Until recently, patients afflicted with certain malignant neoplasms and aggressive nonneoplastic conditions (eg, necrotizing systemic vasculitis, interstitial lung disease) had a poor prognosis and few therapeutic options. For example, patients with Wegener's granulomatosis had a mean survival of five months, and those with idiopathic pulmonary fibrosis (IPF) had a three- to four-year survival. Fauci and colleagues [1-3] presented a series of articles documenting improved survival with polyarteritis nodsa, lymphomatoid granulomatosis, and Wegener's granulomatosis using combination therapy with cyclophoshamide and prednisone. Gadek and Allen [4] extrapolated from the experience of Turner-Warwick and Haslam [5] to recommend combination therapy for some patients with IPF. Investigators reported few instances of serious or life-threatening toxicity, with primary concerns about hemorrhagic cystitis or development of second malignancies, [1] although recent reports document fatal infections and a variety of neoplasms associated with cytotoxic therapy. [6-7] During a 15-month period, we have observed four episodes of acute respiratory failure in patients receiving daily cyclophosphamide and prednisone. During the same period, nine patients received similar therapy without major complications.
CASE REPORTS
CASE 1
A 56-year-old woman presented with confusion, sinus congestion, and multiple cavitary pulmonary infiltrates. A nasal biopsy specimen demonstrated necrotizing granulomatous inflammation, consistent with Wegener's granulomatosis. She was placed on a regimen of prednisone and cyclophosphamide (150 mg) and had a dramatic clinical response with resolution of her confusion and diminution of her infiltrates. Her rheumatologist was unable to taper her prednisone dose below 20 mg at two months, and dyspnea, hypoxemia, and diffuse pulmonary infiltrates developed. An open lung biopsy specimen showed changes consistent with drug-induced lung disease and Pneumocystis carinii cysts, without a characteristic alveolar exudate. Despite ventilatory support and appropriate management, her infiltrates progressed and the patient died. No postmortem examination was done.
CASE 2
A 71-year-old man with a malignant thymoma diagnosed in 1981 was treated with radiation therapy. A malignant left pleural effusion developed in 1986 that remained stable with prednisone therapy. His dyspnea progressed in conjunction with the development of diffuse interstitial lung disease. An open lung biopsy specimen in June 1988 demonstrated bronchiolitis obliterans with organizing pneumonia. This failed to respond to 60 mg of prednisone a day after three months, and he was then placed on a regimen of cyclophosphamide (125 mg/day) with 30 mg of prednisone. Two months later, fever and diffuse infiltrates developed and he required mechanical ventilation. A transbronchial lung biopsy specimen demonstrated P carinii. Despite improvement with trimethoprim-sulfamethoxazole, he remained ventilator dependent for five months and subsequently died. No postmorten examination was performed.
CASE 3
A 60-year-old man presented with chronic cough, fever of unknown origin, and azotemia. A renal biopsy specimen showed necrotizing glomerulitis and (for presumptive polyarteritis nodosa) the patient was placed on a regimen of cyclophosphamide (150 mg) and prednisone (80 mg), which was tapered to 40 mg daily, limited by increasing azotemia. Within three months, diffuse pulmonary infiltrates, fever, and hypoxemia requiring mechanical ventilation developed. Bronchoalveolar lavage showed P carinii pneumonia (PCP). Renal failure and progressive lung disease developed in the patient despite trimethoprim-sulfamethoxazole and pentamidine therapy, and he died. No postmortem examination was obtained.
CASE 4
A 61-year-old man with a six-year history of chronic lymphocytic leukemia (CLL) with splenomegaly and red blood cell aplasia received cyclophosphamide (100 mg) and prednisone (40 mg) for six weeks. Fever, diffuse pulmonary infiltrates, and severe hypoxemia developed. A bronchoalveolar lavage demonstrated P carinii, and treatment with cyclophosphamide was discontinued. On the third hospital day, despite trimethoprim-sulfamethoxazole therapy, respiratory failure developed requiring mechanical ventilation. He ultimately recovered.
Data Analysis
A computerized search for all patients receiving oral cyclophosphamide and prednisone during a 15-month period was performed at the National Naval Medical Center pharmacy to establish patient use of cyclophosphamide and prednisone. We restricted our analysis of cyclophosphamide and prenisone pulmonary toxicity to those patients using outpatient (oral) therapy with these agents. We also reviewed the number of patients treated with prednisone without cyclophosphamide who had CLL, bronchiolitis obliterans, or systemic vasculitis during a similar time period. Statistical comparisons were generated using Student's t test for parametric statistics and Fisher's exact test for nonparametric statistics. This information is presented in Table 1.
