Definition
Lead poisoning occurs when a person swallows or inhales lead in any form. The result can be damage to the brain, nerves, and many other parts of the body. Acute lead poisoning, which is relatively rare, occurs when a large amount of lead is taken into the body over a short period of time. Chronic lead poisoning, which is a common problem in children, occurs when small amounts of lead are taken in over a longer period.
Description
Lead can damage almost every system in the human body, and it can also cause high blood pressure (hypertension). It is particularly harmful to the developing brain of fetuses and young children. The higher the level of lead in a child's blood, and the longer this elevated level lasts, the greater the chance of ill effects. Over the long term, lead poisoning in a child can lead to learning disabilities, behavior problems, and even mental retardation. At very high levels, lead poisoning can cause seizures, coma, and even death.
About one out of every six children in the United States has a high level of lead in the blood, according to the Agency for Toxic Substances and Disease Registry. Many of these children are exposed to lead through peeling paint in older homes. Others are exposed through dust or soil that has been contaminated by old paint or past emissions of leaded gasoline. Since children between the ages of 12-36 months are apt to put things in their mouths, they are more likely than older children to take in lead. Pregnant women who come into contact with lead can pass it along to the fetus.
Over 80% of American homes built before 1978 have lead-based paint in them, according to the Centers for Disease Control and Prevention (CDC). The older the home, the more likely it is to contain lead paint, and the higher the concentration of lead in the paint is apt to be. Some homes also have lead in the water pipes or plumbing. People may have lead in the paint, dust, or soil around their homes or in their drinking water without knowing it, since lead can't be seen, smelled, or tasted. Because lead doesn't break down naturally, it can continue to cause problems until it is removed.
Causes & symptoms
Before scientists knew how harmful it could be, lead was widely used in paint, gasoline ,water pipes, and many other products. Today housepaint is almost lead-free, gasoline is unleaded, and household plumbing is no longer made with lead materials. Still, remnants of the old hazards remain. Following are some sources of lead exposure:
- Lead-based paint. This is the most common source of exposure to large amounts of lead among preschoolers. Children may eat paint chips from older homes that have fallen into disrepair. They may also chew on painted surfaces such as windowsills. In addition, paint may be disturbed during remodeling.
- Dust and soil. These can be contaminated with lead from old paint or past emissions of leaded gasoline. In addition, pollution from operating or abandoned industrial sites and smelters can find its way into the soil, resulting in soil contamination.
- Drinking water. Exposure may come from lead water pipes, found in many homes built before 1930. Even newer copper pipes may have lead solder. Also, some new homes have brass faucets and fittings that can leach lead.
- Jobs and hobbies. A number of activities can expose participants to lead. These include making pottery or stained glass, refinishing furniture, doing home repairs, and using indoor firing ranges. When adults take part in such activities, they may inadvertently expose children to lead residue that is on their clothing or on scrap materials.
- Food. Imported food cans often have lead solder. Also, lead is found in leaded crystal glassware and some imported or old ceramic dishes. In addition, food may be contaminated by lead in the water or soil.
- Folk medicines. Certain folk medicines (for example, alarcon, alkohl, azarcon, bali goli, coral, ghasard, greta, liga, pay-loo-ah, and rueda) and traditional cosmetics (kohl, for example) contain large amounts of lead.
Chronic lead poisoning
New evidence suggests that lead may be harmful to children even at low levels that were once thought to be safe, and the risk of damag erises as blood levels of lead increase. The symptoms of chronic lead poisoning take time to develop, however. Children can appear healthy despite having high levels of lead in their blood. Over time, though, problems such as the following may arise:
- Learning disabilities
- Hyperactivity
- Mental retardation
- Slowed growth
- Hearing loss
- Headaches.
Lead poisoning is also harmful to adults, in whom it can cause high blood pressure, digestive problems, nerve disorders, memory loss, and muscle and joint pain. In addition, it can lead to difficulties during pregnancy, as well as cause reproductive problems in both men and women.
Acute lead poisoning
Acute lead poisoning, while less common, shows up more quickly and can be fatal. Symptoms such as the following may occur:
- Severe abdominal pain
- Diarrhea
- Nausea and vomiting
- Weakness of the limbs
- Seizures
- Coma.
Diagnosis
A high level of lead in the blood can be detected with a simple blood test. In fact, testing is the only way to know for sure if children without symptoms have been exposed to lead, since they can appear healthy even as long-term damage occurs. The CDC recommends testing all children at 12 months of age and, if possible, again at 24 months. Testing should start at six months for children at risk for lead poisoning. Based on these test results and a child's risk factors, the doctor will then decide whether further testing is needed and how often. In some states, more frequent testing is required by law.
Children at risk
Children with an increased risk of lead poisoning include those who:
- Live in or regularly visit a house built before 1978 in which chipped or peeling paint is present.
- Live in or regularly visit a house that was built before 1978 where remodeling is planned or underway.
- Have a brother or sister, housemate, or playmate who has been diagnosed with lead poisoning.
- Live with an adult whose job or hobby involves exposure to lead.
- Live near an active lead smelter, battery-recycling plant, or other industry that can create lead pollution.
Adults at risk
Testing is also important for adults whose job or hobby puts the mat risk for lead poisoning. This includes people who take part in the following activities:
- Glazed pottery or stained glass making
- Furniture refinishing
- Home renovation
- Target shooting at indoor firing ranges
- Battery reclamation
- Precious metal refining
- Radiator repair
- Art restoration.
Treatment
The first step in treating lead poisoning is to avoid further contact with lead. For adults, this usually means making changes at work or in hobbies. For children, it means finding and removing sources of lead in the home. In most states, the public health department can help assess the home and identify lead sources.
