In the February issue of The Nurse Practitioner, the Drug News editors included a brief synopsis of the drug, rosuvastatin (Crestor). The following is an expanded review of this important new medication in the treatment of heart disease, and includes new information about potential adverse reactions.
Dyslipidemia continues to be under-treated despite clear guidelines set by the American College of Cardiology. It is estimated that only one-third of eligible patients receive therapy outside the hospital and many of these treated patients fail to achieve their target low-density lipoprotein levels.1 This is in spite of the fact that dyslipidemia is one of the most researched and easily modified risk factors for arthrosclerosis and subsequent hypertension, coronary heart disease (CHD), and cerebral vascular accident. Current therapies include dietary changes such as adding oat bran, advanced pharmaceuticals, and even gene therapy.
In August 2003, AstraZeneca received the Food and Drug Administration's (FDA) approval for rosuvastatin calcium (Crestor). Rosuvastatin reduces total cholesterol (TC), low-density lipoprotein cholesterol (LDL), triglycerides (TG), and apolipoprotein B (apoB), a main component of LDL.2,3 Rosuvastatin increases high-density lipoprotein cholesterol (HDL) and apolipoprotein Al.2,3 It is approved for patients with primary hypercholesterolemia, mixed dyslipidemia, and hypertriglyceridemia.4 Rosuvastatin seems to improve many aspects of serum cholesterol, and has the potential to reduce the risk of atherosclerosis and resulting CHD.
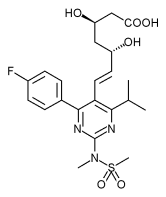
Rosuvastatin is a hydroxy-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitor, or "statin". It joins five other drugs that are also HMG-CoA reductase inhibitors. Early research indicates that rosuvastatin may achieve greater outcomes than the other drugs in its class.2,3,5-7 One study demonstrated that clients on 40 mg daily of rosuvastatin achieved their treatment goals to a greater degree than patients who took any dose of either atorvastatin, simvastatin or pravastatin (see Table: "Comparison of Characteristics of Rosuvastatin and Other Statins").5
* Pharmacokinetics
Rosuvastatin is only available in oral form. It is lipid-soluble and diffuses well across the gastrointestinal (GI) mucosa. Rosuvastatin undergoes extensive extraction in the liver's first pass effect for a final bioavailability of 20% in systemic circulation.8 Peak plasma concentrations are reached in 3 to 5 hours. Both the peak concentration and the area under the plasma concentration curve (AUC) are dose proportionate.8
Rosuvastatin has a 24-hour half-life and plasma concentrations are the same whether taken with or without food, in the morning or at night.8 This allows patients to somewhat individualize their dosing schedule and may enhance patient compliance. Therapy compliance is a major concern; more than 70% of patients currently on statins fail to continue drug therapy beyond a year.1
After absorption, the drug is widely distributed throughout the body. It is protein bound predominantly to albumin. As a result, if a patient is malnourished, has altered liver function or low albumin levels, there may be an increased amount of free drug and increased adverse reactions to the drug.
Rosuvastatin is metabolized by liver enzymes into a water-soluble, excretable form. It is oxidized by liver enzymes of the cytochrome P-450 system (CYP 450), specifically the 2C9 isoenzyme.8 This means that when rosuvastatin is administered with drugs that also utilize the CYP 450 enzymes for metabolism, either drug may be induced or inhibited. Notable drugs whose action may be induced by rosuvastatin are ibuprofen, indomethacin, losartan, phenytoin, warfarin, and torsemide.9 Common drugs whose action may be inhibited include amiodarone, cimetidine, Bactrim, fluconazole, fluoxetine, Flagyl, phenytoin, and barbiturates.9 These interactions are important for the practitioner to share with the patient since toxic levels of drugs can be reached at seemingly safe doses.
Rosuvastatin's potential drug interactions are less than other statins because rosuvastatin is metabolized by a different isoenzyme. The current leading statins, atorvastatin (Lipitor) and simvastatin (Zocor), inhibit the CYP 3A4 isoenzyme, which involves more than twice as many drug interactions as the CYP 2C9 isoenzyme.9 According to Lau et al, atorvastatin interacts with clopidogrel (Plavix), which requires the CYP 3A4 enzyme to be activated. As atorvastatin inhibits this enzyme, it also inhibits the anti-platelet aggregating action of clopidogrel.10 Therefore, rosuvastatin may be a better choice than other statins for patients also taking Plavix.