RESULTS
Four of 13 patients had pulmonary complications
Table 1 -- Characteristics of Patients Receiving Cyclophosphamide and Prednisone and Relationship to Developing Respiratory Failure (*1)
develop, including PCP. Three of the nine patients without complications had myeloma, three had non-Hodgkin's lymphoma, and one each had breast cancer, Wegener's granulomatosis, and systemic lupus erythematosus. Patients in whom PCP developed had lower serum albumin levels and received daily doses of cyclophosphamide and prednisone. Three of the four patients in whom PCP developed had serum albumin levels less than 3.0 g/dl (30 g/L), while none of the intermittent cyclophosphamide and prednisone group had albumin levels less than 3.0 g/dl (30 g/dL) during the survey period (p = 0.018). Three of four patients with acute toxicity had less than 500 lymphocytes per cubic millimeter (by differential cell count), while the fourth had CLL. Relative proportions of lymphocytes were not determined. None of the patients who had development of respiratory failure had a total WBC count of less than 3,000/cu mm or total polymorpho-nuclear leukocytes of less than 1,500/cu mm. There was no significant difference in the mean age of the two groups. Among patients who had complications develop, cyclophosphamide doses ranged from 100 to 150 mg daily, with prednisone 20 to 40 mg daily at the time of complications. In the group without complications, cyclophosphamide was never used for more than five days per month, at a dose of 800 mg/day. Only two of the latter group were receiving "immunosuppressive" therapy, while seven received cancer chemotherapy with immunosuppression as a secondary effect. Sustained neutropenia was seen in neither group. During the specified time period, all patients who had PCP develop in our institution had either the acquired immunodeficiency syndrome (AIDS) or were receiving oral cyclophosphamide and prednisone. Four of six patients with CLL, systemic vasculitis, or bronchiolitis obliterans receiving oral cyclophosphamide and prednisone during this period had PCP develop, while none of 32 patients with the same conditions (CLL, 22 patients; bronchiolitis obliterans, five patients; vasculitis, five patients) receiving prednisone without cyclophosphamide had PCP develop (p = .0002). No patient with PCP in our institution between 1986 and 1990 has received prednisone alone.
DISCUSSION
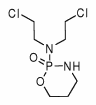
Progressive and ultimately fatal conditions such as cancer, necrotizing systemic vasculitis, and IPF justify some of the potential risk associated with immunosuppressive therapy. Cyclophosphamide reduces the circulating pool of mononuclear phagocytes producing both monocytopenia and lymphopenia. [8] Although a total peripheral lymphocyte count of less than 500/cu mm is associated with significant immunosuppression, infection risks are more closely associated with total granulocyte counts. [9] Pneumocystis carinii pneumonia has emerged as a frequent opportunistic pathogen in immunosuppressed patients, particularly those with AIDS. [10] Both cyclophosphamide and prednisone have been implicated as capable of producing immunosuppression contributing to the development of PCP, presumably related to T-cell dysfunction. [11] O'Donnell and associates [12] have shown greater suppression of neutrophil alveolitis in IPF with either cyclophosphamide or cyclophosphamide and prednisone than with prednisone alone. The quantitative effects of cyclophosphamide and prednisone on pulmonary cell-mediated immunity are less clear, although Hughes et al [13] established that the likelihood of PCP relates to the intensity of immunosuppression.
The contribution of cyclophosphamide and prednisone to impaired cell-mediated immunity is not new information, [14] although the frequency of complications varies. Pneumocystis carinii has previously been identified as a cause of respiratory morbidity in patients with lymphoma receiving combination chemotherapy. [15] Thirty of 39 patients without AIDS who had PCP develop were receiving both prednisone and cytotoxic therapy. [16] Three patients died of PCP among 44 fatalities with systemic lupus erythematosus in one series. [6] Twelve of 53 patients with PCP whose cases were reported by the Mayo Clinic were receiving steroids alone, while four were receiving cytotoxic therapy without steroids. [17] However, among 71 patients with polyarteritis nodsa and Churg-Strauss angiitis receiving cytotoxic therapy (including cyclophosphamide and prednisone in 45 patients), no cases of PCP are presented. [18] Individual cases of PCP may not be deemed "newsworthy" by physicians using immunosuppression, leading to possible case under-reporting. Our experience suggests that PCP is the principal early risk associated with daily oral cyclophosphamide and prednisone therapy. Cyclophosphamide pulmonary toxicity is an uncommon entity, a diagnosis of exclusion, and represents an idiosyncratic pulmonary reaction characterized by hyperplasia of type 2 pneumocytes. [19] Limited use of open lung biopsy and lack of reporting requirements of drug-induced lung disease may result in underdiagnosis and under-reporting of pulmonary drug toxicity. [20] Only one of our four patients developing acute respiratory failure had pulmonary drug toxicity from cyclophosphamide substantiated by open lung biopsy specimen.
