Editor:
Adrenal function is vital to life: without cortisol we die. This fact has been known since the 1930s when it was described by Banting and Best. Glucocorticoids are essential for maintaining carbohydrate, protein and fat metabolism. They also have a permissive effect which allows for glucagon and catecholamines to work. Important glucocorticoid effects include the normal functioning of the nervous system, water metabolism, vascular reactivity, regulation of circulating lymphocytes and the immune system and "resistance to stress." Complete lack of adrenal function is a disease state known as Addison's Disease. Conventional medicine only recognizes two states: you either make cortisol or you don't. Allopathic physicians are unaware of the decline in adrenal function as illness becomes chronic.
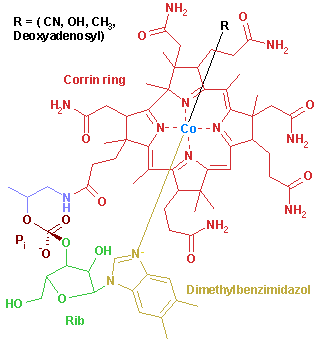
The etiology of adrenal fatigue begins with a "stressor," or in functional medicine terms, a "trigger." Triggers fall into several categories: psychosocial stress, environmental toxins (radon, mercury, mold), infectious organisms (fungal, bacterial, parasitic), food allergies (wheat, corn, sugar, milk), and other toxins (alcohol, drugs, prescription medications) to name a few. In addition, stressful events such as surgery or car accidents place a huge (usually unrecognized) load on the adrenal glands. The initial response to each of the above events is to elevate cortisol levels to help cope with the stress. However, over time, the adrenals become weakened and lose their circadian rhythm. This is due in large part to poor nutrition. All stressful events require increased amounts of several nutrients: vitamin C, pantothenic acid, B6 (pyridoxine), B12 (methylcobalamin), and folate. Interestingly, if the adrenal glands are catheterized and a "stressor" is introduced, the first chemical to leave the adrenals is not cortisol as one would suspect, but large amounts of vitamin C. These nutrients are severely lacking in the typical American diet or are not found in high enough amounts. More often than not "orthomolecular" dosing is necessary to correct the deficits.
The initial response to any stress is the hypersecretion of cortisol, but over time (approximately one year) there develops a negative feedback and a genuine "fatigue" causing reduced levels of DHEA-S and cortisol. The end result is an organism with reduced immunity, increased likelihood of autoimmune disease, heart attacks, elevated cholesterol and triglycerides, skin disorders, carbohydrate cravings, protein wasting, fatigue and depression (to name but a few). Physicians normally view these as separate events in a given organ and do not see that the symptoms represent a disease process (inflammation) that may occur in one or more organs simultaneously. Therefore everyone with any chronic disease, not just cardiovascular disease, should be screened using DHEA-S and a homocysteine level. As DHEA-S decreases, the level of homocysteine rises, with a concomitant decrease in most B-vitamins, but especially folate and B12. The currently accepted norms for these parameters are too permissive, reminiscent of glucose control in years past. All of our organs are linked and nothing that happens is random. We are all the result of our genetic interaction with our environment.
With the establishment of "disease" another pivotal biochemical event happens: abnormal methyl metabolism. Multiple reports in the recent literature link abnormal DNA methylation with the onset of cancer in laboratory animals. Undoubtedly this occurs in humans as well.
It is my clinical experience that as soon as a patient's DHEA-S falls to below 160 the ability to make methyl groups nosedives as well. These patients may then present with symptoms of depression (inability to synthesize S-adenosylmethionine), joint pain (inability to make methylsulfonylmethionine), and gastric acid reflux disease (inability to make betaine or trimethylglycine), to name a few. Not only does the ability to make methyl groups decrease, but the ability to convert to a methylated product is also compromised. For example, in chronically ill individuals the use of B12--as either the cyanocobalamin or the hydroxocobalamin form seems to do little to improve fatigue or mental functioning. The ideal compound to replenish B12 is methylcobalamin--the only active form. In each case, oral supplementation with the missing methyl-containing substrate ameliorates the symptoms. In each of the scenarios listed, the severity of the illness correlates with the level of the reduced or deficient DHEA-S and the concomitant elevated homocysteine level. The elevated homocysteine level is not only a marker for inflammation, but it is a marker for deficient B vitamins as well. The stage is now set for abnormal DNA methylation and the induction of cancer.
Efforts to repair adrenal fatigue include nutrients (in their most active form), glandular preparations, DHEA (and in severe cases cortisol itself), and lifestyle modifications with removal of triggers. Even with these measures, expect adrenal recovery to take 3 to 5 years.
Bibliography
Shealy, CN. Chronic Pain Management. TLfDP. 258:22-23, January 2005
Ganong. WF. Review of Physiology. McGrawh-Hill. 1999: pages 344-362
Poirer, LA. The effects of diet, genetics and chemicals on toxicity and aberrant DNA methylation: an introduction. J Nutr 2002 Aug: 132 (8 Suppi): 2336S-2339S
Shames, RL. Nutritional Management of Stress-Induced Dysfunction. ANSR-Applied Nutritional Science Reports. 2002
www.Dr.Lam.com: Adrenal Fatigue
Miller, AL. The Methionine-Homocysteine Cycle and Its Effects on Cognitive Diseases Alternative Medicine Review. Vol 8, number 1, page 7-13.
Susan Solomon, MD
12201 Gayton Road Suite 201
Richmond, Virginia 23238 USA
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group