Rosuvastatin's action is augmented when taken with other cholesterol-lowering drugs, including fibric acid derivatives and niacin.4 For the same reason, AstraZeneca recommends that combination therapy with rosuvastatin and gemfibrozil should generally be avoided. Rosuvastatin coadministered with cyclosporine increases rosuvastatin's effect.4 When co-administered with oral contraceptives, the plasma concentration of ethinyl estradiol and norgestrel is increased.8 Concomitant use of rosuvastatin and warfarin often results in an increased international normalized ratio (INR). The practitioner should carefully monitor the patient's INR, as a dose reduction may be required during the co-administration of these medications.
* Pathophysiology Review
Hepatocytes synthesize cholesterol along a pathway that includes the conversion of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) to mevalonic acid.11 This reaction is carried out by the enzyme HMG-CoA reductase, which after subsequent steps, allows apolipoproteins and triglycerides to form. Apolipoproteins bind with TG to form functional lipoproteins. LDLs are comprised of apoB, and HDLs are comprised of apoAl.11
Once cholesterol components and TGs are synthesized, they are released from the liver and mature as they travel through the bloodstream. TG are eventually broken down by Iipases and excreted in the digestive tract. LDLs travel to peripheral tissues to supply cells with cholesterol via endocytosis.12 When cellular receptors for LDL and apoB are saturated, the remaining LDL is transported back to the liver by HDL.
The process of secretion, circulation, and excretion of cholesterol in the blood and cells is efficient as long as the conditions are optimal. If there are excessive circulating LDLs or TG, a disproportionate number of HDLs or LDL receptors, or damage to the endothelial layer of blood vessels, the process of atherosclerosis begins. Endothelial damage may be caused by high blood pressure, high blood sugar, smoking, high cholesterol, and numerous other factors.11 Injury stimulates inflammatory and coagulatory responses. Macrophages release enzymes and destructive oxygen-free radicals that further damage vessels, oxidize LDL, and cause smooth muscles of the vessel to proliferate and vasoconstrict.11
Macrophages engulf oxidized LDL to form foam cells, which accumulate in vessels and form fatty streaks.11 Fatty streaks damage vessels, releasing more free radicals, causing a further inflammatory response. Collagen eventually forms a fibrous plaque over the fatty streak, causing necrosis of underlying tissue and narrowing of the vessel lumen. Blood flow is reduced to distal tissues, and there is an increased potential for a portion of the plaque to rupture and obstruct a vessel.
During all phases of the atherosclerotic process, HDLs are extremely valuable in stopping further damage. Besides actively transporting LDLs from the peripheral tissues back to the liver, HDLs and apoAls also inhibit LDLs from being oxidized, prevent monocytes from adhering to the endothelium, and inhibit platelet aggregation.13 HDLs act by stimulating arterial endothelial cells to secrete vasoactive substances that slow the atherosclerotic process by inhibiting vascular endothelial cell apoptosis.13 These properties of HDLs suggest that a low HDL level may be an independent risk factor for heart disease.
Correspondingly, the highest risk of CHD is correlated with low HDL (150 mg/dL) concentrations.14 By inhibiting HMG-CoA reductase, the synthesis of cholesterol in the liver is reduced, the number of LDL and apoB receptors on the liver are increased, and the amount of HDL and apoAl is increased.2 Rosuvastatin improves all aspects of cholesterol metabolism and is therefore an effective overall treatment for CHD.
Research now indicates extended benefits of rosuvastatin beyond lowering cholesterol. Kleeman et al found that rosuvastatin reduces vascular inflammation in terms of serum amyloid and fibrinogen by over 40%, and reduces expression of tumor necrosis factor alpha (TNF-a) in atherosclerotic lesions by 88%.15 These results were independent of plasma cholesterol. Similarly, multiple studies showed that statins reduce C-reactive protein (CRP) from 25% to 50%.16-18 CRP is an independent marker of inflammation that predicts cardiovascular risk in patients with and without evidence of cardiovascular disease.19-20 Atherosclerosis is partly an inflammatory response and therefore the anti-inflammatory benefit of statins is clear.