The frequency with which pulmonary complications developed in our patients in conjunction with daily cyclophosphamide and prednisone therapy is unique. All patients had respiratory failure develop that required mechanical ventilation, and three eventually died. Two of the patients had underlying neoplasms, although neither CLL nor malignant thymoma are ordinarily associated with PCP. Our patients with CLL, vasculitis, and bronchiolitis obliterans treated with daily prednisone with or without intermittent alkylating agents have not had PCP develop. We believe this strongly implicates the daily administration of cyclophosphamide in the pathogenesis of PCP. Although defective antigen presentation in CLL may account for some defects in cell-mediated immunity (CMI), some defects in CMI are attributed to therapy. [21] The reduced serum albumin level seen in these patients, reflecting diminished visceral protein stores, may have contributed to immunosuppression and development of PCP. [22]
The treatment protocol of Fauci et al [1] for Wegener's granulomatosis included initiation of cyclophosphamide therapy at an oral dose of 2 mg/kg of body weight, continued for variable periods. Simultaneously, prednisone (1 mg/kg of body weight) was administered for two to four weeks until cyclophosphamide effects were noted. The prednisone dosage was then tapered over one to two months to an alternate-day regimen. [1] Leavitt and Fauci [23] have more recently noted that by the third month of therapy, "the patient should be maintained on 1 mg/kg of prednisone on alternate days." The duration (but not the doses) of daily cyclophosphamide and prednisone in the patients in whom we diagnosed PCP modestly exceeded Fauci's guidelines, because limited clinical responses to therapy prevented further prednisone tapering. None of the patients had development of PCP coincident with withdrawal of prednisone therapy. It is unknown whether strict adherence to the Fauci protocol would have prevented development of PCP. Only one of the patients (Case 1) had been recently hospitalized, making in-hospital acquisition of the agent unlikely. The patients had four different diagnoses and had received care from four different physicians, rendering systematic prescription or follow-up errors unlikely. The finding of severe lymphopenia in three of the four patients is a tantalizing explanation to account for the toxicity seen, and none of the four patients had either profound granulocytopenia or leukopenia. Severe lymphopenia (T4 cells <200/cu mm) has been associated with increasing frequency of PCP in several studies in patients with AIDS. [24,25]
Although we cannot fully explain the frequency of PCP with daily cyclophosphamide and prednisone therapy in our institution, we believe our experience provides convincing evidence that the combination of daily doses of cyclophosphamide and prednisone contributed to development of PCP. We believe the frequency and severity of complications suggests the following recommendations: (1) strong consideration of PCP in any patient receiving daily doses of cyclophosphamide and prednisone who has development of symptoms or signs of pulmonary infection; (2) consideration of prophylactic trimethoprim-sulfamethoxazole therapy in these patients; and (3) possibly limiting use of daily doses of cyclophosphamide/prednisone in IPF to patients with histologically proven disease who have not responded to initial prednisone therapy, until further prospective data substantiate a favorable change in the natural history of IPF with initial cytotoxic therapy. Serial monitoring of carbon monoxide diffusing capacity (Dco), which is generally reduced when PCP is diagnosed, [26] could potentially detect subclinical pulmonary function changes. Because the duration of symptoms with PCP associated with immunosuppressive diseases other than AIDS is short, [16] and previous frequency of PCP with cyclophosphamide and prednisone is low, the value of serial Dco determination is uncertain. Evaluation of quantitative measurements of cell-mediated immunity (eg, peripheral helper T cells, bronchoalveolar lavage, delayed hypersensitivity testing) and their correlation with "safe" and effective immunosuppression may establish better guidelines for "appropriate" immunosuppression. Although cyclophosphamide is sometimes considered a means to reduce steroid side effects, it carries a significantly different set of risks, both acute (hemorrhagic cystitis and opportunistic infection) and chronic toxicity (bladder carcinoma and hematologic malignancy), which may be either underreported or increasing in incidence.
