A 57-year-old woman presented to a community hospital with complaints of headache and photophobia, cough, and nausea. Workup included a lumbar puncture to rule out meningitis. Spinal fluid analysis was unremarkable for infection or malignancy. Her initial CBC count showed a normal total WBC count, but the differential was noted to contain 75% fibroblasts. The patient was transferred to the hematology/oncology service at our hospital, where a bone marrow biopsy was performed. Within 24 h, progressive fevers, respiratory distress, and hypoxemia developed, and the patient was transferred to the ICU.
The medical history was significant for only migraine headaches. There were no known drug allergies. The medical and surgical histories otherwise were noncontributory. The patient was a lifelong nonsmoker, drank a glass of wine with dinner, and had no history of illicit drug use. Up to the time of hospitalization, she was working as a women's health physician and had no recent travel outside of the country.
Physical Examination
The patient's temperature was 101.3[degrees]F, systolic/ diastolic BP was 121/52 mm Hg, and pulse rate was 101 beats/min. Respiratory rate ranged from 22 to 40 breaths/min. Oxygen saturation was as low, at 60% on room air, but increased to 95% with a 100% nonrebreather mask. The neck was supple, without evidence of jugular venous distension. Sclera were nonicteric. Mucous membranes were moist and pink without evidence of mucosal hemorrhage. Lungs exhibited bibasilar rales. There were no rhonchi or wheezes. There was no dullness to percussion. Cardiac examination was unremarkable. The abdominal examination was normal; specifically, there was no hepatosplenomegaly. Extremities were without cyanosis, clubbing, or edema. Pulses were strong in all four extremities.
Laboratory Data
Laboratory data included WBC count of 16,100/ [micro]L; hemoglobin, 10.2 g/dL; platelets, 125,000. Manual differential showed 4% neutrophils, 44% lymphocytes, 28% monocytes, and 24% fibroblasts. Sermn chemistries and arterial blood gas revealed a nonanion gap metabolic acidosis, an albumin level of 2.1 mg/dL, and a total bilirubin level of 9.. 1 mg/dL, with a direct fraction of 0.9 mg/dL. On hospital day 3, the bone marrow aspiration revealed abundant fibroblasts, and flow cytometry showed these were consistent with acute monocytic leukemia (AML) [AML M5].
Radiographic Data
An initial chest radiograph showed bilateral alveolar infiltrates with lower-lobe predominance (Fig 1).
Clinical Course
Shortly after the patient arrived in our ICU, worsening respiratory distress and hypotension developed. Endotracheal intubation, mechanical ventilation, and IV fluids and vasopressors were required. CT of the thorax with IV contrast demonstrated dense bilateral lower-lobe airspace disease with air bronchograms, and bilateral small pleural effusions (Fig 2).
What was the diagnostic procedure? What was the cause of the hypoxemic respiratory failure?
The diagnostic procedure was BAL. The cause of the hypoxemic respiratory failure was pulmonary leukemic infiltration secondary to AML M5.
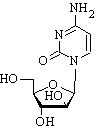
Following intubation, bronchoscopy was performed and BAL was obtained from the left lower lobe. The results of this showed 200 WBCs in the BAL fluid, 80% of which were fibroblast cells, and 30,000 RBCs. Monoblasts were present in the BAL preparation from the patient (Fig 3). These fibroblasts were similar in morphology to those present in the bone marrow aspirates and the peripheral blood from the patient. Flow cytometry showed that the fibroblasts were positive for monocytic markers (CD14 and CD13) and myelceytic markers (CD33). In addition, they showed aberrant expression of T-cell markers (CD4 and CD7), B-cell markers (CD24), and natural killer T-cell markers (CD56). This immunophenotype is similar to that seen in the peripheral blood fibroblasts. The aberrant expression of lymphoid markers on the monoeytic cells in the lung indicates the presence of a neoplastic cell population, consistent with the diagnosis of AML M5, with pulmonary inprovement. No organisms were cultured from the BAL fluid. The peripheral blood showed a 3.9% blast count with a total leukocyte count of 14,100/[micro]L on the same day the BAL was obtained. The patient was started on a course of chemotherapy consisting of cytarabine, etoposide, and danorubiein.