Rosuvastatin may also decrease atherosclerosis by inhibiting intervascular coagulation. There is evidence that statins interfere with the clotting cascade by decreasing fibrinogen concentrations,15 by interfering with the conversion of prothrombin to thrombin, and by stimulating the process of fibrinolysis.21 These data imply that mevalonic acid and other precursors of cholesterol that are synthesized by HMG-CoA reductase are also precursors to cell functions other than lipid synthesis. When statins block the action of this enzyme, they also block other noncholesterol-lowering processes beneficial in treating CHD.22
* Practitioner Considerations
Before initiating rosuvastatin, secondary causes for hypercholesterolemia, such as poorly controlled diabetes mellitus, obstructive liver disease, and alcoholism must be ruled out or appropriately treated. Baseline lipoprotein and chemistry profiles (specifically creatinine, blood urea nitrogen, and electrolytes) should also be obtained before starting therapy to follow the drug's efficacy and safety. Rosuvastatin is contraindicated in patients with active liver disease or unexplained chronically elevated liver enzymes.4 Similarly, rosuvastatin should be used with caution in patients who have a history of liver disease, consume large quantities of alcohol, or are at a higher risk for myopathies (renal impairment, elderly, or hypothyroid).4 For this reason, whenever rosuvastatin is initiated or a dose change is made, liver function should be checked within 12 weeks and semiannually thereafter.4 Patients taking rosuvastatin should also have baseline and annual creatinine clearance levels done, and be routinely checked for proteinuria and hematuria. Higher doses of rosuvastatin are associated with acute renal failure secondary to rhabdomyo lysis.4
Rosuvastatin oral tablets are available in 5 mg, 10 mg, 20 mg, or 40 mg doses, although a 40 mg dose is not recommended. Treatment is tailored to meet individual goal guidelines for LDL levels, based on risk factors. The National Cholesterol Education Program suggests specific guidelines for a variety of risk factors, available at (http://www.nhlbi.nih. gov/about/ncep/index.htm). Therapeutic response of all doses is seen within 1 week, and maximum response is usually achieved within 4 weeks.8
Rosuvastatin's initial recommended dose is 10 mg. A 5 mg dose is appropriate for patients who are predisposed to severe adverse reactions or who require less aggressive reduction in LDL.4 Research shows that the initial dose of statins is the most effective, and with each increase in dose there is only a 6% improvement of outcomes.8 Patients should undergo 6 weeks of therapy combined with other risk factor interventions (e.g. diet and exercise) before dose adjustments are made.14 A 20 mg dose is appropriate for patients who failed treatment at lower doses, who have a baseline LDL >190 mg/dL, or who have familial hypercholesterolemia.
Although current recommendations for starting statin therapy are based on a patient's LDL levels, recent research indicates that health care providers should begin statins early in at-risk patients irrespective of LDL levels. In The MIRACL trial, patients hospitalized for a cardiac event who were given statins (regardless of LDL level) had 50% fewer complications compared to the patients who did not receive statins early in treatment.23 Statins also benefit patients with only moderate cardiovascular risk, such as patients with hypertension but without hyperlipidemia.24 Early disease benefits and the anti-inflammatory and anticoagulatory effects of statins indicate the benefit of rosuvastatin in both primary and secondary prevention of atherosclerosis.
* Upcoming Clinical Trials
AstraZeneca is conducting numerous additional studies to address the efficacy of rosuvastatin in primary and secondary prevention of cardiovascular morbidity and mortality. These studies are titled under the main heading GALAXY, with specific studies entitled COMETS, DISCOVERY, LUNAR, MERCURY, ORBITAL, PLUTO, etc. These studies are using various techniques to examine rosuvastatin's effect on cardiovascular problems such as inflammatory markers, atherosclerosis, metabolic syndrome, end stage renal disease, congestive heart disease, and acute coronary syndromes; and to compare rosuvastatin's effect to that of the other leading statins. Additional information is available at www.AstraZenecaPressOffice.com.