REFERENCES
[1] Fauci AS, Haynes BF, Katz P, Wolff SM. Wegener's granulomatosis: prospective clinical and therapeutic experience with 85 patients for 21 years. Ann Intern Med 1983; 98:76-85
[2] Fauci AS, Haynes BF, Costa J, Katz P, Wolff SM. Lymphomatoid granulomatosis. N Engl J Med 1982; 306-68-74
[3] Fauci AS, Doppmann JL, Wolff SM. Cyclophosphamide-induced remissions in advanced polyarteritis nodosa. Am J Med 1978; 64:890
[4] Gadek JE, Allen JD. Update on the evaluation and treatment of idiopathic pulmonary fibrosis. Pulmonary Perspectives 1988; 5:1-4
[5] Turner-Warwick M, Haslam PL. The value of serial bronchoalveolar lavages in assessing the clinical progress of patients with cryptogenic fibrosing alveolitis. Am Rev Respir Dis 1987; 135:26-34
[6] Hellmann DB, Petri M, Whitting-O'Keefe Q. Fatal infections in systemic lupus erythematosus: the role of opportunistic organisms. Medicine 1987; 66:341-48
[7] Baker GL, Kahl LE, Zee BC, Stolzer BL, Agarwal AK, Medsger TA. Malignancy following treatment of rheumatoid arthritis with cyclophosphamide. Am J Med 1987; 83:1-9
[8] Dale DC, Fauci AS, Wolff SM. The effect of cyclophosphamide on leukocyte kinetics and susceptibility to infection in patients with Wegener's granulomatosis. Arthritis Rheum 1973; 16:657
[9] Cupps TR, Fauci AS. The vasculitides. Philadelphia: WB Saunders Co; 1981
[10] Levine SJ, White DA. Pneumocystis carinii. Clin Chest Med 1988; 9:395-423
[11] Frenkel JK, Good JT, Shultz JA. Latent pneumocystic infection in rats, relapse and chemotherapy. Lab Invest 1966; 15:1559
[12] O'Donnell K, Keogh B, Cantin A, Crystal RG. Pharmacologic suppression of the neutrophil component of the alveolitis in idiopathic pulmonary fibrosis. Am Rev Respir Dis 1987; 136:288-92
[13] Hughes WT, Feldman S, Aur JAR, Verzosa MS, Hustu HO, Simone JV. Intensity of immunosuppressive therapy and the incidence of Pneumocystis carinii pneumonitis. Cancer 1975; 36:2004-09
[14] Burke BA, Good RA. Pneumocystis carinii infection. Medicine 1973; 52:23-51
[15] Browne MJ, Hubbard SM, Longo DM, Fisher R, Wesley R, Ihde DC, et al. Excess prevalence of Pneumocystis carinii pneumonia in patients treated for lymphoma with combination chemotherapy. Ann Intern Med 1986; 104:338-44
[16] Kovacs JA, Hiemenz JW, Macher AM, Stover D, Murray HW, Shelhamer J, et al. Pneumocystis carinii pneumonia: a comparison between patients with the acquired immunodeficiency syndrome and patients with other immunodeficiencies. Ann Intern Med 1984; 100:663-71
[17] Peters SG, Prakash UBS. Pneumocystis carinii pneumonia. Am J Med 1987; 82:73-8
[18] Guillevin L, Du LTH, Godeau P, Jais P, Wechsler B. Clinical findings and prognosis of polyarteritis nodosa and Churg-Strauss angiitis: a study in 165 patients. Br J Rheumatol 1988; 27:258-64
[19] Cooper, JAD Jr, White DA, Matthay RA. Drug-induced pulmonary disease, I: cytotoxic drugs. Am Rev Respir Dis 1986; 133:321-40
[20] Rosenow EC. Drug-induced pulmonary disease. In: Murray J, Nadel J (eds): Textbook of respiratory medicine. Philadelphia: WB Saunders Co; 1988:1681-1702
[21] Chapel HM, Bunch C. Mechanism of infection in chronic lymphocytic leukemia. Semin Hematol 1987; 24:291-96
[22] Walzer PD, LaBine M, Redington TJ, Cushion MT. Predisposing factors in Pneumocystis carinii pneumonia: effects of tetracycline, protein malnutrition, and corticosteroids on hosts. Infect Immun 1984; 46:747
[23] LEavitt RY, Fauci AS. State of the art: pulmonary vasculitis. Am Rev Respir Dis 1986; 134:149-66
[24] Mittelman A, Wong G, Safai B, Myskowski P, Gold J, Koziner B. Analysis of T-cell subsets in different clinical subgroups of patients with the acquired immune deficiency syndrome. Am J Med 1985; 78:951-56
[25] Polk BF, Fox R, Bookmeyer R, Kanchanaraksa S, Kaslow R, Visscher B, et al. Predictors of the acquired immunodeficiency syndrome developing in a cohort of seropositive homosexual men. N Engl J Med 1987; 316:61-6
[25] Coleman DL, Dodek PM, Golden JA, Luce J, Golden E, Gold WM, et al. Correlation between serial pulmonary function tests and fiberoptic bronchoscopy in patients with Pneumocystis carinii pneumonia and the acquired immune deficiency syndrome. Am Rev Respir Dis 1984; 129:491-93
COPYRIGHT 1991 American College of Chest Physicians
COPYRIGHT 2004 Gale Group