (NYHA) class II or III CHF and had a left ventricular ejection fraction of 35 percent or less (median: 25 percent). The etiology of CHF could be ischemic or nonischemic. Participants were primarily white men (77 percent). All patients received standard therapy for CHF, including angiotensin-converting enzyme (ACE) inhibitors and beta blockers when clinically appropriate.
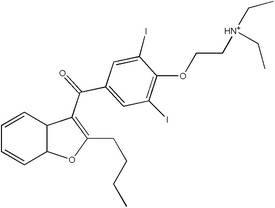
Patients were randomized to receive amiodarone, an ICD, or placebo. Placebo and amiodarone administration was double blind and partially weight based (average dose: 300 mg). Defibrillators were set up in single-lead, shock-only mode because the primary intention was to treat sustained ventricular tachycardia or ventricular fibrillation. The three groups were similar in size lowed for at least two years; median follow-up was 45.5 months.
Discontinuation rates for drug therapy were 22 percent for placebo and 32 percent for amiodarone. Seven percent of patients in the medication and placebo groups ended up on open-label amiodarone, and 14 percent of patients in the ICD group crossed over to open-label amiodarone during follow-up. Eleven percent of patients in the drug and placebo groups crossed over to an ICD. The most common negative side effects of amiodarone were tremor (4 percent) and increased hypothyroidism (6 percent). Complications in the ICD group occurred as well, with 5 percent of participants having problems at the time of implantation and 9 percent during follow-up. This included events necessitating surgery, hospitalization, or other medical therapy.
Death occurred in 29 percent of patients receiving placebo, 28 percent of patients receiving amiodarone, and 22 percent of patients in the ICD group. Thus, ICD use reduced the risk of death by 7 percent. Amiodarone did not make a significant difference.
Approximately one third of patients in the ICD group received shocks from their devices, with 68 percent being shocked for rapid ventricular tachycardia or ventricular fibrillation. ICD therapy led to a significant absolute reduction in mortality of 11.9 percent in patients with NYHA class II CHF but no significant risk reduction in patients with NYHA class III CHF. Amiodarone did not decrease risk of death in patients with NYHA class II CHF, but it relatively increased the risk of death by 44 percent in patients with NYHA class III CHF. The use of ICDs reduced the absolute risk of death by 7.2 percent at five years, whereas amioda-rone therapy showed no benefit.
The authors conclude that conservatively programmed, shock-only ICDs significantly decrease the relative risk of death in patients with CHF, whereas amiodarone has no positive effect on survival. Other defibrillator studies have shown increased benefit for patients with lower ejection fractions or with NYHA class III CHF. Thus, the lack of benefit found for patients with NYHA class III CHF in this study should be considered in the context of the larger evidence base. Because this study used only single-lead, shock-only treatment, these findings may not apply to all types of ICDs.
CHUCK CARTER, M.D.
Bardy GH, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure [published correction appears in N Engl J Med May 19, 2005;352:2146]. N Engl J Med January 20, 2005;352:225-37.
EDITOR'S NOTE: In an accompanying editorial, (1) McClellan and Tunis discuss how the Centers for Medicare and Medicaid Services (CMS) will respond to this study. In short, CMS will expand coverage, coordinate patient registries, and support clinical outcomes research. Physicians should know that CMS will use the evidence derived from this process to inform future coverage decisions. At an estimated reimbursement of $30,000 per ICD for the potentially 500,000 newly covered patients, this type of evidence-informed oversight seems appropriate. For now, the evidence is trending toward ICDs as a routine addition to the CHF armamentarium. Thus, family physicians should consider whether their patients with CHF are at high risk for arrhythmia and consult for this intervention after discussing the risks and benefits. Furthermore, this should prompt reevaluation of the entire treatment plan. Often patients are not receiving proven treatments (e.g., angiotensin-converting enzyme inhibitors, beta blockers), and the outcomes observed in this trial were in patients on appropriate medical therapy.--C.C.
REFERENCE
(1.) McClellan MB, Tunis SR. Medicare coverage of ICDs. N Engl J Med 2005;352;222-4.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group