* Patient Education
While on rosuvastatin, patients should understand the importance of adhering to a cholesterol-lowering diet, an active lifestyle, and their drug therapy. Atherosclerosis and its causative factors (i.e. hypertension) are often asymptomatic for many years. Practitioners should also review with their clients any potential interactions of rosuvastatin with other medications and/or supplements the patient may be taking. Patients are also reminded to update the practitioner with any changes in medications or supplements for possible interactions. Although the patient may take rosuvastatin with or without food, any antacids should be taken at least 2 hours after taking rosuvastatin.4
Although the drug is well tolerated, patients should be aware of potential side effects. Instruct patients to report any unexplained muscle pain, tenderness, or weakness, particularly if these sensations are accompanied by malaise, fever or brown urine.4,25 These symptoms may indicate potentially life-threatening conditions such as myopathy or rhabdomyolysis. Rosuvastatin is rated pregnancy category X, and is contraindicated in women who are or may become pregnant.4 Rosuvastatin does cross the placenta, and it is unknown whether it is secreted into human breast milk. Detailed information on the safety and effectiveness for children was not available at press time. The overall frequency and type of adverse effects were similar in geriatric populations compared to younger participants.
For more information, patients can be directed to various web resources. Recommended sites include the American Heart Association (http://www.americanheart.org), the National Cholesterol Education Program (http://www.nhlbi.nih.gov/ about/ncep/index.htm), and the American Dietetic Association (http://www.eatright.org). These sites contain simple patient education materials aimed at raising awareness, and information on the prevention and treatment of coronary heart disease. The Crestor homepage includes the package insert information (http://www.crestor.com).
Dyslipidemia is an undisputed primary risk factor in the development of atherosclerosis, which is associated with numerous pathologies including hypertension, coronary heart disease and cerebral vascular accident. Guidelines continually emphasize the role of dyslipidemia and the importance of early diagnosis and prevention. Rosuvastatin, the newest statin, improves all components of dyslipidemia, has anti-inflammatory, anti-oxidant and anticoagulatory properties, and appears to be more effective than the other drugs in its class. Additionally, rosuvastatin has an easy dosing schedule and fewer potential drug-to-drug interactions. Its major adverse reaction is rhabdomyolysis. It may not be on all formularies and it is currently expensive. http://www.Drugstore.com quotes a price of $69 for 30 tablets, and 5 mg, 10 mg, 20 mg or 40 mg tablets are available at this price.26
REFERENCES
1. Fonarow GC1 French W J, Parsons LS et al for the National Registry of Myocardial Infarction 3 Participants: Use of Hpid-towering medications at discharge in patients with acute myocardial infarction: data from the National Registry of Myocardial Infarction 3. Circulation 2001;103: 38-44.
2. Paoletti R, Fahmy M, Mahla G, et al: Rosuvastatin demonstrates greater reduction in low-density lipoprotein cholesterol compared with pravastatin and simvasatin in hypercholesterolaemic patients: a randomized, double-blind study. J Cardiovasc Risk 2001;(8): 383-90.
3. Olsson AG, Pears J, McKellar J, et ah Effect of rosuvastatin low-density lipoprotein cholesterol in patients with hypercholesterolemia. Am J Cardiol 2001; 88: 504-58.
4. AstraZeneca Pharmaceuticals LP: Crestor (rosuvastatin calcium) prescriber's information 2003. Wilmington, DE.
5. Jones PH, Davidson MH, Stein EA et al for STELLAR Study Group: Comparison of the efficacy and safety of rosuvastatin versus atorvastatin, simvastatin, and pravastatin across doses (STELLAR Trial). Am J Cardiol 2003;92:152-60.
6. Olsson AG, Istad H, Luurila O, et al for Rosuvastatin Investigators Group: Effects of rosuvastatin compared over 52 weeks for treatment in patients with hypercholesterolemia. Am Heart J 2002;144:1044-51.
7. Rader DJ, Davidson MH, Caplan RJ, et al: Lipid and apolipoprotein ratios: Association with coronary artery disease and effects of rosuvastatin compared with atorvastatin, pravastatin, and simvastatin. Am J Cardiol 2003; 91(5A): 20C-24C.