DISCUSSION
The differential diagnosis of the acute hypoxic respiratory failure included severe bacterial pneumonia, congestive heart failure, pulmonary hemorrhage, and pulmonary leukemic infiltration. Crampositive and Gram-negative infections are common in patients with AML because of impaired cell-mediated immunity that results from the immature and dysfunctional leukemic cells. Although the patient received broad-spectrum antibiotics, the patient never had positive Gram-stain or culture results for bacteria. The patient had no signs or history consistent with heart failure. Pulmonary hemorrhage does occur in this population of patients, yet the BAL finding was negative, and there was no decrease in hematocrit that would imply hemorrhage.
The reported incidence of leukemic pulmonary infiltrates at autopsy in patients who die of leukemia ranges from 24 to 64%. There are no distinctive radiographic findings, as the leukemic infiltrates can mimic consolidated pneumonia, ARDS, or heart failure. Interlobular septal thickening has been reported as a consistent finding on CT, but this is not specific to this entity alone. Nodular and ground-glass opacities also may manifest on CT. Additionally, diffuse reticular patterns have been described on chest radiography.
There are also few data on the pathogenesis or incidence of lung involvement with other forms of leukemia. As many as 17% of patients with chronic lymphocytic leukemia can acquire leukemic pulmonary infiltration. This is in comparison to other forms of AML, which are reported to have up to 10% lung involvement.
Premortem pathologic diagnosis of pulmonary leukemic infiltrates has generally been obtainable via flexible fiberoptic bronchoscopy. Although the cutoff ranges of fibroblasts recovered on bronchoalveolar specimens vary somewhat in the literature, this is one acceptable method of making the diagnosis. Transbronchial biopsies can also be helpful, especially when a BAL specimen may be skewed by alveolar hemorrhage. In 1990, Kovalski et al reported a series of patients in whom the peripheral blast count was > 40% at the time of pulmonary diagnosis, which was via transbronchial biopsies. This has been termed pulmonary leukostasis, as the high burden of peripheral leukocytes leads to trapping in the pulmonary circulation, with interstitial infiltrates and hypoxemia. However, Azoulay et al reported a series of 9.0 patients with confirmed AML M5 with respiratory status deterioration in which only 4 patients had peripheral fibroblast counts that fulfilled the criteria of Kovalski et al. The lowest reported peripheral leukocyte count in a patient with pulmonary leukemic infiltrates is 800/[micro]L, with zero fibroblasts.
There are no established clinical criteria to firmly exclude or include a diagnosis of leukemic pulmonary infiltrates, since their radiographic appearance mimics other conditions. A previous diagnosis of leukemia should raise the suspicion of this entity in a patient with pulmonary infiltrates and hypoxemia. Laboratory testing may be helpful if there is a high peripheral leukocyte or fibroblast burden. But, as our patient and other case reports highlight, there is no single low cutoff value for peripheral leukocyte or fibroblast counts that excludes this diagnosis.
Another striking feature of the patients in the series of Azoulay et al of AML with acute respiratory failure was that all of the patients experienced acute worsening of their respiratory status within hours of chemotherapy initiation. This has been termed acute lysis pneumopathy and is presumably pathologically related to the destruction of fibroblast cells in the pulmonary circulation. These cells release cytokines and cytotoxic enzymes, which promotes inflammation in the lungs, with subsequent airspace infiltration and hypoxia. Animal models have shown that monoeytic ceils have a predilection for the pulmonary circulation, probably as a result of monocyte-endothelium interaction. This likely explains the strong association between AML M5 pulmonary leukemic infiltrates and lysis pneumopathy, regardless of peripheral fibroblast counts.
The management for acute lysis pneumopathy is supportive care in an ICU setting. Mechanical ventilation, whether invasive or noninvasive, should be instituted promptly, along with other therapies aimed at stabilizing hemodynamics and organ function, such as vasopressors, IV fluid resuscitation, supportive blood product transfusions, renal replacement therapy if indicted, ensuring adequate nutrition and maintaining electrolyte homeostasis. Prompt recognition of and therapy directed toward the tumor lysis syndrome is also a crucial element of care in this patient population.
After aggressive ICU care with both noninvasive and invasive ventilation, only 50% of the patients died in the group of Azoulay et al. While seemingly high, this is superior to other published studies of patients with hematologic malignancies and respiratory failure requiring ICU care, in which the mortality rate is [greater than or equal to] 67%. It was postulated that aggressive care and support in the ICU was a reason for this survival benefit in this group. Much of the data on leukemic patient outcomes in the ICU come from literature that is > 15 years old. More outcome studies in modern ICUs are needed, as our methods of care and support have improved over the last 20 years.