If the problem is lead paint, a professional with special training should remove it. This is not a do-it-yourself project. Scraping or sanding lead paint creates large amounts of dust that can poison people in the home. This dust can stay around long after the work is completed. In addition, heating lead paint can release lead into the air. For these reasons, lead paint should only be removed by someone who knows how to do the job safely and has the equipment to clean up thoroughly. Occupants, especially children and pregnant women, should leave the home until the cleanup is finished.
Chelation therapy
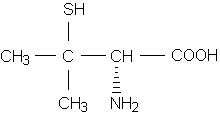
If blood levels of lead are high enough, the doctor may also prescribe chelation therapy. This refers to treatment with chemicals that bind to the lead and help the body pass it in urine at a faster rate. There are four chemical agents that may be used for this purpose, either alone or in combination. Edetate calcium disodium (EDTA calcium) and dimercaprol (BAL) are given through an intravenous line or in shots, while succimer (Chemet) and penicillamine (Cuprimine, Depen) are taken by mouth. (Although many doctors prescribe penicillamine for lead poisoning, this use of the drug has not been approved by the Food and Drug Administration.)
Alternative treatment
Changes in diet are no substitute for medical treatment. However, getting enough calcium, zinc, and protein may help reduce the amount of lead the body absorbs. Iron is also important, since people who are deficient in this nutrient absorb more lead. Garlic and thiamine, a B-complex vitamin, have been used to treat lead poisoning in animals. However, their usefulness in humans for this purpose has not been proved. Nutritional, botanical, and homeopathic medicines can be administered once the source is removed, to help correct any imbalances brought on by lead toxicity.
Prognosis
If acute lead poisoning reaches the stage of seizures and coma, there is a high risk of death. Even if the person survives, there is a good chance of permanent brain damage. The long-term effects of lower levels of lead can also be permanent and severe. However, if chronic lead poisoning is caught early, these negative effects can be limited by reducing future exposure to lead and getting proper medical treatment.
Prevention
Many cases of lead poisoning can be prevented. These steps can help:
- Keep the areas where children play as clean and dust-free as possible.
- Wash pacifiers and bottles when they fall to the floor, and wash stuffed animals and toys often.
- Make sure children wash their hands before meals and at bedtime.
- Mop floors and wipe windowsills and other chewable surfaces, such as cribs, twice a week with a solution of powdered dishwasher detergent in warm water.
- Plant bushes next to an older home with painted exterior walls to keep children at a distance.
- Plant grass or another ground cover in soil that is likely to be contaminated, such as soil around a home built before 1960 or located near a major highway.
- Have household tap water tested to find out if it contains lead.
- Use only water from the cold-water tap for drinking, cooking, and making baby formula, since hot water is likely to contain higher levels of lead.
- If the cold water hasn't been used for six hours or more, run it for several seconds, until it becomes as cold as it will get, before using it for drinking or cooking. The more time water has been sitting in the pipes, the more lead it may contain.
- If you work with lead in your job or hobby, change your clothes before you go home.
- Do not store food in open cans, especially imported cans.
- Do not store or serve food in pottery meant for decorative use.
Key Terms
- Chelation therapy
- Treatment with chemicals that bind to a poisonous metal and help the body pass it in urine at a faster rate.
- Dimercaprol (BAL)
- A chemical agent used to remove excess lead from the body.
- Edetate calcium disodium (EDTA calcium)
- A chemical agent used to remove excess lead from the body.
- Penicillamine (Cuprimine, Depen)
- A drug used to treat medical problems (such as excess copper in the body and rheumatoid arthritis) and to prevent kidney stones. It is also sometimes prescribed to remove excess lead from the body.
- Succimer (Chemet)
- A drug used to remove excess lead from the body.
Further Reading
For Your Information
Books
- Centers for Disease Control and Prevention. Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials. Atlanta, GA: CDC, 1997.
- Upton, Arthur C., and Eden Graber, eds. Staying Healthy in a Risky Environment: The New York University Medical Center Family Guide. New York: Simon & Schuster, 1993.
Periodicals
- Centers for Disease Control and Prevention. "Adult Blood Lead Epidemiology and Surveillance--United States, Second Quarter, 1995." Morbidity and Mortality Weekly Report 44(October 27, 1995): 801-803.
- Committee on Drugs, American Academy of Pediatrics. "Treatment Guidelines for Lead Exposure in Children." Pediatrics 96(July 1995): 155-160.
- Krucoff, Carol. "Lead Alert." Child (August 1996): 64-65, 67.
- Trachtenbarg, David E. "Getting the Lead Out." Postgraduate Medicine 99(March 1996): 201-202, 207-208, 211-214, 216, 218.
Organizations
- National Center for Environmental Health, Centers for Disease Control and Prevention. Mail Stop F-29, 4770 Buford Highway N.E., Atlanta, GA 30341-3724. (888) 232-6789. http://www.cdc.gov/nceh/ncehhome.htm.
- National Lead Information Center, National Safety Council. 1025 Connecticut Ave. N.W., Suite 1200, Washington, DC 20036. (800) LEAD-FYI (general information), (800) 424-LEAD (detailed information or questions). http://www.nsc.org/ehc/lead.htm.
- Office of Water Resources Center, Environmental Protection Agency. Mail Code (4100), Room 2615 East Tower Basement, 401 M St. S.W., Washington, DC 20460. (800) 426-4791. http://www.epa.gov/ow/.
Gale Encyclopedia of Medicine. Gale Research, 1999.