INTRODUCTION: Granulocytic sarcoma is a mass of myeloid precursor cells that are extra-medullary in location. The masses of leukemia cells have also been called chloroma because of their green hue on exposure to air. They have been reported in many sites in the human body. We present a case of granulocytic sarcoma presenting as a single necrotic pulmonary mass.
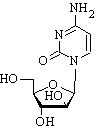
CASE PRESENTATION: A 39-year-old recently immigrated Jamaican male presented to an outside institution with three weeks of fever, chills, night sweats, weight loss, and productive sputum. The patient was a 25-pack-year smoker, and he also smoked marijuana and "crack" cocaine. He denied a history of active TB or TB exposure. He was noted to have a LUL lung cavity and left pleural effusion. At the outside institution he was diagnosed with AML and received treatment for community-acquired pneumonia with subsequent clinical improvement. The pleural fluid analysis for cytology was non-diagnostic. He was transferred to our hospital for further evaluation and treatment. Physical examination was unrevealing. An initial CT scan showed a moderate sized pericardial effusion, mediastinal adenopathy, and a left-upper lobe cavity at the left heart harder with a pleural effusion. Laboratory evaluation was significant for a white-blood cell count of 106,500 cells/mm3 with 65% blasts and hemoglobin of 7.4 g/dl. A bone marrow biopsy was consistent with a diagnosis of acute myelogenous leukemia. The patient underwent bronchoscopy that showed a mild amount of blood-tinged secretions from the left-upper lobe. Special stains of bronchial washings and lavage were negative for fungus and acid-fast bacilli. An endobronchial biopsy was unrevealing, and so a transthoracic needle biopsy was performed. The fungal and AFB stains were again negative, but cytology showed a mass of necrotic tissue with cells that were immunohistochemically consistent with myeloblasts. The patient was started on a seven-day induction chemotherapy protocol of Daunorubicin and Cytarabine. It was started thirteen days after transfer. The patient had transient bone marrow suppression but blasts were still present on recovery. Nevertheless, there was an improvement in the necrotic cavity and adenopathy seen on a subsequent CT scan about one month later.
DISCUSSIONS: Granulocytic sarcomas are associated with myeloproliferative disorders or leukemias. They have been reported both before and after the hematological diagnosis (l). Usually, there is known bone marrow involvement at the time of presentation and a clinical diagnosis is made. Immunohistochemical staining will reveal myeloperoxidase positivity though it is not universally present, and the tumor will share receptors with the myeloblasts in bone marrow. In this case, the patient was at risk for active TB and had supportive radiographs. Therefore, a definitive diagnosis had to be made before chemotherapy began. In a large case series, the most common sites were the soft tissue, bone, lymph nodes, and skin (2). Granulocytic sarcomas have been much less frequently noted in the thoracic cavity, and of those, the majority have solely involved the mediastinum or pleural space (3). There have been cases of these granulocytic sarcomas presenting as endobronchial tumors, multiple bilateral parenchymal nodules and interstitial infiltrates. (3-6).
CONCLUSION: A young male presented with constitutional symptoms and was found to have an abnormal chest radiograph and peripheral smear. The evaluation revealed AML with granulocytic sarcoma in the form of a necrotic lung nodule with mediastinal adenopathy and pleural effusion. Involvement of the lung is less common with granulocytic sarcoma, and this particular presentation is distinctly unusual.
REFERENCES:
(1) Menasce LP. Histopathology.1999 May;34(5):391-8.
(2) Neiman RS. Cancer. 1981 Sep 15;48(6):1426-37.
(3) Takasugi JE. J of Thorac Imaging. 1996 Summer;11(3): 223-30.
(4) Hicklin GA. Chest. 1988 Sep;94(3):655-6.
(5) Dugdale DC. Am Rev Respir Dis. 1987 Nov;136(5):1248-50.
(6) Lee DA. J Pediatr Hematol Oncol. 2004 July;26(7):431-434.
DISCLOSURE: Vivek Kaul, None.
Vivek Kaul MD * Joseph Cicenia MD Patricia Tietjen MD St. Vincent Catholic Medical Center, New York, NY
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group