8. McTaggart F, Buckett L, Davidson G et al: Preclinical and clinical pharmacology of rosuvastatin, a new 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor. Am J Cardiol 2001;87(5A):28B-32B.
9. Hansten PD, Horn JR: Cytochrome P-450 Isoenzymes: Substrates, Inhibitors, and Inducers. University of Washington, 1998.
10. LauWC,WaskellLA,WatkinsPBetal:Atorvastatin reduces the ability of clopidogrel to inhibit platelet aggregation: A new drug-drug interaction. Circulation 2003;107(1): 32-7.
11. Brashers VL: Alterations of cardiovascular function. In: McCance KL, Huether SE, (Eds). Pathophysiology 4th edition. St.Louis, MO: Mosby, 2002;980-1003.
12. Jorde LB: Genes, environment, and common diseases. In: McCance KL, Huether SE (Eds). Pathophysiology, 4th edition. St.Louis, MO: Mosby, 2002;159-61.
13. Hersberger M, von Eckardstein A: Low highdensity lipoprotein cholesterol: Physiologic background, clinical importance and drug treatment. Drugs 2003; 63 (18);1907-45.
14. NCEP-ATP III: Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486-97.
15. Kleeman R, Princen HM, Emcis JJ et al: Rosuvastatin reduces atherosclerosis development beyond and independent of its plasma cholesterol-lowering effect in apo-e 3-leiden transgcneic mice: Evidence for anti-inflammatory effects of rosuvastatin. Circulation 2003; 108 (11):1368-74.
16. Albert MA, Daniclson E, Rifai N, et al for PRINCE Investigators: Effect of statin therapy on C-reactivc protein levels: The pravastatin inflammation/CRP evaluation (PRINCE): A randomized trial and cohort study. JAMA 2001 ;286 (1): 64-70.
17. Kent SM, Flaherty PJ, Coyle LC et al: Effect of atorvastatin and pravastatin on serum C-reactive protein. Am Heart J 2003;145(2).
18. Ridker PM, Rifai N, Pfeffer MA et al: Long-term effects of pravastatin on plasma concentration of c-reactivc protein. Circulation 1999:100 (3): 230-5.
19. Ansell BJ, Watson KE, Weiss RE, et al: hsCRP and HDL effects of statins trial (CHEST): Rapid effect of statin therapy on c-reactive protein and high density lipoprotein levels: A clinical investigation. Heart Disease 2003;5(1):2-7.
20. Ridker PM, Rifai N, Clearfield M, et al for Air Force/Texas Coronary Atherosclerosis Prevention Study Investigators. Measurement of C-reactivc protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med 2001;344 (26):1959-65.
21. Krysiak R, Okopien B, Herman ZS: Effects of HMG-CoA reductase inhibitors on coagulation and fibrinolytic processes. Drugs 2003; 63(17): 1821-54.
22. Bellosta S, Ferri N, Bernini F et al: Non-lipid-related effects of statins. Ann Intern Med 2000; 32(3):164-76.
23. Schwartz GG, Olsson AG, Ezekowitz MD, et al for the Myocardial Ischemia Reduction with Aggressive Cholesterol-Lowering (MIRACL) Study Investigators. Effects of atorvastatin on early recurrent ischemie events in acute coronary syndromes: the MIRACL study; a randomized controlled trial. JAMA 2001;285: 1711-8.
24. Sever PS, Dahlof B, Poulter NR et al for the ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations. In:The AngloScandinavian Cardiac Outcomes Trial - Lipid Lowering Arm (ASCOT-LLA): A multicenter randomized controlled trial. Lancet 2003: 361:1149-58.
25. Pasternak RC, Sidney SC, Bairey-Merz CN et al: ACC/AHA/NHLBI Clinical Advisory on the use and safety of statins. J Am Col Cardiol 2002; 40: 567-572.
26. Drugstore.com. Available at http://www.drugstore.com/pharmacy/drugindex/rxsearch.asp?s earch-crestor. Retrieved February 9, 2004.
Katie A. Leonard, RN, BSN
Copyright Springhouse Corporation May 2004
Provided by ProQuest Information and Learning Company. All rights Reserved