For pulmonary and critical care physicians as well as oncologists, it is important to recognize leukemia patients at high risk for respiratory Failure. Prompt ICU monitoring and supportive care, including non invasive and invasive ventilation during initiation of chemotherapy, can improve survival in the subset of patients with AML M5.
Our patient's pulmonary status destabilized on initiation of chemotherapy, and she required prolonged mechanical ventilation and tracheostomy. She sustained several episodes of Gram-negative sepsis but ultimately was liberated from the ventilator and remained hemodynamically stable. Four weeks after induction chemotherapy was initiated, a repeat bronchoscopy was performed with BAL of the right upper and lower lobes to evaluate persistent infiltrate. No malignant cells were identified in the BAL fluid, and during the following week the infiltrates cleared. The patient was transferred to a medicine ward, from which she signed herself out the following week and was unavailable for follow-up.
CLINICAL PEARLS
1. Pulmonary leukemic infiltrates should be considered in the differential diagnosis of patients with acute leukemia who present with respiratory failure, regardless, of their peripheral leukocyte or fibroblast counts. Leukemic infiltrates have been documented with peripheral leukocyte counts' as low as 800/[micro]L and absence of fibroblasts.
2. AML M5 cells have a predilection for the pulmonary circulation and are the likely reason that this. form of leukemia commonly causes leukemic pulmonary infiltration.
3. Prompt bronchoscopy with BAL and transbronchial biopsies should be performed on all leukemic patients with respiratory failure to facilitate a diagnosis of leukemic pulmonary filtration.
4. Acute lysis pneumopathy, a clinical sequelae of tumor destruction by chemotherapy in which dying malignant cells' release cytokines and enzymes, causing pulmonary inflammation and tissue destruction, can lead to hypoxemic respiratory failure.
5. Aggressive ICU support, including the use of noninvasive and invasive ventilation, has decreased mortality in AML M5 patients with acute hypoxemic respiratory failure from leukemic infiltration and acute lysis pneumopathy.
SUGGESTED READINGS
Azoulay E, Alberti C, Bornstain C, et al. Improved survival in cancer patients requiring mechanical ventilatory support: impact of noninvasive ventilatory support. Crit Care Med 2001; 29:519-525
Azoulay E, Fieux F, Moreau D, et al. Acute monocytic leukemia presenting as acute respiratory failure. Am J Respir Crit Care Med 2003; 167:1329-1333
Breuer R, Lossos IS, Lafair JS, et al. Utility of bronchoalveolar lavage in the assessment of diffuse pulmonary infiltrates in non-AIDS immunocompromised patients. Respir Med 1990; 84:313-816
Depuydt PO, Benoit DD, Vandewoulde KH, et al. Outcome in noninvasively and invasively ventilated hematologic patients with acute respiratory failure. Chest 2004; 126:1299-1306
Heyneman LE, Johkoh T, Ward S, et al. Pulmonary leukemic infiltrates. AJR Am J Roentgenol 2000; 174:517-521
Kovalski R, Hansen-Flaschen J, Lodato RF, et al. Localized leukemie infiltrates: diagnosis by bronchoscopy and resulution with therapy. Chest 1990, 97:674-678
Kress JP, Christenson J. Pohlman AS, et al. Outcomes of critically ill cancer patients with pulmonary infiltrates, fever, and acute respiratory failure. Am J Respir Crit Care Med 1999; 160: 19,57-1961
Prakash UB, Divertic MB, Banks PM. Aggressive therapy in acute respiratory failure from leukemic pulmonary infiltrates. Chest 1979; 75:345-350
van Buchem MA, Hogendoorn PC, Levelt CN, et al. Development of pulmonary lenkostasis in experimental myelocytic leukemia in the Brown-Norway rat. Leukemia 1992; 6:142-149
* From the Departments of Pulmonary, Critical Care, and Sleep Medicine (Drs. Valentino and Roberts), Nephrology (Dr. Gelfand), and Pathology (Drs. Nava and Galwin), Georgetown University Hospital, Washington, DC.
Manuscript received April 5, 2005: revision accepted April 18, 2005.
Reproduction of tiffs article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/repfints.shtml).
Correspondence to: Dominic J. Valentino III, DO, Department of Pulmonary, Critical Care, and Sleep Medicine, Georgetown University Hospital, Washington, DC; e-mail: DJVDO@ mindspring.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group